Chapter 220 Puerperal Infection
INTRODUCTION
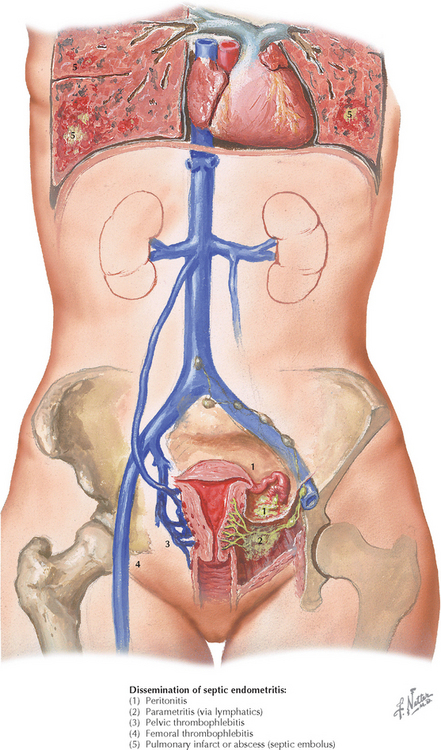
ETIOLOGY AND PATHOGENESIS
DIAGNOSTIC APPROACH
Differential Diagnosis
Workup and Evaluation
MANAGEMENT AND THERAPY
Nonpharmacologic
Drug(s) of Choice
FOLLOW-UP
Livingston JC, Llata E, Rinehart E, et al. Gentamicin and clindamycin therapy in postpartum endometritis: the efficacy of daily dosing versus dosing every 8 hours. Am J Obstet Gynecol. 2003;188:149.
Chongsomchai C, Lumbiganon P, Laopaiboon M. Prophylactic antibiotics for manual removal of retained placenta in vaginal birth. Cochrane Database Syst Rev. 2006. CD004904.
French LM, Smaill FM. Antibiotic regimens for endometritis after delivery. Cochrane Database Syst Rev. 2004. CD001067.
Hopkins L, Smaill F. Antibiotic regimens for management of intra-amniotic infection. Cochrane Database Syst Rev. 2002. CD003254.
Liabsuetrakul T, Choobun T, Peeyananjarassri K, Islam M. Antibiotic prophylaxis for operative vaginal delivery. Cochrane Database Syst Rev. 2004. CD004455.
Lumbiganon P, Thinkhamrop J, Thinkhamrop B, Tolosa JE. Vaginal chlorhexidine during labour for preventing maternal and neonatal infections (excluding Group B Streptococcal and HIV). Cochrane Database Syst Rev. 2004. CD004070.
Smaill F, Hofmeyr GJ. Antibiotic prophylaxis for cesarean section. Cochrane Database Syst Rev. 2002. CD000933.
American College of Obstetricians and Gynecologists. Prevention of early-onset group B streptococcal disease in newborns. ACOG Committee Opinion 279. Obstet Gynecol. 2002;100:1405.
American College of Obstetricians and Gynecologists. Prophylactic antibiotics in labor and delivery. ACOG Practice Bulletin 47. Obstet Gynecol. 2003;102:875.
American College of Obstetricians and Gynecologists. Premature rupture of membranes. ACOG Practice Bulletin 80. Obstet Gynecol. 2007;109:1007.
Casey BM, Cox SM. Chorioamnionitis and endometritis. Infect Dis Clin North Am. 1997;11:203.
Faro S. Postpartum endometritis. Clin Perinatol. 2005;32:803.
Maharaj D. Puerperal pyrexia: a review. Part I. Obstet Gynecol Surv. 2007;62:393.
Maharaj D. Puerperal pyrexia: a review. Part II. Obstet Gynecol Surv. 2007;62:400.