Chapter 66 Psychocutaneous diseases
Gupta MA: Psychosomatic dermatology: is it relevant? Arch Dermatol 126:90–93, 1990.

Figure 66-1. Scale, scabs, and hair brought in by a patient with delusions of parasitosis who insists that these are parasites.
Edlich RF, Cross CL, Wack CA, Long WB 3rd: Delusions of parasitosis, Ann J Emerg Med 27:997–999, 2009.
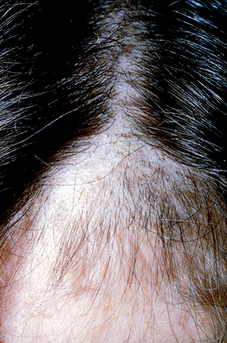
In trichotillomania, irregular patches of nonscarring, noninflammatory alopecia are covered with broken-off hairs of variable lengths that are scattered randomly between empty hair follicles (Fig. 66-4). Patients with trichotillomania often pull out their upper lid eyelashes but leave the lower lid eyelashes, as these are more difficult to grasp. Patients with alopecia areata may have eyelash loss on both the upper and lower lids.
Key Points: Psychocutaneous Diseases