Chapter 19
Putting the Examination Together
A physician is not only a scientist or a good technician. He must be more than that—he must have good human qualities. He has to have a personal understanding and sympathy for the suffering of human beings.
Albert Einstein (1879–1955)
The Techniques
The previous chapters dealt with the individual organ systems and the history and physical examinations related to each of them. The purpose of this chapter is to help the student assimilate each of the individual examinations into one complete and smoothly performed examination.
Ideally, a complete examination is performed in an orderly, thorough manner with as few movements as possible required of the patient. Most errors in performing a physical examination result from a lack of organization and thoroughness, not from a lack of knowledge. Evaluate each part of the examination carefully before moving on to the next part. The most common errors in performing the physical examination are related to the following:
Errors in technique are related to lack of order and organization during the examination, faulty equipment, and poor bedside etiquette. Errors of omission are common in examinations of the eye and nose; auscultation of the neck vessels, chest, and heart; palpation of the spleen; rectal and genital examinations; and the neurologic examination. Errors of detection are those in which the examiner fails to find abnormalities that are present. The most common errors of this type involve thyroid nodules, tracheal deviation, abnormal breath sounds, diastolic murmurs, hernias, and abnormalities of the extraocular muscles. Errors in interpretation of findings occur most commonly with tracheal deviation, venous pulses, systolic murmurs, fremitus changes, abdominal tenderness, liver size, eye findings, and reflexes. The most common types of recording errors are related to descriptions of heart size and murmurs, improper terminology, and obscure abbreviations.
In most situations, the hospitalized patient will be lying in bed when you arrive. After introducing yourself and documenting a complete history, you should inform the patient that you are ready to begin the physical examination. Always start by washing your hands.
The reader is advised now to watch the video presentation to review the complete physical examination of the man and the breast and pelvic examinations of the woman. The video will help you put the examination together.
Patient Lying Supine in Bed
General Appearance
Inspect the patient’s facial expression (see Chapters 10, The Chest; 11, The Heart; 14, The Abdomen; and 18, The Nervous System).
Have Patient Sit Up in Bed
Vital Signs
Check for orthostatic changes in left arm (see Chapter 11, The Heart).
Have Patient Turn and Sit with Legs Dangling off Side of Bed
Vital Signs
Eyes (Chapter 7, The Eye)
Nose (Chapter 8, The Ear and Nose)
Ears (Chapter 8, The Ear and Nose)
Mouth (Chapter 9, The Oral Cavity and Pharynx)
1. Inspect outer and inner surfaces of lips.
5. Observe Stensen’s and Wharton’s ducts, both sides.
9. Test hypoglossal nerve function (see Chapter 18, The Nervous System).
10. Palpate tongue.
13. Inspect tonsils, both sides.
14. Inspect posterior pharyngeal wall.
15. Observe uvula as patient says “Ah” (see Chapter 18, The Nervous System).
Neck (Chapter 6, The Head and Neck)
Neck Vessels (Chapter 11, The Heart)
Inspect height of jugular venous pulsation, right side.
Posterior Chest (Chapter 10, The Chest)
2. Palpate back for tenderness, both sides.
3. Evaluate chest excursion, both sides.
4. Palpate for tactile fremitus, both sides.
6. Evaluate diaphragmatic excursion, right side.
7. Auscultate back, both sides.
8. Palpate for costovertebral angle tenderness, both sides (see Chapter 14, The Abdomen).
Sacrum (Chapter 11, The Heart)
Test for edema.
Anterior Chest3 (Chapter 10, The Chest)
Female Breast (Chapter 13, The Breast)
Have Patient Lean Forward
Heart (Chapter 11, The Heart)
Auscultate with diaphragm at cardiac base.
Have Patient Lie Supine with Head of Bed Elevated Approximately 30 Degrees
Neck Vessels (Chapter 11, The Heart)
Breasts, Male and Female (Chapter 13, The Breast)
Have Patient Turn on Left Side
Heart (Chapter 11, The Heart)
Auscultate with bell at cardiac apex.
Have Patient Lie Supine with Bed Flat
Abdomen (Chapter 14, The Abdomen)
1. Inspect contour of abdomen.
4. Auscultate abdomen for bowel sounds, one quadrant.
5. Auscultate abdomen for bruits, both sides.
6. Palpate abdomen lightly, all quadrants.
7. Palpate abdomen deeply, all quadrants.
8. Percuss abdomen, all quadrants.
10. Percuss spleen.
11. Test superficial abdominal reflex (see Chapter 18, The Nervous System).
12. Check for rebound tenderness.
13. Check for hepatic tenderness.
14. Evaluate hepatojugular reflux (see Chapter 11, The Heart).
15. Palpate liver.
16. Palpate spleen.
17. Palpate aorta.
Pulses (Chapter 12, The Peripheral Vascular System)
1. Palpate radial pulse, both sides.
2. Palpate brachial pulse, both sides.
3. Palpate femoral pulse, both sides.
4. Palpate popliteal pulse, both sides.
5. Palpate dorsalis pedis pulse, both sides.
6. Palpate posterior tibial pulse, both sides.
7. Time radial and femoral pulses, right side.
8. Perform heel-to-knee test (part of neurologic examination; see Chapter 18, The Nervous System).
Have Male Patient Stand in Front of Seated Examiner
Male Genitalia (Chapter 15, Male Genitalia and Hernias)
Have Male Patient Turn around and Bend over Bed
Help Female Patient to Lithotomy Position
Female Genitalia (Chapter 16, Female Genitalia)
1. Inspect skin and hair distribution.
4. Inspect labia minora, clitoris, urethral meatus, and introitus.
5. Inspect area of Bartholin’s glands, both sides.
7. Test for pelvic relaxation.
8. Perform speculum examination.
12. Perform bimanual examination.
13. Palpate cervix and uterine body.
14. Palpate adnexa, both sides.
Have Patient Sit on Bed with Legs off Side
Mental Status
Ask routine questions (see Chapters 1, The Interviewer’s Questions; 18, The Nervous System; and 22, The Geriatric Patient).
Face (Chapter 18, The Nervous System)
Neck
Test range of motion (see Chapter 17, The Musculoskeletal System).
Hands and Wrists (Chapters 17, The Musculoskeletal System, and 18, The Nervous System)
1. Inspect hand and wrist, both sides.
2. Inspect nails, both sides (see Chapter 5, The Skin).
3. Palpate shoulder joint, both sides.
4. Palpate interphalangeal joints, both sides.
5. Palpate metacarpophalangeal joints, both sides.
6. Test light touch sensation, both sides.
7. Test vibration sense, both sides.
8. Test position sense, both sides.
9. Test object identification, both sides.
10. Test graphesthesia, both sides.
Elbows (Chapter 17, The Musculoskeletal System)
Shoulders (Chapter 17, The Musculoskeletal System)
Feet and Ankles (Chapters 17, The Musculoskeletal System, and 18, The Nervous System)
2. Test range of motion, both sides.
3. Palpate Achilles tendon, both sides.
4. Palpate metatarsophalangeal joints, both sides.
5. Palpate metatarsal heads, both sides.
6. Palpate ankle and foot joints, both sides.
7. Test light touch sensation, both sides.
8. Test vibration sense, both sides.
9. Test position sense, both sides.
10. Test lower extremity strength, both sides.
Have Patient Stand with Back to Examiner
The Written Physical Examination
After the examination has been completed, the examiner must be able to record objectively all the findings of inspection, palpation, percussion, and auscultation. Be precise in stating locations of abnormalities. Small drawings may be useful to describe a shape or location better. When describing the size of a finding, state the size in millimeters or centimeters rather than comparing it with a fruit or nut, for example, because these can vary greatly in size. It is best not to use most abbreviations because they may mean different things to different readers. However, the abbreviations used in the following examples are standard and may be used. Finally, do not make diagnostic statements in the write-up; save them for the summary at the end. For example, it is better to state that “a grade III/VI holosystolic murmur at the apex with radiation to the axilla” is present rather than “a murmur of mitral insufficiency” is heard.
Head: Normocephalic without evidence of trauma; no tenderness present.
Sinuses: No tenderness detected over frontal and maxillary sinuses.
Breasts: Mild gynecomastia, L > R; no masses or discharge present.
Heart: Point of maximum impulse, sixth intercostal space (PMI 6ICS) 2 cm lateral to midclavicular line (MCL); normal physiologic splitting present; no heaves or thrills are present; S1 and S2 distant; a grade II/VI high-pitched holodiastolic murmur is heard at the 2ICS at the right upper sternal border; a grade I/VI medium-pitched systolic crescendo-decrescendo murmur is heard in the aortic area; the systolic murmur is midpeaking (Fig. 19-1).
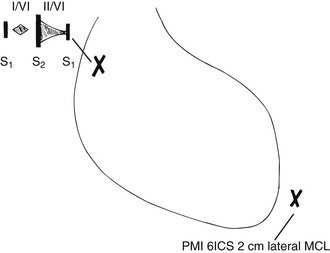
Figure 19–1 Location of cardiac physical signs.
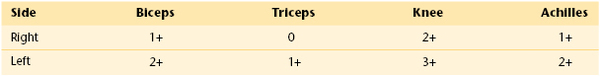
Neurologic: Oriented to person, place, and time; cranial nerves I to XII intact; gross sensory and motor strength intact; cerebellar function normal; plantar reflexes down; gait normal; deep tendon reflexes as shown in Table 19-1.
Summary: Mr. Henry is a 65-year-old man in no acute distress. Physical examination reveals systolic hypertension, retinal changes suggestive of sustained hypertension, a mild cataract in his right eye, a conductive hearing loss in his right ear, tonsillopharyngitis, and gynecomastia. Cardiac examination reveals aortic insufficiency. Peripheral vascular examination reveals possible atherosclerotic disease of the right carotid artery and mild venous disease of the lower extremities. The patient has a right, easily reducible inguinal hernia. A left-sided varicocele is present. Mild osteoarthritis of the hands is also present.
Head: Normocephalic without evidence of trauma; face appears edematous; no tenderness noted.
Nose: Straight without deviation; mucosa reddish-pink; inferior turbinates within normal limits.
Sinuses: No tenderness detected.
Breasts: Left mastectomy scar; right breast without masses, dimpling, or discharge.
Vascular: There are no bruits present over the carotid, renal, femoral, or abdominal arteries; the extremities are without clubbing or edema.
Pelvic: Deferred until patient more stable.
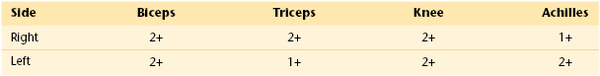
Neurologic: Oriented to person, place, and time; cranial nerves I to XII intact; gross sensory and motor strength intact; cerebellar function normal; plantar reflex down bilaterally; deep tendon reflexes as shown in Table 19-2.
The bibliography for this chapter is available at studentconsult.com.
Bibliography
Corbett EC, et al. Enhancing clinical skills education: University of Virginia School of Medicine’s Clerkship Clinical Skills Workshop Program. Acad Med. 2007;82:690.
DeMaria AN. Wither the cardiac physical examination? J Am Coll Cardiol. 2006;48:2156.
Fletcher FK, et al. The physical examination of patients with abdominal pain: the long-term effect of adding standardized patients and small-group feedback to a lecture presentation. Teach Learn Med. 2004;16:171.
Goldstein EA, et al. Promoting fundamental clinical skills: a competency-based college approach at the University of Washington. Acad Med. 2005;80:423.
March SK, Bedynek JL, Chizner MA. Teaching cardiac auscultation: effectiveness of a patient-centered teaching conference on improving cardiac auscultatory skills. Mayo Clin Proc. 2005;80:1443.
Ortiz-Neu C, et al. Error patterns of 3rd-year medical students on the cardiovascular physical examination. Teach Learn Med. 2001;13:161.
Vukanovic-Criley JM, et al. Competency in cardiac examination skills in medical students, trainees, physicians, and faculty: a multicenter study. Arch Intern Med. 2006;166:610.
Wiener S, Nathanson M. Physical examination: frequently observed errors. JAMA. 1976;236:852.
1 If the blood pressure is elevated in the upper extremity, blood pressure in the lower extremity must be assessed to exclude coarctation of the aorta. The patient is asked to lie prone, and blood pressure by auscultation is determined (see Chapter 11, The Heart).
2 The examiner should now go to the back of the patient while the patient remains seated with legs dangling off the side of the bed.
3 The examiner should now go to the front of the patient while the patient remains seated with legs dangling off the side of the bed.
4 This name is fictitious. Any similarity to any person living or dead with this name is purely coincidental.
5 This name is fictitious. Any similarity to any person living or dead with this name is purely coincidental.