Pubovaginal Slings for the Correction of Stress Incontinence
Pubovaginal slings are well-accepted procedures utilized for the correction of stress incontinence. Materials utilized for pubovaginal slings are always biologic and are placed at the proximal urethra and bladder neck. Currently used biologic materials are divided into autologous tissue, which is harvested from the patient who is undergoing the sling; allograft material, which is most commonly cadaveric fascia lata; and xenografts, which are harvested from various animal sources. Technically, bladder neck slings are called pubovaginal slings when the arms of the material used are connected to the anterior rectus fascia on each side. Various modifications of a traditional pubovaginal sling have been described and involve various patch-type slings in which the sling materials are placed vaginally at the level of the proximal urethra and then are attached to sutures that are passed suprapubically. Proximal suburethral slings work best when bladder neck mobility and vaginal pliability are present. Although plenty of data are available to support the use of pubovaginal slings as a primary operation, these procedures are usually reserved for patients who have failed synthetic midurethral slings, or who have a contraindication for the use of a synthetic material.
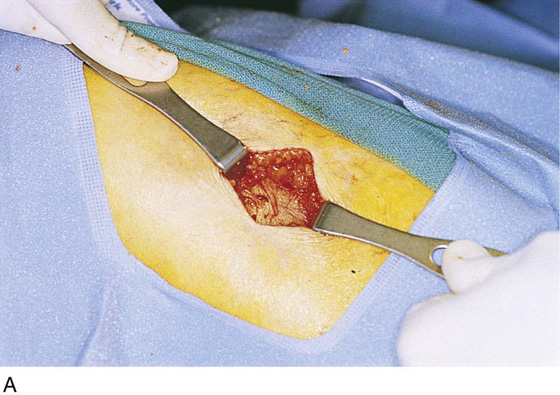
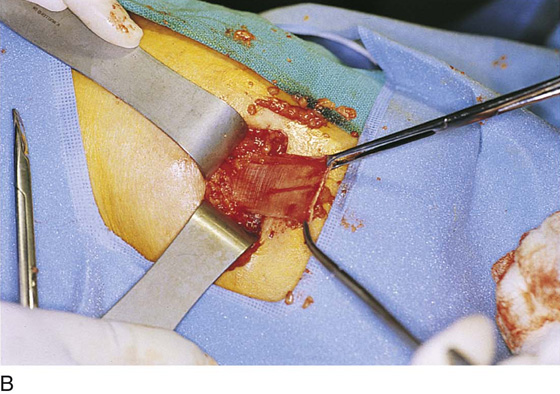
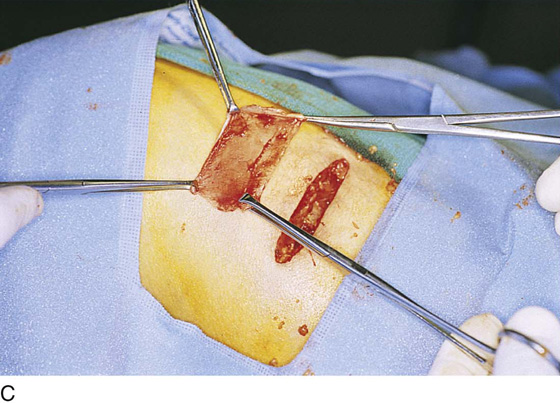
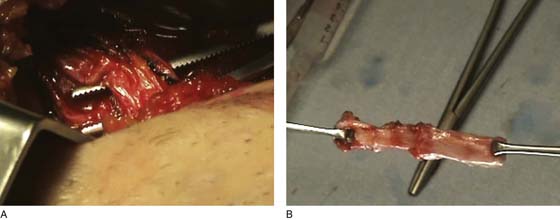
If the surgeon decides to utilize autologous tissue, this will most commonly be fascia lata or rectus fascia. Harvesting of these tissues usually will occur before any vaginal dissection is performed. The technique used to harvest fascia lata is determined by whether the surgeon prefers to do a complete pubovaginal sling, in which the fascia will need to extend from the anterior abdominal fascia to below the proximal urethra and back to the anterior abdominal fascia on the opposite side, or if the surgeon prefers to place a patch-type sling. If a patch-type sling is used, a patch of rectus fascia or fascia lata is harvested. To harvest a patch of fascia lata, a 3- to 4-cm transverse skin incision is made about 8 cm above the midpatella lateral to the knee and the lower thigh. Blunt dissection exposes the underlying fascia lata. A 4 × 6-cm piece of fascia lata is removed and will serve as the patch for the sling procedure (Figs. 59–1 and 59–2). Subcutaneous tissue is reapproximated, the skin is closed, and a pressure bandage is placed. If a full pubovaginal sling is to be utilized, then a long piece of fascia lata can be obtained by using a Wilson or Crawford fascial stripper. The technique used to obtain a full strip of fascia involves a similar incision as described with the patch technique; however, fat is bluntly dissected away from the fascia lata, all the way up the lateral side of the leg toward the greater trochanter. A 1-cm-wide piece of fascia is then removed with the fascial stripper. This usually will produce a 20-cm-long piece of fascia. A second piece of fascia lata of similar length can be obtained by repeating the same procedure. A 1-cm-wide bridge of fascia lata should remain between the two areas where the stripper has removed the tissue (Fig. 59–3). These two pieces of fascia can then be sutured to each other, thus providing a 30- to 35-cm-long piece of fascia for use in providing the pubovaginal sling. If the rectus fascia is used for a pubovaginal sling, a transverse abdominal incision is made, usually 4 cm above the pubic symphysis. Blunt dissection is performed until the underlying rectus fascia is identified. Via a transverse incision in the fascia, a 1- to 2-cm-wide strip of fascia is sharply dissected away. If the goal is to have the arms extend to the anterior abdominal wall, then a 20-cm-long piece of fascia is harvested (Fig. 59–4). If a patch sling is to be placed, then a 2 × 8 piece of fascia is harvested.
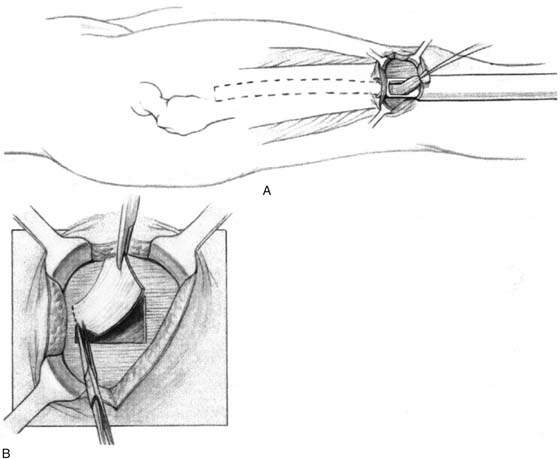
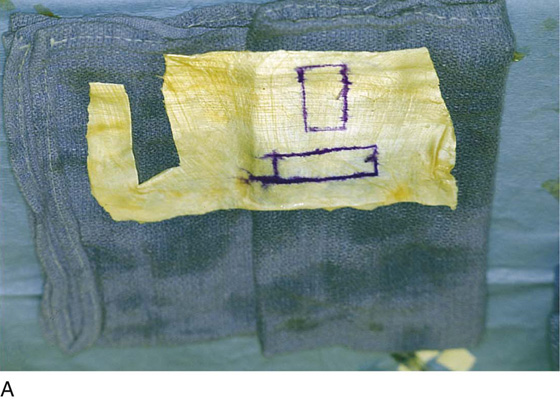
FIGURE 59–1 A. Technique for obtaining a strip of fascia lata using a vein stripper. B. Technique for obtaining a patch of fascia lata. Fascia lata patch has been excised.
FIGURE 59–2 A. An incision on the lower leg is made about 8 cm above the midpatella lateral to the knee, exposing fascia lata. B. A patch of fascia is being excised. C. A fascia lata patch has been excised.
FIGURE 59–3 A. Appropriate positioning of the leg for obtaining a full-length fascia lata strip. B. Exposure of a 1-cm-wide piece of fascia lata. C. Initial mobilization of a 1-cm fascial strip. D. Stripper is applied to the fascia lata to complete fascial stripping. E. Full-length strip of fascia lata. (Photographs A–D compliments of Dr Alfred Bent.)
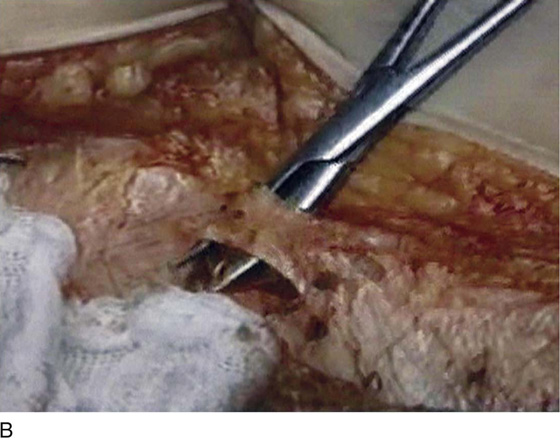
FIGURE 59–4 A. Rectus fascia has been exposed via a low transverse skin incision. B. A 1-cm-wide piece of fascia lata is exposed at the midline. C. Full-length piece of rectus fascia has been completely excised. (Photographs compliments of Dr Jerry Blaivas.)
Operative Details
1. The patient is placed in high stirrups in the dorsal lithotomy position, and the vagina and lower abdomen are appropriately prepped and draped. Preoperative antibiotics are usually given on call to the operating room.
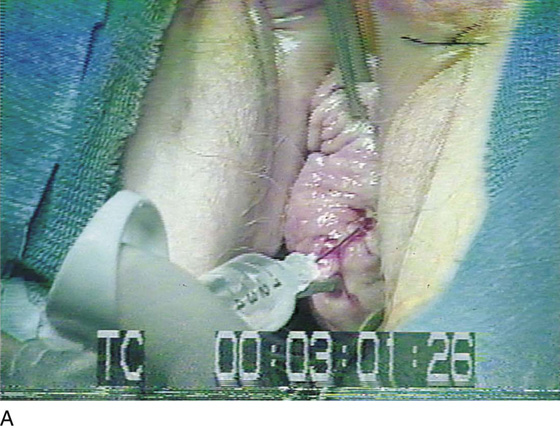
2. Hydrodissection of the anterior vaginal wall is usually utilized by injecting beneath the epithelium of the anterior vaginal wall at the level of the bladder neck (Fig. 59–5A). This facilitates dissection of the appropriate plane and also may have a hemostatic effect.
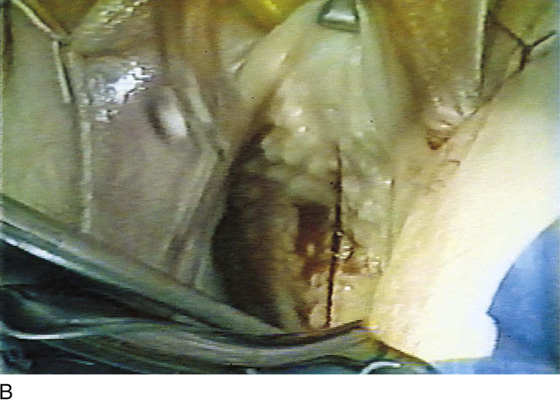
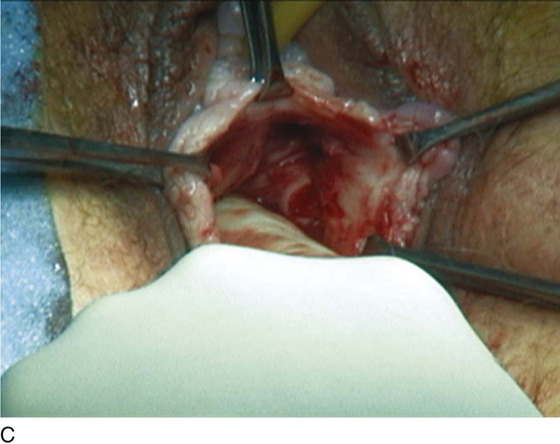
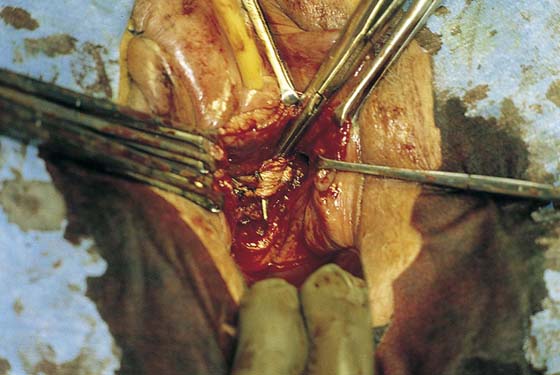
3. A midline vaginal incision or an inverted-U vaginal incision is made at the level of the proximal urethra or bladder neck (Fig. 59–5B). This is easily determined by palpation of the anterior vaginal wall with a Foley catheter in place. The vaginal epithelium is carefully dissected off the underlying periurethral and perivesical fascia with the use of blunt and sharp dissection. This dissection is extended bilaterally to the inferior lateral aspect of the pubic rami (Fig. 59–5C).
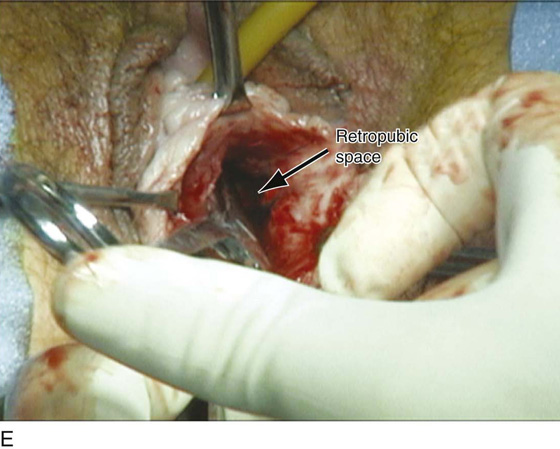
4. The retropubic space is then entered via blunt or sharp dissection (Fig. 59–5D, E). Once the periurethral attachment of the urethra has been penetrated on each side, one should be able to pass a finger along the back side of the pubic bone all the way to the inferior aspect of the rectus muscle.
5. If a traditional pubovaginal sling procedure is to be performed, an abdominal incision is made. This is usually made approximately two fingerbreadths, or 4 cm, above the level of the pubic symphysis and is a transverse incision usually no longer than 8 cm. The incision is extended down to the rectus fascia.
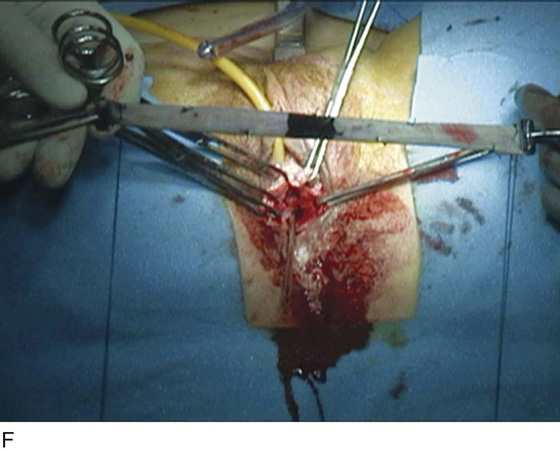
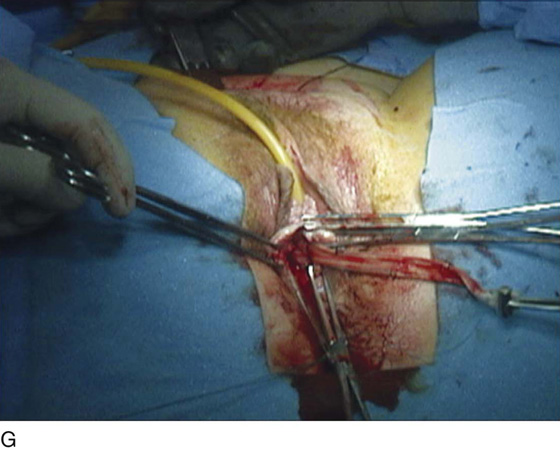
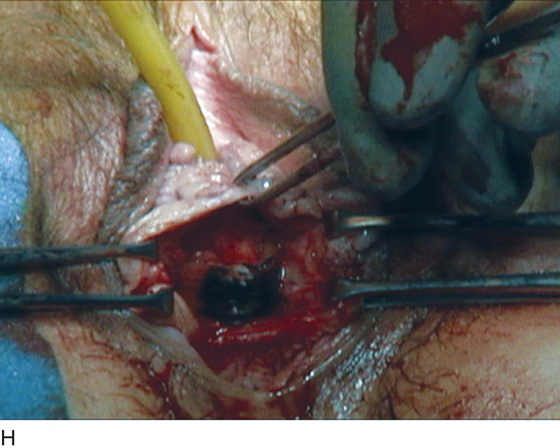
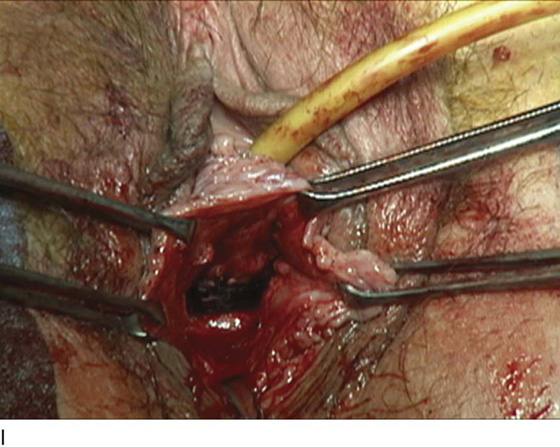
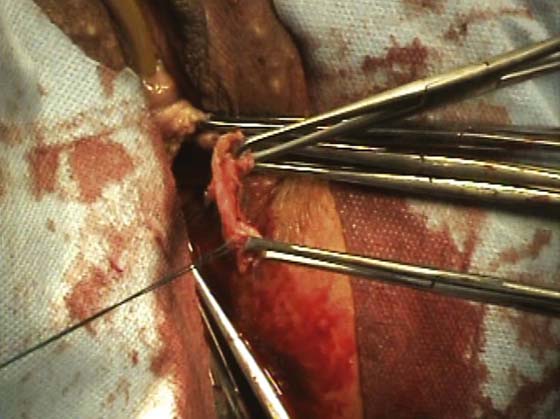
FIGURE 59–5 A. Hydrodissection of the anterior vaginal wall to facilitate dissection in the appropriate plane. B. A midline anterior vaginal wall incision is made that extends from the level of the proximal urethra to the level of the bladder base. C. The anterior vaginal wall has been opened up, and the dissection has been extended on the left side to the inferior pubic ramus. D. The index finger is now placed in the plane of dissection, and blunt dissection is utilized to penetrate the urogenital diaphragm and enter the retropubic space. E. The retropubic space has been entered sharply on the patient’s left side with the use of Mayo scissors. The scissors are directed toward the ipsilateral shoulder and are maintained in direct contact with the inferior pubic ramus. Once the urogenital diaphragm has been penetrated, the scissors are spread to complete the dissection. F. The sling material is brought into the field. It has been attached to a suture on each side, which will facilitate passage of it into the suprapubic incision. The area has been darkened at the midportion of the sling because this area sits under the proximal urethra. G. One arm of the sling has been passed into the suprapubic incision, and a Pereyra needle ligature carrier has been passed on the right side; the sutures from the other end of the sling have been passed through the eye of the ligature carrier. H. The sling is in place at the level of the proximal urethra and bladder neck. I. The arms of slings have been tied suprapubically, and the sling is resting loosely at the level of the proximal urethra and bladder.
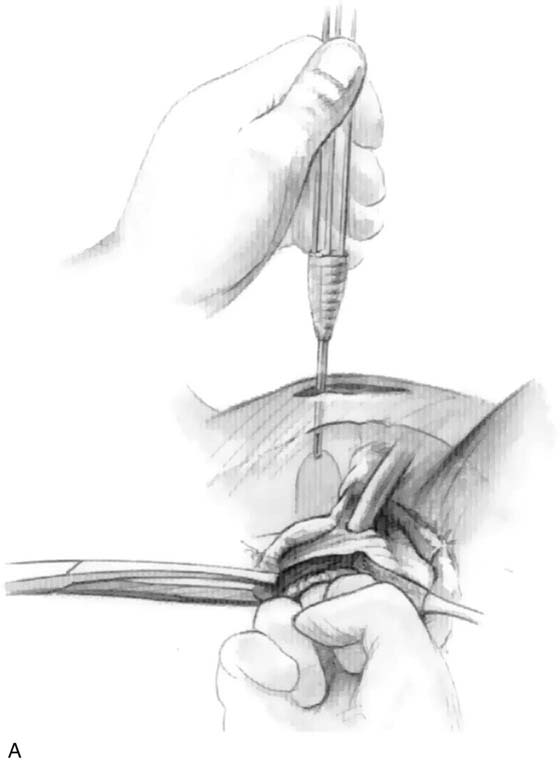
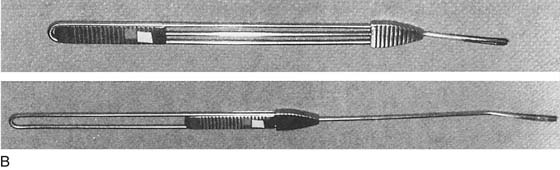
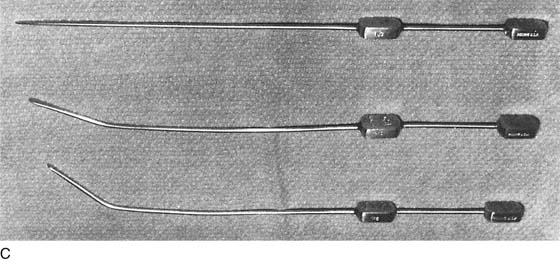
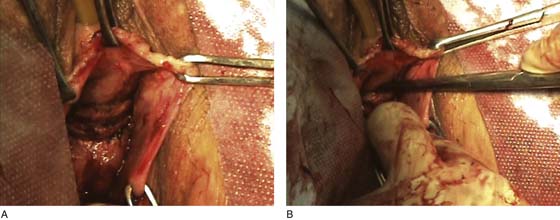
6. The sling is then brought into the field and is transferred from the vaginal incision to above the anterior abdominal fascia (Fig. 59–5F). Each arm is transferred with the use of a dressing forceps or some type of needle ligature carrier (Fig. 59–5G). Small incisions in the fascia allow each arm to come up through the fascia. Transfer of each arm of the sling is done under direct finger guidance with the use of a dressing forceps or a Stamey or Pereyra needle (Fig. 59–6A through C). A full-length pubovaginal sling should sit loosely at the level of the proximal urethra (Fig. 59–7).
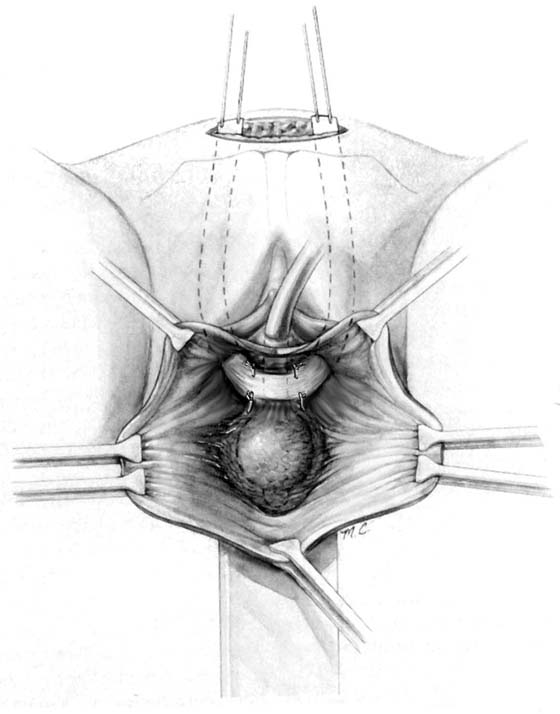
7. If a patch-type sling is utilized, the length of the patch is determined, and the longitudinal edges of the patch are usually attached to permanent sutures, which are passed into the anterior abdominal incision (Figs. 59–8 and 59–9). With some bone fixation techniques, sutures, or the sling itself, are directly anchored into bone. When the sling is directly anchored into bone, this can be done entirely via a vaginal incision, so an abdominal incision is not required. For patch slings, some surgeons do not enter the retropubic space and thus transfer the sutures after blind passage of the ligature carrier through the retropubic space.
8. Cystourethroscopy is performed to ensure no inadvertent injury or passage of any material through the bladder. Also, visualization of the proximal urethra and bladder neck documents that the sling is in the appropriate position. Elevation of the arms of the sling or the sutures should elevate or compress the proximal urethra. If no mobility occurs at this area, then the sling may be placed in the wrong anatomic position, or further periurethral dissection may need to be performed to create urethral mobility (Figs. 59–10 and 59–11).
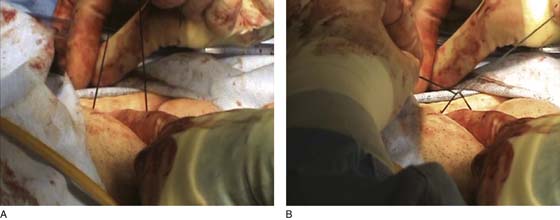
9. The final step in proximal suburethral sling placement involves appropriate tensioning of the sling. Unfortunately, no standardized method can be utilized on all patients. One must individualize the surgery on the basis of the severity of the patient’s incontinence and the state of her pelvic tissue. In general, the sling should be placed loosely at the level of the proximal urethra and should act as a backboard to prevent descent of the proximal urethra during increases in intra-abdominal pressure. Thus, after tying of the sling, downward traction on a Foley catheter should document that this area has been appropriately supported with the previously mentioned backboard mechanism. The author routinely places a right-angle clamp between the urethra and the sling material during tying, with the goal of maintaining zero tension at rest (Fig. 59–12). Ideally, a compressive mechanism initiated only during increases in abdominal pressure creates continence.
10. After the sutures are tied, the anterior vaginal wall is closed, and a transurethral or suprapubic catheter is left in place. A vaginal packing is also commonly utilized.
Figures 59–13 through 59–18 show a similar technique in which a piece of rectus fascia is used as the sling material.
FIGURE 59–6 A. The needle is passed under direct finger guidance. A finger in the vagina is inserted to the posterior aspect of the rectus muscle. (From Hurt WG: In Urogynecologic Surgery, 2nd ed. Lippincott, Williams & Wilkins, Philadelphia, 2000, with permission.) B. Pereyra ligature carrier. (Courtesy El Ney Industries, Inc., Upland, Calif.) C. Series of Stamey needles: straight needle (top), 15° angled needle (middle), and 30° angled needle (bottom). (Courtesy Pilling Company, Fort Washington, Pa.)
FIGURE 59–7 Full-length suburethral sling in which the sling material is passed and tied above the anterior rectus fascia.
FIGURE 59–8 A through C. Cadaveric fascia lata. Two pieces with the fibers running in opposite directions have been attached to each other.
FIGURE 59–9 A patch sling has been attached to sutures that have been passed via a long needle to the suprapubic area. The sling material is being held away from the urethra with T-clamps.
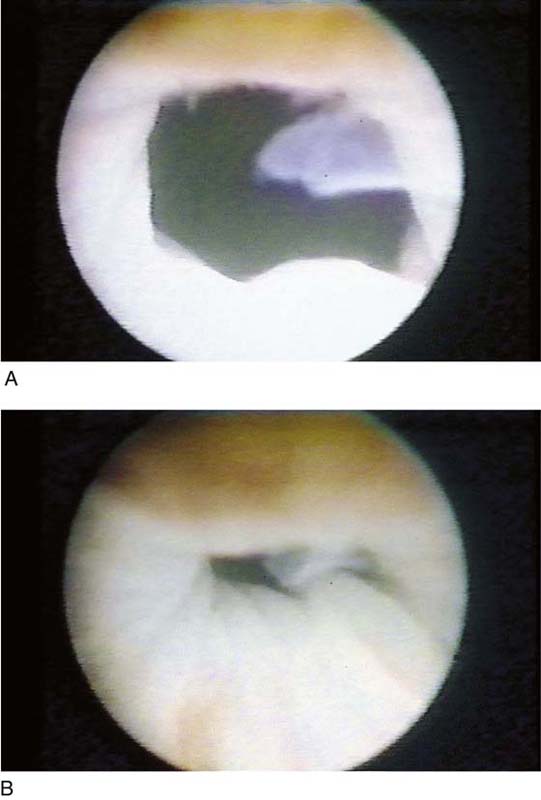
FIGURE 59–10 Urethroscopic view of the proximal urethra to confirm proper placement of the suburethral sling. A. Proximal urethra and bladder neck before elevation of sling. B. Elevation of the sling closes the bladder neck. This maneuver ensures proper placement of the sling under the proximal urethra.
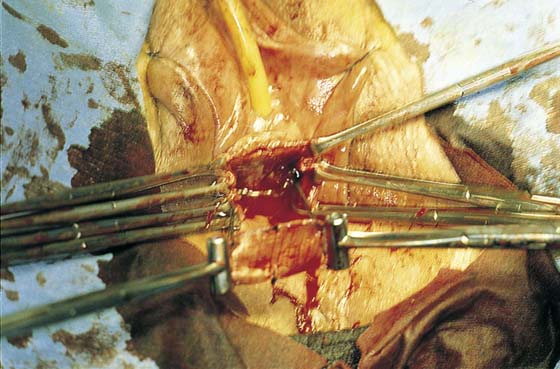
FIGURE 59–11 A patch sling in which a suburethral patch of fascia or synthetic material is suspended to the anterior rectus fascia with permanent sutures.
FIGURE 59–12 A right-angle clamp is placed between the patch and the urethra to prevent excess tension as sutures are being tied suprapubically.
FIGURE 59–13 A. A 1.5- to 2.0-cm-wide piece of rectus fascia is isolated and mobilized off the underlying rectus muscle. B. The mobilization is then extended laterally, resulting in an 8- to 10-cm-long piece of rectus fascia that will be used for the sling material.
FIGURE 59–14 After an anterior vaginal wall incision is made, the inferior pubic ramus is dissected on each side of the urogenital diaphragm sharply (shown on this figure) or bluntly to enter the retropubic space.
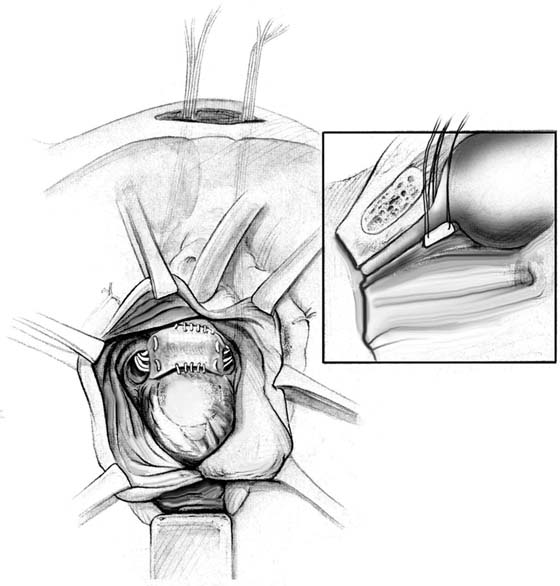
FIGURE 59–15 A Stamey needle is then passed from the suprapubic incision under direct finger guidance into the vaginal incision. This needle will be used to transfer a permanent suture that is attached to the lateral aspects of the sling into the suprapubic incision.
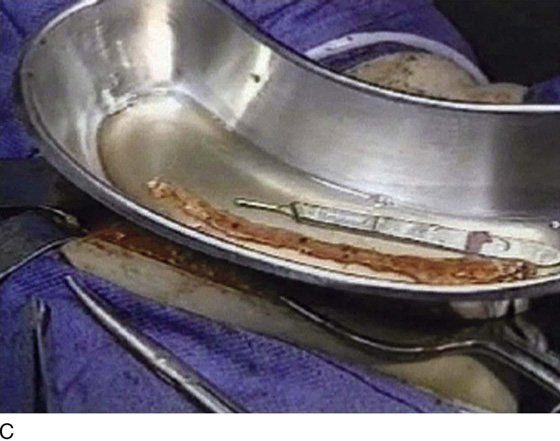
FIGURE 59–16 A permanent suture has been attached to the lateral edge of the rectus fascia sling.
FIGURE 59–17 A. Both sutures have been transferred into the suprapubic incision and (B) are loosely tied across the midline to each other.
FIGURE 59–18 A. The rectus fascia sling is shown supporting the proximal urethra. B. To ensure that the sling is not placed too tightly, a right-angle clamp can be passed easily between the sling material and the posterior urethra.

 Mark D. Walters
Mark D. Walters