38
Psoriasis: nails

Surface pitting is the best-known sign of psoriatic nail disease. Pits may be random but are often linear.
Onycholysis. Separation of the distal nail plate may be misdiagnosed as a Candida or fungal infection.

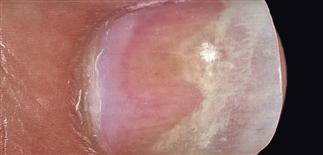
Oil spot lesions. Brown-red spots represent accumulation of serum under the nail.

Matrix lesions. Distortion of the entire nail plate occurs when psoriasis involves the nail matrix. The entire nail plate is affected.
DESCRIPTION
Distinct nail changes occur in psoriasis that support the diagnosis when skin changes are equivocal or absent. Psoriatic nail disease frequently misdiagnosed as nail fungal infection.
HISTORY
• Incidence varies from 10% to 50% in psoriasis patients. • Nail involvement may occur as isolated finding. • Fifty percent of patients complain of pain. • Arthritis of the distal phalangeal joint may be present.
PHYSICAL FINDINGS
Four distinct nail changes seen alone or in combination. • Pitting. Pitting in the nail plate is the most common finding. Nail plate cells are shed like psoriatic scale is shed, leaving tiny, punched-out depressions on the nail plate surface. Pits evolve from psoriasis in the superficial nail matrix. Pitted areas emerge from under the cuticle and grow out with the nail. Many other skin diseases cause pitting (e.g. eczema, fungal infections, alopecia areata), or it may occur as an isolated finding in a normal variation. • Onycholysis. Psoriasis of the distal skin of fingertip results in accumulation of yellow, scaly debris that elevates the nail plate. Debris is often mistaken for nail fungus infection. Psoriasis of the nail bed causes separation of nail from nail bed. Unlike the uniform separation caused by pressure on the tips of long nails, the nail detaches in an irregular manner. The nail plate turns yellow, simulating a fungal infection. • Oil spot lesion. Psoriasis of the nail bed causes localized separation of the nail plate. Cellular debris and serum accumulate in this space. The brown, yellow color observed through the nail plate looks like a spot of oil. • Nail deformity. Extensive involvement of the nail matrix results in a nail losing its structural integrity, resulting in fragmentation, crumbling. Gross alteration of the nail plate surface and nail bed splinter hemorrhages are common.
TREATMENT
Nail psoriasis is difficult to treat. Nails may improve when patients are treated with systemic agents such as ciclosporin, methotrexate, acitretin, or biologic agaents. • Triamcinolone acetonide. Intralesional injections at monthly intervals into the matrix with triamcinolone acetonide (Kenalog) (2.5–10 mg/mL) delivered with a 30-gauge needle is the standard treatment. Most patients lose interest in this painful procedure. Subungual hyperkeratosis, ridging, and thickening respond. Benefits are sustained for up to 9 months. Onycholysis and pitting less responsive. • Tazarotene. Tazarotene 0.1% gel (Tazorac) applied each evening for up to 24 weeks to fingernails. Medication can be used under occlusion or unoccluded. Onycholysis responds in occluded and non-occluded nails and pitting (in occluded nails). • Calcipotriene. Dovonex 0.005% solution applied to the distal nail and nail folds twice daily reportedly helps.







