25 Pulmonary stenosis
Salient features
History
• Patients may be asymptomatic.
• Ask if there is a history of maternal rubella.
• Dyspnoea on exertion or fatigability may occur (when the stenosis is severe), less often, patients may have retrosternal chest pain or syncope with exertion. Eventually, right ventricular failure may develop, with resultant peripheral oedema and abdominal swelling.
• Cyanosis and clubbing (if the foramen ovale is patent, shunting of blood from the right to the left atrium may occur).
Examination
• Prominent ‘a’ wave in the JVP
• Ejection click, which decreases on inspiration (this is the only right sided sound that decreases with inspiration) (valvular stenosis) (Br Heart J 1951;13:519)
• Soft P2, with a wide split second sound
• Ejection systolic murmur in the left upper sternal border, best heard on inspiration. The murmur radiates to the left shoulder and left lung posteriorly. The more severe the stenosis, the longer is the murmur, obscuring the second aortic sound A2
• Then proceed by looking for central cyanosis and clubbing (Fallot’s tetralogy).
Advanced-level questions
How is the severity of pulmonary valve stenosis determined?
Mild: valve area larger than 1.0 cm2/m2, transvalvular gradient <50 mmHg or peak right ventricular systolic pressure <75 mmHg.
Moderate: valve area 0.5–1.0 cm2/m2, transvalvular gradient 50–80 mmHg or right ventricular systolic pressure 75–100 mmHg.
Severe: valve area <0.5 cm2/m2, transvalvular gradient >80 mmHg or right ventricular systolic pressure >100 mmHg.
How would you investigate this patient?
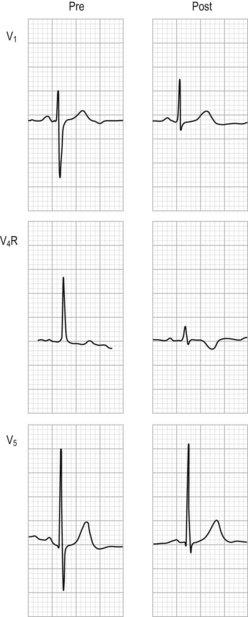
• Electrocardiogram shows right-axis deviation and right ventricular hypertrophy (Fig. 25.1).
• Chest radiograph shows a normal aortic knuckle whereas the pulmonary conus is either normal or enlarged (caused by post-stenotic dilatation of the main pulmonary artery) and the pulmonary vascular markings are diminished. The cardiac silhouette is usually normal in size or may be enlarged (when the patient has right ventricular failure or tricuspid regurgitation) (Fig. 25.2).
• Echocardiography can visualize the site of obstruction in most patients, but right ventricular hypertrophy and paradoxical septal motion during systole are evident. Doppler flow studies accurately assesses the severity of stenosis so that cardiac catheterization and angiography are usually unnecessary.
What are the complications of this condition?
Do you know of any eponymous syndromes linked to pulmonary stenosis?
• Noonan syndrome: short stature, ptosis, downward slanting eyes, wide-spaced eyes (hypertelorism), low-set ears, webbed neck, mental retardation and low posterior hairline. About two-thirds of patients with Noonan syndrome have pulmonary stenosis caused by valve dysplasia.
• Watson syndrome: café-au-lait spots, mental retardation and pulmonary stenosis.
• Williams syndrome: infantile hypercalcaemia, elfin facies and mental retardation, in addition to supravalvular pulmonary stenosis. Subvalvular pulmonary stenosis, which is caused by the narrowing of the right ventricular infundibulum or subinfundibulum, usually occurs in association with a ventricular septal defect.
How would you manage a patient with pulmonary stenosis?
• Mild valvular pulmonary stenosis: patients are usually asymptomatic and survival is excellent (with 94% still alive 20 years after diagnosis); therefore surgical correction is not required.
• Moderate pulmonary stenosis has an excellent prognosis with either medical or interventional therapy. Interventional therapy is usually recommended since most patients with moderate pulmonary stenosis eventually have symptoms requiring such therapy. Valve replacement is required if the leaflets are dysplastic or calcified or if marked regurgitation is present.
• Severe stenosis: relieve the the stenosis since only 40% of such patients do not require any intervention by 10 years after diagnosis.