Pulmonary Rehabilitation
I The following definition of pulmonary rehabilitation was drafted and adopted in 1999 by the American Thoracic Society:
II Pulmonary Rehabilitation Program
A Community assessment and planning before a program is started are crucial.
1. Assess the demographic profile of patients in the target community.
2. Evaluate medical (physician) interest and awareness.
B Assessment of program resources
1. Determine available versus needed space and equipment.
2. Identify clinical personnel desired versus personnel available.
C Alternatives in program structure
1. Inpatient pulmonary rehabilitation, which may include hospital, skilled nursing facility, or rehabilitation hospital
a. Individual or group education and breathing retraining are scheduled for the patient in a general acute care unit 5 to 7 days/week.
b. Individual low-level bedside or ambulatory exercise is instituted.
c. Patients may be prepared for follow-up evaluation in an outpatient rehabilitation setting.
d. Few are structured as comprehensive multidisciplinary 1- to 2-week inpatient programs because of reimbursement limitations, time constraints, and patient acuity.
e. Most commonly created to serve rehabilitation needs of patients with greatest acuity and complex long-term needs.
2. Outpatient pulmonary rehabilitation, conducted in outpatient hospital-based clinic, comprehensive outpatient rehabilitation facility (CORF), or extended care facility
a. These are the most common formats used for pulmonary rehabilitation.
b. Usually these programs involve two or five visits per week, but program lengths vary from 4 to 12 weeks, with 6 to 8 weeks the norm.
c. Individual or small group (two to five patients) exercise and educational sessions are instituted.
3. Outpatient office-based pulmonary rehabilitation
a. These programs may include some components of outpatient programs, such as education, breathing retraining, and exercise testing and prescription.
b. A pulmonary physician, pulmonary nurse specialist, and/or respiratory care practitioner usually implements the program.
4. Home-based pulmonary rehabilitation
a. These programs may include education, breathing retraining, and a simple exercise routine.
b. They may be included in the home care services of visiting nursing agencies or occasionally by the respiratory equipment providers.
c. They are generally less comprehensive in scope than hospital- or clinic-based programs, with visits often fewer than once per week.
d. They may be the only alternative for the homebound patient or when nearby hospitals do not have a pulmonary rehabilitation program.
e. Such programs may serve as a final rehabilitative transition from other more comprehensive and intensive program formats.
D Advantages and disadvantages of various pulmonary rehabilitation settings
1. Inpatient rehabilitation advantages
a. Reserved for the most acute patients with the greatest functional deficits, monitoring by professional staff is available 24 hr/day.
b. Allows staff to teach and observe family/patient interaction during therapies.
c. Best for patients requiring assistive devices, suctioning, tracheostomy care, or long-term ventilation.
2. Inpatient rehabilitation disadvantages
a. Most labor intensive and costly format
b. Transportation/availability of family members may be problematic.
3. Outpatient rehabilitation advantages
a. Most efficient use of professional staff
b. Typically greatest scope of professional staff is available.
c. Largest exposure (availability and accessibility) to target patient population
4. Outpatient rehabilitation disadvantages
a. Requires a certain base level of functional ability to access program
b. Transportation and availability of patient and/or family members may be issues.
c. External variables such as weather and pollution alerts may present barriers.
5. Home-based pulmonary rehabilitation advantages
a. Most convenient for patient and family
b. Transportation and availability of patient/family generally are nonissues.
c. Adaptation of exercises to a familiar environment may lead to greater compliance and offer identification by staff of home limits/barriers.
6. Home-based pulmonary rehabilitation disadvantages
a. Limited availability of sophisticated monitoring, testing, and exercise equipment
b. Most labor intensive, being one on one, and requires professional staff travel
c. The smallest scope of professional staff generally is available.
d. Usually the most questionably reimbursed rehabilitation format
E Multidisciplinary team approach
1. Clinicians from a variety of health care disciplines are necessary participants in a pulmonary rehabilitation program.
2. The number of contributing disciplines varies with the size, scope, availability, and setting of the pulmonary rehabilitation program.
3. If some or all of these disciplines are not available, a simple team composed of the physician and respiratory care practitioner, nurse, or physical therapist can provide thorough pulmonary rehabilitation in any of the previously mentioned settings.
4. Team members should have special interest or training in meeting the needs of patients with pulmonary disease.
5. Each team member should be qualified in their area of expertise to assess the patient’s needs, provide appropriate intervention, and monitor patient outcomes.
6. Each team member must be fully versed in their role and educational content, as well as completely aware of the role and content of each of the other disciplines represented.
7. All team members should be minimally trained in basic cardiac life support and ideally trained in advanced cardiac life support.
a. Are attended by all team members at regular intervals (e.g., weekly or monthly)
b. Provide a forum for initial goal setting, plan formation, and ongoing discussion of patients’ progress and discharge goals
c. Facilitate dissemination of general program information to team members (e.g., quality assurance findings, policy and procedure changes)
F Team members and their roles
a. A licensed physician with an interest in and knowledge of pulmonary rehabilitation, pulmonary function, and exercise evaluation
b. A pulmonary physician commonly fills this role.
c. Reviews and oversees all policies and procedures of the program
d. Reviews and oversees all billing and reimbursement practices
e. Participates in the initial screening of patients
(1) Reviews the medical history, medications, and diagnostic test results
f. Performs an educational and administrative role in advanced medical care planning/advanced directives
g. Represents the program to hospital administration, medical staff colleagues, and the community
h. May initiate, review, participate in, and evaluate pulmonary rehabilitation research
2. The program coordinator should be trained in a health-related profession and have demonstrated clinical experience and expertise in the care of patients with chronic pulmonary disease.
a. A respiratory care practitioner, registered nurse, or registered physical therapist commonly fills this role.
b. May serve a combined role as program coordinator and primary patient care provider/educator with responsibilities to
(1) Develop and revise program policies and procedures
(2) Implement and oversee daily program activities
(a) Assess weight, heart and breath sounds, respiratory and other symptoms, sleep, appetite, and adherence to home medication and exercise regimen at each patient visit
(3) Maintain written and verbal communication with each patient’s referring physician
(4) Participate in the development and implementation of program marketing plan
(5) Collect and report program quality assurance data
(6) Collect and report billing and reimbursement data
(7) Review current pulmonary rehabilitation literature and update protocols and equipment as indicated
(8) Represent the program to other hospital departments and to the community
c. Provides patient education on select topics
(1) Medications, with emphasis on indications, actions, side effects, drug interactions, and prescription compliance
(2) Respiratory anatomy and pathophysiology of chronic pulmonary disease
(3) Sequelae of chronic pulmonary disease
(4) Sleep disorders common to chronic pulmonary disease
(5) Description of medical procedures and test results used in pulmonary medicine
(6) Exercise testing, techniques, and conditioning
(7) Activities of daily living (ADLs)
(8) Breathing retraining, relaxation, and stress management techniques
(9) Oxygen therapy and bronchial hygiene techniques
(10) Functional self-management (e.g., self-assessment and management of symptoms, early intervention, and seeking medical attention)
d. Commonly participates in exercise testing
e. Performs assistance as needed with ADLs
f. Assesses the need for home care equipment/supplies and personnel
a. Evaluates nutritional status of patients
(3) Review of food record or calorie count
(4) Laboratory indices (e.g., total protein, albumin, cholesterol, phosphate, magnesium, transferrin, and calcium values)
(5) Anthropometric measurements (e.g., skinfold thickness, arm muscle circumference)
b. Recommends individual dietary modifications, including calories, components, supplements, and meal scheduling as indicated
a. Screens patients and families for evidence of psychosocial problems warranting referral or further treatment
b. Assesses and discusses with patients and families the impact of pulmonary disease on self-esteem, lifestyle, and relationships
c. Provides information on community resources to meet social, vocational, financial, transportation, and counseling needs
d. Assists physician and clergy in performing an educational and administrative role in advanced medical care planning/advanced directives
5. Psychologist or psychiatrist
a. Most often serves the pulmonary rehabilitation program on a consultant basis for select patients and families
b. Administers and interprets psychological tests
c. Conducts ongoing group or individual therapy
d. Recommends or prescribes psychotropic medications (e.g., anxiolytics, antidepressants, and sedative hypnotics)
a. Evaluates the impact of chronic pulmonary disease on the patient’s ability to perform ADLs and home maintenance, social, and vocational activities
b. Provides instruction and opportunities for practice in energy conservation and work simplification techniques
c. Recreational and leisure activity assessment and education
d. Includes instruction on coordinated breathing strategies
e. Recommends vocational alternatives or modifications for continued employment in the same setting
a. Serves as program coordinator and primary patient caregiver in some institutions
b. Teaches relaxation and biofeedback techniques
c. Provides consultation, treatment, and modified exercise recommendations for pulmonary rehabilitation patients with specific neuromusculoskeletal conditions
d. May design warm-up, strengthening, and toning exercise routines
a. Provides consultation to program staff on medication selections, actions, and interactions
b. May provide group education to patients and families on medications
a. Participates in exercise testing and prescription
b. May assist in conducting or monitoring group exercise sessions
a. May receive referrals as a consultant for patients and families with identified spiritual concerns
b. Provides spiritual counseling on issues such as death, dying, and quality of life, assisting physician and social worker in performing an educational and administrative role in advanced medical care planning/advanced directives
III Evaluation of the Pulmonary Rehabilitation Candidate
A Thorough screening of each patient is essential to the optimal planning and success of the individual treatment program.
B Pulmonary rehabilitation is indicated for patients with chronic respiratory impairment who, despite optimal medical management, remain dyspneic, have reduced exercise tolerance, or a restriction in activities. It is therefore not exclusionary on a disease-specific basis.
C The ideal candidate meets the following criteria.
1. Correctly diagnosed with symptomatic chronic pulmonary disease (most commonly chronic obstructive pulmonary disease [COPD]); however, with recent expansion to also include
g. Selected neuromuscular disease
h. Thoracic/abdominal surgical perioperative state
2. Willing and motivated to participate in the program
3. Free from concurrent medical problems precluding safe, successful program participation, such as
a. Recent myocardial infarction or ischemic heart disease
d. Severe pulmonary hypertension
e. Febrile or symptomatic infectious illness
f. Significant hepatic dysfunction
h. Recent gastrointestinal (GI) bleeding
i. Severe disabling neuromusculoskeletal condition
k. Psychiatric disorder or substance abuse, with significant impairment in concentration, motivation, judgment, or mood
l. Physical limitations secondary to poor eyesight, hearing, or orthopedic impairment may require modified techniques but should not represent a barrier to participation in pulmonary rehabilitative programs.
D The program medical director and primary patient caregiver (usually the program coordinator) should participate in the initial evaluation visit.
1. The patient should undergo a physical examination (see Chapter 18).
2. A patient and family medical history interview is conducted with assessment of the following
a. Respiratory symptoms: Onset, duration, severity, and ameliorating or aggravating factors
b. Family history of respiratory problems
c. Childhood respiratory health and illness
e. General medical and surgical history
f. Effects of pulmonary disease on quality of life
g. Exercise/activity abilities
h. Dependence versus independence in ADLs
i. Impairment in occupational performance
j. Current medications and schedule
k. History of psychosocial issues, such as depression and/or anxiety
l. Patient social support network
m. Use of assistive devices, such as cane, walker, or wheelchair
3. The goals and expectations of the patient and family are determined.
4. The program’s overall goals, activities, and expected benefits (Box 31-1), as well as limitations and risks, should be explained verbally and detailed on an informed written consent or program contract form.
E Preentry diagnostic tests should include
1. Complete pulmonary function test
a. To establish correct diagnosis and severity of lung disease
F Quantification of dyspnea is an essential component of evaluating the effectiveness of pulmonary rehabilitative efforts in patients. A number of reliable and valid tools exist to assess dyspnea in a given patient.
1. The Borg Scale for Breathlessness (BORG) uses a 10-point scale with a nonlinear scaling scheme with descriptive terms to pinpoint patient responses.
2. The visual analog scale (VAS) is a vertical or horizontal line with anchors to represent extremes of sensation. Patients physically mark the scale (commonly 100 cm long) during exercise to quantify their dyspnea.
3. The Baseline Dyspnea Index (BDI) is completed by an interviewer and measures three elements affected by dyspnea: functional impairment, magnitude of effort, and magnitude of task that provokes dyspnea.
4. The Transitional Dyspnea Index (TDI) is also completed by an interviewer comparing changes in dyspnea reported by the patient with BDI data.
5. The Chronic Respiratory Disease Questionnaire (CRQ) administered by an interviewer assesses dyspnea, fatigue, emotional function, and mastery of breathing.
6. The Pulmonary Functional Status and Dyspnea Questionnaire (PFSDQ) rates six categories: self-care, mobility, eating, home management, social, and recreational activities independently and in association with level of dyspnea.
7. The University of California, San Diego Shortness of Breath Questionnaire (SOBQ) assesses dyspnea on a six-point scale for each of 21 ADLs associated with varying exertional demands.
G A variety of reliable and valid tools can be used to assess psychological status, motivation, and several aspects of quality of life in patients with chronic pulmonary disease.
1. The St. George’s Respiratory Questionnaire (SGRQ) is a patient-completed quality of life questionnaire that assesses the three areas of illness, namely symptoms, activity, and impact on daily life.
2. The Medical Outcomes Study Short Form 36 (SF-36) consists of a 36-question questionnaire that assesses physical functioning, role functioning, bodily pain, general health, vitality, social functioning, and mental health.
3. The Minnesota Multiphasic Personality Inventory (MMPI) assesses 10 major dimensions of emotional distress and personality disturbance.
4. The Profile of Mood States (POMS) is a list of adjectives rated on a Likert-type scale to indicate recent mood.
5. The Katz Adjustment Scale (KAS) is composed of five subscales that focus on social adjustment, recreational activities, and general psychological disturbance.
6. The Sickness Impact Profile (SIP) measures the effect of illness on behavioral function in 12 areas of daily living, such as ambulation, home maintenance, social interaction, communication, alertness, and recreational pastime.
7. The Quality of Well-Being Scale (QWBS) is a subcomponent of the General Health Status index. The scaled score is derived based on symptom complexes and weighted functional level and indicates health-related life quality at one point in time.
8. The Eysenck Personality Inventory (EPI) is a simple instrument used to assess basic pertinent personality traits, such as extroversion and neuroticism.
9. The Additive Daily Activities Profile Test (ADAPT) is a self-administered test on which patients identify which of 105 activities (listed in order of descending estimated volume of oxygen utilization [ o2] requirement) they currently perform and which they have stopped because of respiratory limitations.
o2] requirement) they currently perform and which they have stopped because of respiratory limitations.
10. Rotter’s Locus of Control Scale evaluates the extent to which an individual perceives internal or external factors as responsible for outcomes and events in his or her life.
H Exercise testing in pulmonary rehabilitation should include
a. To diagnose the etiology of exercise limitation
(1) Rule out primary or concomitant cardiac disease (e.g., exercise-induced ischemia or dysrhythmias)
(2) Assess ventilatory response to exercise
b. To determine the functional capacity and severity of exercise impairment
(4) Uncontrolled hypertension (resting systolic pressure >190 mm Hg, diastolic pressure >120 mm Hg)
(5) Myocardial ischemic changes on electrocardiography (ECG) not attributable to medications
(6) Acute exacerbation of COPD
(7) Other acute medical illnesses (e.g., febrile condition, recent pulmonary embolism or thrombophlebitis, GI bleeding)
3. Patient safety and monitoring during exercise testing
a. Two experienced clinicians, including a physician and respiratory care practitioner, exercise physiologist, or cardiopulmonary diagnostic technician, conduct most exercise tests.
b. All persons should be certified in basic cardiac life support and ideally in advanced cardiac life support measures.
c. Emergency resuscitation equipment should be available.
d. Minimum requirements for noninvasive monitoring during exercise testing of the patient with chronic pulmonary disease include
(1) Patient’s physical appearance
(2) Perceived levels of dyspnea using a dyspneic rating tool (e.g., BORG)
(3) Blood pressure values, heart rate, and respiratory rate: Baseline, every 2 to 3 minutes, at the end of exercise, and 3 to 5 minutes after exercise
(5) Oxygen saturation: Baseline, continuous during exercise, and for 3 to 5 minutes after exercise
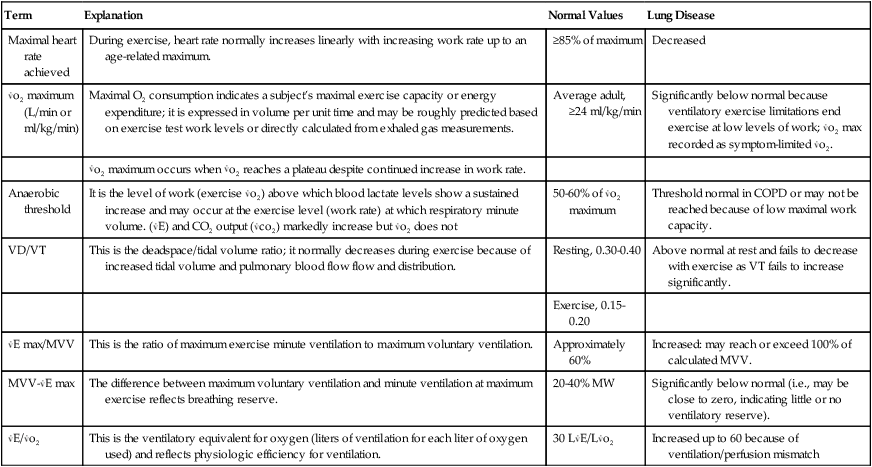
e. Derived additional exercise diagnostic measurements and information (Table 31-1); such data may not be available because of equipment, setting, and financial limitations of the program.
TABLE 31-1
Selected Exercise Test Information: Results in Health and in COPD
| Term | Explanation | Normal Values | Lung Disease |
| Maximal heart rate achieved | During exercise, heart rate normally increases linearly with increasing work rate up to an age-related maximum. | ≥85% of maximum | Decreased |
 o2 maximum (L/min or ml/kg/min) o2 maximum (L/min or ml/kg/min) |
Maximal O2 consumption indicates a subject’s maximal exercise capacity or energy expenditure; it is expressed in volume per unit time and may be roughly predicted based on exercise test work levels or directly calculated from exhaled gas measurements. | Average adult, ≥24 ml/kg/min | Significantly below normal because ventilatory exercise limitations end exercise at low levels of work;  o2 max recorded as symptom-limited o2 max recorded as symptom-limited  o2. o2. |
 o2 maximum occurs when o2 maximum occurs when  o2 reaches a plateau despite continued increase in work rate. o2 reaches a plateau despite continued increase in work rate. |
|||
| Anaerobic threshold | It is the level of work (exercise  o2) above which blood lactate levels show a sustained increase and may occur at the exercise level (work rate) at which respiratory minute volume. ( o2) above which blood lactate levels show a sustained increase and may occur at the exercise level (work rate) at which respiratory minute volume. ( E) and CO2 output ( E) and CO2 output ( co2) markedly increase but co2) markedly increase but  o2 does not o2 does not |
50-60% of  o2 maximum o2 maximum |
Threshold normal in COPD or may not be reached because of low maximal work capacity. |
| VD/VT | This is the deadspace/tidal volume ratio; it normally decreases during exercise because of increased tidal volume and pulmonary blood flow flow and distribution. | Resting, 0.30-0.40 | Above normal at rest and fails to decrease with exercise as VT fails to increase significantly. |
| Exercise, 0.15-0.20 | |||
 E max/MVV E max/MVV |
This is the ratio of maximum exercise minute ventilation to maximum voluntary ventilation. | Approximately 60% | Increased: may reach or exceed 100% of calculated MVV. |
MVV- E max E max |
The difference between maximum voluntary ventilation and minute ventilation at maximum exercise reflects breathing reserve. | 20-40% MW | Significantly below normal (i.e., may be close to zero, indicating little or no ventilatory reserve). |
 E/ E/ o2 o2 |
This is the ventilatory equivalent for oxygen (liters of ventilation for each liter of oxygen used) and reflects physiologic efficiency for ventilation. | 30 L E/L E/L o2 o2 |
Increased up to 60 because of ventilation/perfusion mismatch |
(1) Expiratory flow measurements, such as peak expiratory flow rate (PEFR), minute volume (Ve), and tidal volume (Vt), provide information regarding airflow limitation to exercise and the anaerobic threshold.
(2) Measurements of exhaled gases (breath by breath, end-tidal carbon dioxide and oxygen) allow calculation of the maximal oxygen consumption ( o2 max), respiratory quotient (RQ), and ventilatory equivalents for oxygen and carbon dioxide. These values indicate work efficiency and anaerobic threshold, as well as the physiologic efficiency for oxygen transport and the adequacy of ventilation during exercise.
o2 max), respiratory quotient (RQ), and ventilatory equivalents for oxygen and carbon dioxide. These values indicate work efficiency and anaerobic threshold, as well as the physiologic efficiency for oxygen transport and the adequacy of ventilation during exercise.
4. General exercise testing schemes
a. Constant time tests require exercise at the highest possible work rate for a given period.
b. Single-stage tests require exercise at a constant work rate for as long as possible; careful selection of the steady-state, submaximum exercise level is important to allow test completion in approximately 8 to 12 minutes.
c. In discontinuous tests, patients exercise at increasing work rates for constant periods with rests of 15 minutes to 24 hours between exercise periods.
d. Continuous incremental tests are used most commonly and use stages that are 1 to 3 minutes long. The increase in workload between each stage may vary, and a 3-minute stage is required for steady-state measurements.
a. The standard Bruce protocol consists of five 3-minute stages beginning at 1.7 miles/hr (mph) and 10% grade but has been modified for use in pulmonary patients by decreasing the starting grade and maximum speed. This protocol is used commonly in stress testing for cardiac disease.
b. The lower-level Naughton protocol begins at 0% grade and 1 or 2 mph and after seven 2-minute stages reaches the maximal level, 2.0 mph, 17.5% grade, or approximately a level of seven metabolic equivalents of the task, or 7 METs. The metabolic energy equivalent unit represents approximately 3.5 ml/kg of oxygen consumption at rest. Multiples of the MET unit are used to roughly indicate energy (oxygen consumption) required to perform various activities.
c. A variety of continuous cycle ergometer protocols are each designed with workload increments of equal size (usually 8 to 25 W) imposed every 30 seconds to 4 minutes (1 W equals 1 joule).
d. The 12-minute walking test requires that the patient cover as much distance as possible in a measured level corridor, resting only if necessary. At least two baseline measurements are recommended to account for a learning effect; through practice and pacing improvements subjects may show a significant increase in distance even before true training begins.
e. The 2- or 6-minute variation of the 12-minute walking test is useful for patients unable to complete the latter.
f. Many pulmonary rehabilitation teams design their own treadmill or cycle protocols; however, common to most are a work rate increment and intensity that achieve the symptom-limiting end point in 10 to 15 minutes.
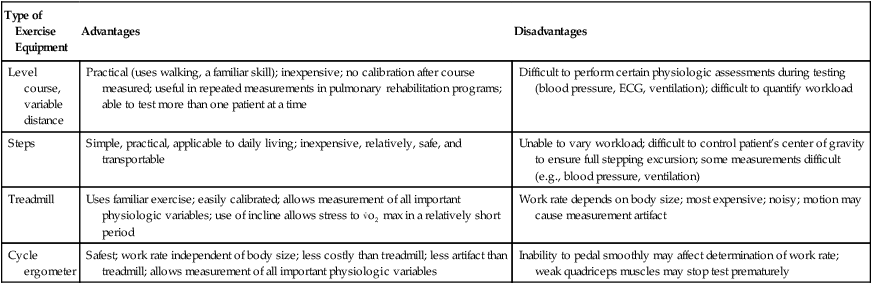
g. Advantages and disadvantages of common exercise testing equipment are highlighted in Table 31-2.
TABLE 31-2
Exercise Testing Equipment: Advantages Versus Disadvantages
| Type of Exercise Equipment | Advantages | Disadvantages |
| Level course, variable distance | Practical (uses walking, a familiar skill); inexpensive; no calibration after course measured; useful in repeated measurements in pulmonary rehabilitation programs; able to test more than one patient at a time | Difficult to perform certain physiologic assessments during testing (blood pressure, ECG, ventilation); difficult to quantify workload |
| Steps | Simple, practical, applicable to daily living; inexpensive, relatively, safe, and transportable | Unable to vary workload; difficult to control patient’s center of gravity to ensure full stepping excursion; some measurements difficult (e.g., blood pressure, ventilation) |
| Treadmill | Uses familiar exercise; easily calibrated; allows measurement of all important physiologic variables; use of incline allows stress to  o2 max in a relatively short period o2 max in a relatively short period |
Work rate depends on body size; most expensive; noisy; motion may cause measurement artifact |
| Cycle ergometer | Safest; work rate independent of body size; less costly than treadmill; less artifact than treadmill; allows measurement of all important physiologic variables | Inability to pedal smoothly may affect determination of work rate; weak quadriceps muscles may stop test prematurely |
A Components of an exercise prescription: Type of exercise, frequency, intensity, and duration
1. The type of exercise prescribed should parallel the desired outcome (the goals of training) as closely as possible and should be further determined by the patient’s abilities, preferences, and availability of equipment.
a. Aerobic exercise aims to improve cardiopulmonary fitness through sustained activity of large muscle groups at an intensity increasing the heart rate to a safe target range.
b. Strengthening exercises aim to improve the tone and function of select muscle groups. Isolated muscle movements are repeated 10 to 30 times often against resistance.
c. Most pulmonary rehabilitation programs emphasize lower extremity muscle training. However, many of the ADLs involve use of the arms; therefore, upper extremity muscle training should additionally be incorporated into the program.
2. Equipment and exercises commonly used in pulmonary rehabilitation include
3. The intensity of exercise is traditionally prescribed based on the heart rate or workload achieved on the baseline exercise test.
a. The initial target heart rate (THR) is 60% to 70% of the maximum age-predicted heart rate (males, 205 – one half their age; females, 220 – their age) unless it exceeds the maximum heart rate achieved during exercise testing.
b. The Karvonen method is an alternative means to calculate exercise THR.
(1) Maximum heart rate achieved on the exercise test (MHR) minus the resting heart rate (RHR) equals the heart rate range (HRR):
< ?xml:namespace prefix = "mml" />
 (1)
(1) (2)
(2)(2) In this equation 0.60 or 0.80 may be substituted to set the THR at lower or higher levels.
(3) Adding the product from equation 2 to the RHR will determine the THR:
 (3)
(3)4. Intensity of exercise may also be selected based on the exercise test workload (treadmill speed and grade or cycle load) corresponding to the following measurements.
5. Home or supervised exercise performed at any of these levels for 30 minutes three to four times per week generally will produce training effects in 4 to 6 weeks.
6. Some patients with chronic pulmonary disease may be unable to tolerate this traditional exercise-conditioning scheme; some may fail to achieve target heart rates, whereas others achieve high heart rates at relatively low levels of exercise.
a. Exercise schemes should be modified to each patient’s tolerance.
b. If necessary, begin with short exercise periods at a low intensity (e.g., 3 to 5 minutes walking or unloaded cycling) and aim to increase endurance before increasing the intensity of exercise.
7. Box 31-2 lists potential benefits from exercise reconditioning.
B Implementation of pulmonary rehabilitation exercise sessions
1. Patients are taught 10- or 15-second pulse taking.
2. Each session begins and ends with stretching and warm-up or cool-down exercises.
a. Rhythmic controlled breathing with head, neck, and shoulder exercises
b. Arm lifts (small 1- to 5-lb weights optional)
3. The following parameters are monitored.
a. Heart rate, blood pressure, and respiratory rate at rest, at the end of exercise, and 3 minutes after exercise
b. Oxygen saturation (Sao2) as needed
c. ECG rhythm as needed in patients with known (or at high risk for) cardiac arrhythmias using conventional lead or telemetry
4. The main exercise should be continuous and should involve large muscle groups of the upper and lower extremities.
5. Supplemental oxygen is given during exercise.
a. The use of supplemental oxygen during exercise is mandatory for patients who receive oxygen at rest.
b. Flow rate or FIO2 is titrated to achieve Sao2 of at least 90% with exercise.
c. It is indicated for patients not otherwise receiving oxygen if the Sao2 level decreases to <90% with exercise.
d. Traditionally it is provided via nasal cannula.
e. Portable oxygen should be used when warranted by the mobility demands of the exercise.
f. Oxygen-conserving systems (see Chapter 34) should always be used when the patient is using such a device at home for portability. Some of the devices may not provide adequate FIO2 with the increased minute ventilation resulting from exercise. Doing so provides documentation that oxygen requirements during exercise are or are not being met by the system, and changes should be made accordingly.
A Clinical assessment of ventilatory muscles
1. Maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP)
a. Measured during maximal static inspiratory or expiratory efforts into a mouthpiece connected to a pressure gauge
b. Indicate ventilatory muscle strength
c. Measured from near residual volume and total lung capacity, respectively
d. Normal values for MIP in those aged 20 to 54 years
e. Normal values for MEP in those aged 20 to 54 years
f. MIP and MEP measurements decrease with age, chronic pulmonary disease, neuromuscular conditions, and nutritional depletion.
a. Measured as the distance between percussed levels of dullness on full inspiration and full expiration
b. Normally approximately 3 to 5 cm
c. May be reduced in those with chronic pulmonary disease because of diaphragmatic weakness, severe hyperinflation, or both
1. Isocapneic hyperpnea: Rapid deep breathing into a circuit maintaining end-tidal carbon dioxide level within normal limits
a. Ventilatory muscle endurance training: Subject performs near-maximal breathing (rate and depth) for 15 to 30 minutes 3 to 5 days/week.
b. Sophisticated equipment and supervision are required to regulate FIO2 and prevent hyperventilation and respiratory alkalosis; thus it should not be performed at home or in any other unmonitored setting.
2. Inspiratory resistive breathing (IRB)
a. The variable-orifice, flow-dependent device has multiple openings ranging from 1.8 to 5.3 mm in diameter.
b. With the spring-load, flow-independent device, the patient must generate a prescribed threshold pressure to open a vent and allow inspiration.
c. Optimal candidates and protocols for IRB are not firmly established.
(1) One should begin with inspiratory resistive load corresponding to 30% of the MIP, or the smallest orifice tolerated, and monitor the Sao2 and respiratory rate.
(2) Frequency and duration are 10 to 15 minutes once or twice daily for 4 to 8 weeks, and then the resistance or threshold pressure is increased gradually to 60% to 70% of the MIP.
C Reported benefits of ventilatory muscle training
1. Increased inspiratory muscle strength (MIP)
2. Increased inspiratory muscle endurance (SIP, MSVC)
4. Increased exercise performance
5. Improved ability to perform ADLs
6. There is conflicting scientific evidence supporting the routine use of ventilatory muscle training as an essential component of pulmonary rehabilitation. However, it is reserved for individual consideration in select patients with COPD who have decreased ventilatory muscle strength and dyspnea.
VI Patient and Family Education
A Major objectives of patient education in pulmonary rehabilitation
1. Identifying and explaining the physical and psychosocial changes related to chronic pulmonary disease to set realistic individual goals
2. Identifying and developing skills in self-care techniques for optimal symptom management and overall health maintenance
B Factors that influence learning
2. Motivation and perceived need to learn
4. Patient-professional relationship (learner-educator relationship)
C Teaching techniques used in pulmonary rehabilitation programs
1. Lecture or panel presentation to group
2. Individualized patient and/or family education sessions
3. Demonstration of skills, practice, and return demonstration
5. Reading or written assignments
7. Normal anatomy and pathology posters
D Content of pulmonary rehabilitation education as modified from the AARC Clinical Practice Guidelines on Pulmonary Rehabilitation
1. Respiratory anatomy and physiology and pathophysiology of the specific chronic pulmonary disease
a. Upper and lower airway structures
b. Respiratory muscles and the act of breathing
c. Anatomic and functional changes in chronic pulmonary disease
d. Diagnostic tests and expected findings
f. Common complications of chronic pulmonary disease (e.g., infection, cor pulmonale)
(1) Diaphragmatic breathing is generally not recommended; however, it may have application in a non-COPD patient population.
(2) Pursed lip breathing with prolonged controlled exhalation
b. Use of breathing retraining techniques at rest, during exercise, and with daily activities
a. Causes and effects of stress
b. Techniques for stress reduction and relaxation
(1) Jacobsen’s progressive relaxation technique: Selected muscle groups are consciously relaxed in a systematic manner. The patient tenses and then relaxes muscles from head to toe, including face, neck, shoulders, arms, back, abdomen, legs, and feet.
(2) Guided imagery: The coach (nurse, therapist, or family member) uses descriptive statements to aid the patient in visualizing relaxing scenes.
(3) Biofeedback: Instrumentation is used to provide patients with signals regarding their control of select physiologic functions, such as respiratory rate and muscle tension.
(5) Simple body positioning and controlled breathing
5. Energy conservation in ADLs
7. Smoking cessation: Importance and methods available
a. Behavior modification techniques (e.g., desensitization, gradual reduction, and stimulus control)
b. Individual counseling or psychotherapy
c. Group smoking-cessation clinics
e. Cognitive approach (e.g., medical information, physician order)
8. Oxygen therapy (see Chapters 33 and 34)
a. Indications and expected benefit
b. Use/prescription (dose, hours, adjustment with sleep and exercise)
11. Sexuality and lung disease
12. Sleep abnormalities commonly associated with chronic pulmonary disease
13. Advanced medical care planning/advanced directives
b. Avoidance of settings with high density of respiratory infections
d. Cleaning and disinfecting home respiratory equipment
e. Prompt access of medical attention with symptom occurrence
1. Help patients accept their condition and realistically assess strengths and limitations.
2. Identify specific strategies to enlist for coping with stress, anxiety, and depression.
VIII Program Evaluation and Quality Assurance
A Program activities and goals should be monitored regularly in quality assurance audits (e.g., monthly or quarterly).
B Sample criteria include assessment of subjective and objective elements of pulmonary rehabilitation.
1. Patient satisfaction assessments (postprogram interviews or questionnaires)
2. Survey of patient’s perceived achievement of goals
3. Preprogram and postprogram comparison of
b. Exercise (tolerance) testing data
c. Indicators of quality of life, including reduction in dyspnea
d. Frequency of respiratory symptoms (e.g., cough, sputum production, wheezing)
4. Program attrition rates and reasons
5. Preprogram and postprogram hospitalization days and need to access other medical services
IX Postprogram Patient Follow-up Evaluation
A A summary letter is sent from the program coordinator to the primary or referring physician detailing the patient’s goals, progress, and achievements.
B The patient is encouraged to continue ongoing physician office visits for periodic medical assessment and regulation of medications.
C Many outpatient pulmonary rehabilitation programs offer reevaluation visits at 3-, 6-, and 12-month intervals to assess and reinforce compliance with home exercise and activity plans and to provide remediation as warranted.
D Ongoing education, support, and contact among patients are available through groups such as Better Breathers Clubs or other local lung association groups.
E Home respiratory equipment providers commonly participate in patient follow-up evaluation through written or verbal reports to program coordinators and physicians.
F Long-range follow-up evaluation is warranted to evaluate adherence, progression of underlying disease and comorbidity, hospitalization, and survival rates.

 o2 max
o2 max