Chapter 5 Pulse Oximetry, Capnography, and Blood Gas Analysis
Pulse oximetry
1 What is pulse oximetry and how does it work?
Capnography
6 What does the capnogram reveal about a patient’s condition?
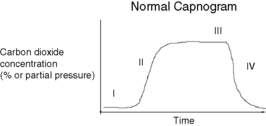
A capnograph provides a continuous display of the CO2 concentration of gases in the airways. A normal capnogram is shown in Figure 5-1. The CO2 partial pressure at the end of normal exhalation (phase III in the figure, end-tidal CO2 [PETCO2]) is a reflection of gas leaving alveoli and is an estimate of the alveolar CO2 partial pressure (PACO2). When ventilation and perfusion are well matched, the PACO2 approximates the arterial PCO2 (PaCO2), and thus PaCO2 equals PACO2 plus PETCO2. The presence of cyclical exhaled CO2 is useful in confirming airway patency, verifying endotracheal tube placement, and verifying the adequacy of pulmonary ventilation. In addition, decreases in cardiac output caused by hypovolemia or cardiac dysfunction result in decreased pulmonary perfusion. This causes an increased alveolar dead space, which dilutes PETCO2. Animal studies show that a 20% decrease in cardiac output causes a 15% decrease in PETCO2.
Arterial blood gases
9 What do arterial blood gas (ABG) instruments measure?
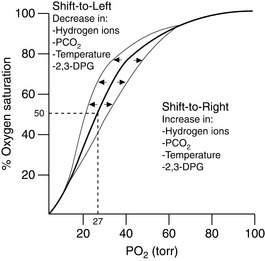
ABG instruments measure pH, PCO2, and PO2 using three separate electrodes. The blood gas samples are placed through an inlet into a temperature-controlled chamber (usually 37° C) where the blood is exposed to these three electrodes. The information from an ABG is essential in evaluating gas transport in blood, because the shape of the O2Hb dissociation curve depends on blood pH (Fig. 5-2).
12 Given that pulse oximetry is painless and accurate, why is ABG analysis even necessary?
1. A patient was noted to have oxygen desaturation via oximetry during a routine check after minor orthopedic surgery. The physicians evaluated this by ordering a chest radiograph, pulmonary function tests, and a ventilation-perfusion lung scan, the results of all of which were normal. Finally, ABG analysis was done and revealed alveolar hypoventilation alone with a normal A − aO2 gradient. The oxygen desaturation was simply the result of an increased PCO2 from hypoventilation in a patient receiving narcotics.
2. After an episode of smoke inhalation, a patient came to the emergency department because of headache and nausea. The oxygen saturation by oximetry was normal, and the patient was nearly dismissed after symptomatic treatment alone. Fortunately, recognizing the limitation of oximetry in differentiating oxygenated hemoglobin from CoHb, the physician drew an ABG sample, which revealed profound carbon monoxide poisoning. The patient was treated appropriately with 100% oxygen and close monitoring.
3. A patient with fever and sepsis had a respiratory rate of 40/min, and a chest radiograph revealed bilateral alveolar infiltrates. Oxygen was initiated, and with the use of pulse oximetry, the oxygen saturation was 90% after breathing 100% O2 by nonrebreathing mask. Unfortunately, the house officer did not draw an ABG sample and failed to realize that, with marked hyperventilation and respiratory alkalosis, the O2Hb dissociation curve is shifted to the left, thereby causing a much higher oxygen saturation for a given PaO2. Had ABG analysis been done at that time, it would have revealed pH 7.58, PACO2 22 mm Hg, PAO2 50 mm Hg, and O2 saturation 90%, all clearly indicating intubation and assisted ventilation with positive end-expiratory pressure.
Key Points Pulse Oximetry, Capnography, and Blood Gas Analysis
1. Pulse oximeter accuracy is strongly degraded by low perfusion states; accept only numeric estimates of saturation that are associated with clean perfusion signals.
2. Pulse oximeters may interpret dyes, skin pigment, and dyshemoglobinemia as alterations in hemoglobin-oxygen saturation.
3. The capnogram contains important information concerning airways disease and cardiopulmonary pathology.
1 Aoyagi T., Miyasaka K. The theory and applications of pulse spectrophotometry. Anesth Analg. 2002;94(1 Suppl):S93–S95.
2 Bickler P.E., Feiner J.R., Severinghaus J.W. Effects of skin pigmentation on pulse oximeter accuracy at low saturation. Anesthesiology. 2005;102:715–719.
3 Callaham M., Barton C. Prediction of outcome of cardiopulmonary resuscitation from end-tidal carbon dioxide concentration. Crit Care Med. 1990;18:358–362.
4 Feiner J.R., Bickler P.E. Improved accuracy of methemoglobin detection by pulse CO-oximetry during hypoxia. Anesth Analg. 2010;111:1160–1167.
5 Gravenstein J.S., Jaffe M.B., Paulus D.A. Capnography: Clinical Aspects. Cambridge, United Kingdom: Cambridge University Press, 2004.
6 Kugelman A., Wasserman Y., Mor F., et al. Reflectance pulse oximetry from core body in neonates and infants: comparison to arterial blood oxygen saturation and to transmission pulse oximetry. J Perinatol. 2004;24:366–371.
7 Robertson F.A., Hoffman G.M. Clinical evaluation of the effects of signal integrity and saturation on data availability and accuracy of Masimo SE and Nellcor N-395 oximeters in children. Anesth Analg. 2004;98:617–622.
8 Severinghaus J.W., Astraup P., Murray J.F. Blood gas analysis and critical care medicine. Am J Respir Crit Care Med. 1998;157:S114–S122.
9 Sorbini C.A., Grassi V., Solinas E., et al. Arterial oxygen tension in relation to age in healthy subjects. Respiration. 1968;25:3–13.