CHAPTER 19 Proximal Tibial Osteotomy
High tibial osteotomy (HTO) is a surgical procedure used to change the mechanical weight-bearing axis and alter the loads carried through the knee. Conventional indications for HTO are medial compartment osteoarthritis and varus malalignment of the knee causing pain and dysfunction, but the indications for HTO have expanded with concomitant cartilage regeneration procedures and meniscal transplantation. Knee instability has been considered a contraindication; however, today the indications for HTO include patients with chronic ligament deficiencies and malalignment, because this procedure can change not only the coronal but also the sagittal plane of the knee, improving stability. In addition, despite good long-term results with total knee arthroplasty, there remains a significant concern regarding the longevity of these prostheses, particularly in younger patients. In contrast, osteotomy provides an alternative that preserves the knee joint, which, when appropriately performed, should not compromise later arthroplasty should this be necessary. The reported results of proximal tibial osteotomy vary considerably across the literature, but in general the procedure provides good relief of pain and restoration of function in approximately 80% to 90 % of patients at 5 years and 50% to 65 % at 10 years.1 Most authors who have analyzed these results have found that success is directly related to ideal patient selection and achieving optimal alignment.2 Accurate preoperative assessment and surgical technique are therefore essential to achieve a satisfactory outcome. This chapter will discuss the importance of alignment, clinic evaluation, radiographic assessment, indications and contraindications, techniques, and special situations regarding proximal tibial osteotomy.
ANATOMY
Importance of Alignment
The tibia has a coronal and sagittal plane, and it is mandatory to consider both in every situation. The normal anatomic axis (coronal plane) of the knee has a range from 5 to 7 degrees. In varus knees (malalignment in the coronal plane), degeneration of the articular cartilage tends to progress because of deviation of the mechanical axis.3 In the normal knee, the medial posterior tibial slope (sagittal plane) is usually 9 to 11 degrees and the lateral posterior tibial slope is generally 6 to 11 degrees; however, a wide range of values have been reported in various studies.4,5 The sagittal plane of the knee has often been ignored but its changes cause important modifications in the biomechanics of the knee and in joint stability. Decreased posterior tibial slope causes posterior tibia translation and helps the anterior cruciate ligament (ACL)–deficient knee. In contrast, increased tibial slope causes anterior tibial translation and helps the posterior cruciate ligament (PCL)–deficient knee. Some studies6,7 have demonstrated that the correction of the alignment is associated with the regeneration of articular cartilage that seemed apparently normal.
PATIENT EVALUATION
History and Physical Examination
A thorough clinical assessment requires a detailed history and physical examination. Specific analysis of this information will help determine whether a patient is likely to benefit from osteotomy. Important aspects of a patient’s general history include age, occupation, activity level, and medical and surgical history. Particularly significant are the expectations that the patient has for activity postoperatively. The patient may have noticed an increasing deformity or a static long-term malalignment. Pain history should focus on the site and severity, as well as aggravating and relieving factors. A history of locking, catching, or instability may indicate a mechanical source of symptoms, and the specific details of each of these symptoms should be sought to determine whether other procedures, such as arthroscopy, may be beneficial as an adjunct to osteotomy. Lower limb alignment should be assessed at each level, and the gait should be observed for any abnormalities, particularly a thrust in the direction of the deformity, indicating a significant dynamic component. Presence of deformity in all three planes should be assessed, particularly rotational deformity, because this is more difficult to assess later radiographically. Whether a deformity is fixed or correctable should be determined. The prresence of an effusion is determined and location of tenderness should be recorded carefully. Range of motion is measured, particularly looking for a flexion contracture and the amount of flexion comfortably achieved. Good mobility of the knee is a prerequisite, with no less then 110 degrees of flexion and no more than 10 degrees of extension loss. Patellar tracking and the presence of crepitus is to be noted, although the status of the patellofemoral joint is not determinate of indication. Ligaments are examined, including the ACL, AMC, PCL, medial cruciate ligament (MCL), and lateral cruciate ligament (LCL). Adjacent joints are examined and assessment of neurovascular function is essential.
Diagnostic Imaging
In 1992, Dugdale and colleagues8 proposed a flow chart for the radiologic evaluation of a patient with a varus of the knee, which was later modified by Noyes and associates.9 They stated that the patient should get stress x-rays if physical examination reveals any of the following: positive varus stress test, increased varus during thrust, increased tibial external rotation at 30 degrees of knee flexion, or varus recurvatum during standing or walking. If the x-rays are positive, the patient should get supine, full-length anteroposterior (AP) x-rays of both legs to evaluate the alignment. If the physical examination reveals none of these, the patient should get full-length double-stance AP x-rays of both legs. If a varus deformity is absent, they suggested that the patient undergo a soft tissue reconstruction; if this deformity is present, it is important to evaluate whether a lateral joint line opening is associated. If this is the case, the patient should get stress x-rays; if not the case, two methods to evaluate the amount of correction to perform during surgery could be used (see later). Since this study, many other reports have been published for radiographic evaluation of the alignment of the lower limb. We believe that the following imaging studies with (standard and stress x-rays) be obtained for these patients.
Standard X-Ray Evaluation
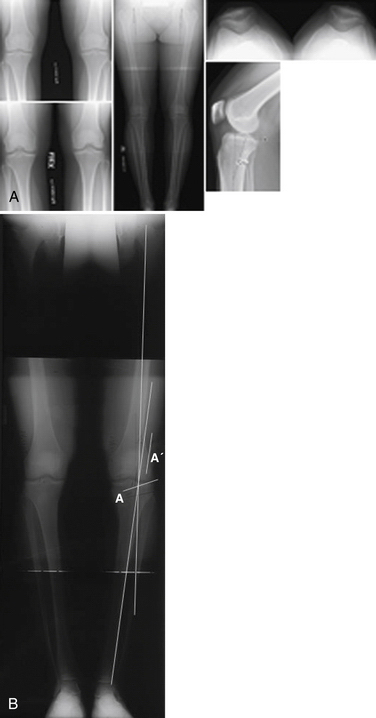
A full-length, double-stance AP x-ray is mandatory to evaluate femorotibial alignment (Fig. 19-1), as described by Moreland and coworkers.10 An AP x-ray is taken from the hips to the ankles with the patient standing and the patellae looking forward using a suitable cassette to filter the x-ray beam gradually for proper visualization of both hips and ankles.
Dugdale and colleagues8 have proposed two methods to quantify the amount of correction to perform if a malalignment is present. In both methods, a line along the tibial plateau and its intersection with the desired mechanical axis of the lower extremity is marked (in this chapter this point is called P for simplicity). A line is traced from the center of the femoral head to P and a line is traced from the center of the tibiotalar joint to P. In the first method, the angle formed at the intersection between these two lines represents the amount of correction required. In the second method, the radiographic film is cut along the osteotomy line and along a vertical line that converges with the first. Leaving a 2-mm hinge at the medial tibial margin, the distal part of the film is rotated until the femoral head, P, and the tibiotalar joint are along the same line. The overlapping wedge margin is the amount of correction to perform. It was also demonstrated that if lateral and/or posterolateral soft tissue structures are insufficient, for every increase of 1 mm in the lateral joint line width, there is 1 degree of added varus. Supine X-rays are important to eliminate the added varus because of the deficiency of the lateral and/or posterolateral structures and to evaluate the actual amount of correction to perform. It was also shown that after HTO, the mechanical axis of the lower extremity is translated laterally—3 to 4 mm for each degree of valgus correction—and this value depends on the height of the patient. We essentially use the same technique as described earlier to estimate the correction required.
The bilateral long-leg standing view is used (see Fig. 19-1B) to calculate the desired location of the new mechanical axis. If the two intersection lines are drawn from the center of the hip and from the center of the ankle, through the lateral tibial spine or 62% of the joint, bringing these two lines together will create the new mechanical axis. The osteotomy is drawn (line A) and measured and transposed to the two intersecting lines (line A′); the amount of opening measured at that point is the amount of correction required.
A lateral x-ray view is used to evaluate posterior tibial slope. A number of methods have been reported to quantify its value. Dejour and Bonnin4 have recommended tracing a line along the proximal tibial anatomic axis (PTAA) and a line along the tibial plateau; the angle between these two lines is tibial slope. Moore and Harvey,11 in 1974, described the tibial plateau angle. They recommended tracing a line along the anterior tibial cortex (ATC) and a line along the medial tibial plateau; the angle between these two lines is tibial slope.
Brazier and associates5 have proposed three other methods:
They compared these three techniques and stated that the most reliable are the PTAA and PTC methods.
Cullù and coworkers12 have compared the various methods and found higher values for the same patients using the method described by Moore and Harvey11 and lower values with the PFAA method.5 We recommend using the line along the articular surface of the medial tibial plateau and the anatomic axis (PTAA) for assessing the posterior slope, because it is simple and reproducible.
Stress X-Ray
The lateral stress view, according to the Telos method, was first described by Jacobsen in 1976.13 The patient lies in the lateral decubitus position with the knee flexed at 90 degrees and is encouraged to relax. The heel is fixed to a stand and the arm of the Telos GA II device (Telos; Weterstadt, Germany) applies a posterior force to the tibia. In this position, a lateral x-ray is taken. The test is then performed with the knee at 25 degrees of flexion.13 This method is important in chronic PCL-deficient knees to evaluate anterior and posterior tibial translation with regard to the femur. It is also useful to detect a fixed posterior tibial subluxation, as described by Strobel and colleagues14 in 2002; they found it to be present in 44% of patients with a PCL lesion.
The lateral stress view using the kneeling method15 also measures posterior subluxation. The patient kneels on a bench with the knee in 90 degreesof flexion; the bench supports the lower legs only up to the tibial tubercle. A lateral x-ray is taken.
In addition, a lateral stress view with hamstring contraction was described by Chassaing and associates16 in 1995. The patient lies in the lateral decubitus or seated position, with the knee at 90 degrees of flexion and the heel fixed to a stand. A lateral x-ray is taken while the patient contracts the hamstring for at least 10 seconds.17
Finally, a lateral stress view is obtained according to the gravity method described by Stäubli and Jakob in 1990.18 The patient lies in the supine position with the hip and the knee at 90 degrees of flexion, supported by an assistant, with the leg in neutral rotation. In this position, a lateral x-ray is taken.
The axial stress view described by Puddu and coworkers19 in 2000. The patient lies in the supine position, with both knees at 70 degrees of flexion, the feet plantigrade in moderate plantar flexion, and the tibia in neutral rotation. The x-ray beam is directed parallel to the longitudinal patellar axis from distal to proximal and the distance between the anterior tibial profile and the center of the femoral groove is measured. The side to side difference is the amount of posterior instability.
Jung and colleagues, in 2006,17 compared these five methods, focusing on posterior translation, side to side difference, condylar rotation, time to perform the test, and pain during the test. Considering all these factors, they stated that the most effective methods are with the Telos device at 90 degrees of knee flexion and the kneeling method, even if they are painful and time-consuming procedures. The Telos procedure is the most expensive but the most reliable for detecting a posterior tibial subluxation.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is useful to evaluate the meniscal, articular cartilage, and soft tissue (ligamentous) status of the knee. In addition, with compartment overload, there may be subchondral edema, indicating the need for unloading that compartment. Traumatic subchondral bone lesions20 can easily be detected.
TREATMENT
Indications And Contraindications
Proper patient selection is fundamental for satisfactory postoperative results. In general, having the knee joint in good condition will result in a more predictable outcome. Naudie and associates1 have concluded that younger patients who have excellent knee range of motion (ROM), higher functional demand, and a lower grade of osteoarthritis (OA) will have better outcomes, and that the survival of the HTO will be much longer than in more advanced knees.
Arthroscopic Technique
Gradual correction is obtained by external fixation.
Lateral Closing Wedge Osteotomy (Acute Correction)
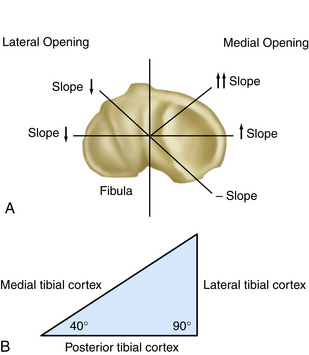
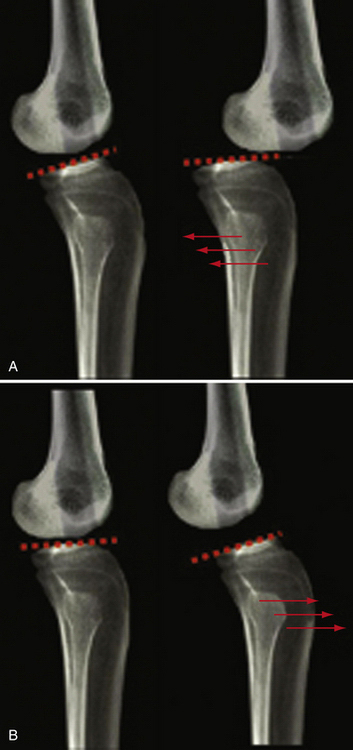
Jackson21 in 1958 and Wardle22 in 1962 described the earliest techniques of proximal tibial valgus osteotomies with a lateral closing wedge, but it was popularized by Coventry23 and Insall and coworkers.24 The goal is correction of alignment, as noted, which is achieved by removing a laterally based wedge of bone and closing the resultant defect. The main cited advantages of this procedure over the opening wedge technique are avoidance of the need for a bone graft, a more stable construct postoperatively allowing earlier weight bearing, and ta heoretically decreased risk of nonunion. The disadvantages of this procedure include the following: (1) difficulty in predicting the amount of correction in the coronal and sagittal planes; (2) inability to adjust the correction intraoperatively; (3) the requirement for two bone cuts; (4) violation of proximal tibiofibular joint or fibular head; and (5) palsy of the external popliteal sciatic nerve. The proximal anteromedial tibial cortex, viewed in cross section, has an oblique or triangular shape and forms an angle of 45 ± 6 degrees with the posterior margin of the tibia; the lateral tibial cortex, however, is almost perpendicular to the posterior margin of the tibia. Because of the same anatomic features, a lateral closing wedge osteotomy causes small decreases in the posterior tibial slope. However, Amendola and colleagues25 have demonstrated that a lateral closing wedge HTO causes a decrease in the posterior tibial slope (Fig. 19-2).
The technique described here is used at our institution when a lateral closing wedge osteotomy is indicated. All patients should receive a prophylactic preoperative dose of intravenous antibiotics. The patient lies in a supine position on the radiolucent operating table; the leg is draped in a sterile fashion. Setup should allow radiographic visualization of the lower limb from hips to ankles, with the fluoroscope coming in from the contralateral side. A lateral support is placed to allow the knee to rest unsupported at 90 degreesof flexion, the position used during most of the procedure. A marking pen is used to outline the fibular head, lateral joint line, patellar tendon, and tibial tubercle. The leg is raised and a tourniquet is inflated. Arthroscopy is performed to treat mechanical symptoms, evaluate articular cartilage and menisci, and occasionally to confirm the indication for HTO.9 We use an L-shaped skin incision with the vertical limb along the lateral edge of the tibial tubercle and the horizontal limb parallel and 1cm distal to the lateral joint line, taken posteriorly to the anterior aspect of fibular head. Dissection is carried down to expose the fascia of the anterior compartment, which is incised along the anterolateral crest of the tibia, leaving a 5-mm cuff for later closure. A Cobb elevator is used to elevate the muscle from the anterolateral surface of the tibia and the iliotibial tract is elevated from Gerdy’s tubercle proximally. The common peroneal nerve is not routinely exposed but is palpated and protected throughout the procedure.
A number of methods for treatment of the proximal tibiofibular joint have been described, including joint excision or disruption, fibular osteotomy, and excision of the fibular head. We prefer to disrupt the joint but preserve the fibular head. The proximal tibiofibular joint is exposed, the anterior capsule incised, and a curved osteotome is directed posteromedially to disrupt this articulation and mobilize the fibula so as not to impede later correction. A Z-shaped retractor is placed through this joint along the posterior aspect of the tibia to protect posterior soft tissues. It is critical that this retractor be placed directly against bone along the posterior cortex to protect the neurovascular structures.
The lateral edge of the patellar tendon is identified and a second Z retractor is placed underneath it to protect it during the osteotomy. In this way, the proximal tibia is exposed from the tibial tubercle to the posterolateral cortex and is therefore prepared for the osteotomy. In removing a laterally based wedge, an angular cutting guide can be used or a specific-sized wedge can be removed. The angled cutting jig system (Guidant) was initially described by Hofmann and colleagues27; it allows for easier use of preoperative calculations and should increase the accuracy of the resultant correction. With this system, the initial step involves making two 3.5-mm drill holes parallel to and approximately 1cm distal to the joint line, across to but not through the medial cortex. A line drawn between these two holes should match the posterior slope of the tibia and the position is checked in both planes with the fluoroscope. These holes are the site of the final proximal fixation and serve as the reference for the remainder of the cuts. Two temporary pins are placed in these holes and a third hole is then drilled distal to these through the medial cortex; this allows measurement of the tibial width to guide for depth of the saw cut. Using the jig, the proximal cut of the osteotomy is performed using a calibrated saw blade to a depth 10 mm less than the measured tibial width. The first jig is removed and a second jig is used, which has a blade that lies in the first saw cut to its full depth and has angled cutting slots at 2-degree increments. The second saw cut is made through the chosen angled slot, with the jig controlling the depth of the saw cut by its position.
Medial Opening Wedge Osteotomy (Acute Correction)
Open wedge osteotomy has not been used as long as the lateral closing wedge osteotomy. It was first described by Hernigou and coworkers26 although this technique had been used since 1951 by Debeyre. At the beginning of the 1990s, Puddu28 developed a plate (Puddu plate, Arthrex spacer plate; Arthrex; Naples, Fla), which supports osteotomy surfaces internally by metal spacers (wedges) to prevent further collapse and that has metal blocks (spacer teeth). In 2000, Fowler and colleagues29 modified Puddu’s open wedge osteotomy technique. The most recent modification is lower profile and is a six-hole spacer plate (ContourLock HTO plate; Arthrex). The TomoFix plate (internal plate fixator, plate fixator, or rigid plate fixation; Synthes; West Chester, Pa) was developed by Lobenhoffer and colleagues.30 In addition, a C plate or T plate can be used.
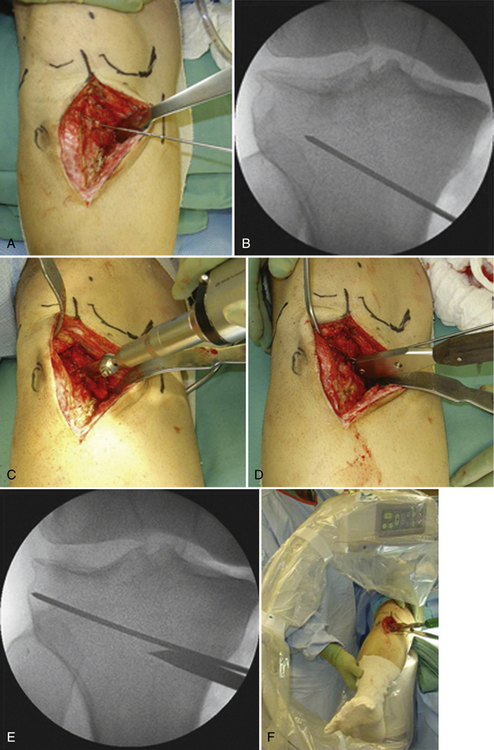
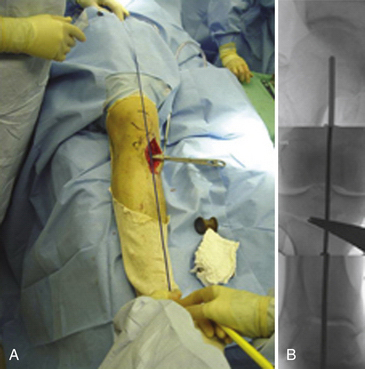
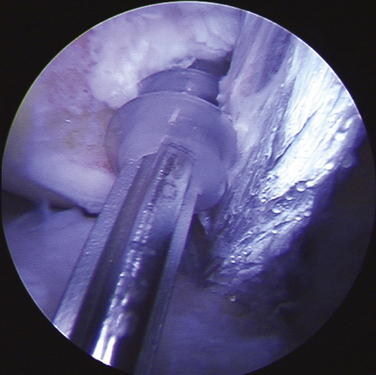
Arthroscopy is performed as indicated, as with the closing wedge technique. A vertical incision is made just behind the pes anserine, between the medial border of the patellar tendon and the posterior border of the tibia. the sartorius fascia is cut to visualize the hamstring tendons. Under fluoroscopic control, a guide wire is positioned medially to laterally. The wire is placed at the level of the superior aspect of the tibial tubercle anteromedially, at about 1.5 cm below the lateral articular margin of the tibia. A cortical osteotomy is performed with an oscillating saw, inferiorly to the guide wire, and it is continued with an osteotome under fluoroscopic control (Fig. 19-3). When the osteotomy is completed, the medial tibia is opened with a wedge of a suitable width (Fig. 19-4). It is important to make the cut parallel to the joint surface in the sagittal plane, with the apex of the osteotomy at the proximal tibiofibular joint, to obviate the need for disrupting this articulation.
Wedges have a graduated scale to quantify the angular correction achieved.9 The position of the wedge is important to correct the deformity on the sagittal plane; the proximal anteromedial tibial cortex, viewed in cross section, has an oblique or triangular shape and forms an angle of 45± 6 degrees with the posterior margin of the tibia. However, the lateral tibial cortex is almost perpendicular to the posterior margin of the tibia. Because of these anatomic features, a wedge placed anteriorly causes an increase in posterior tibial slope, whereas a posterior wedge tends to decrease the posterior tibial slope slightly.31
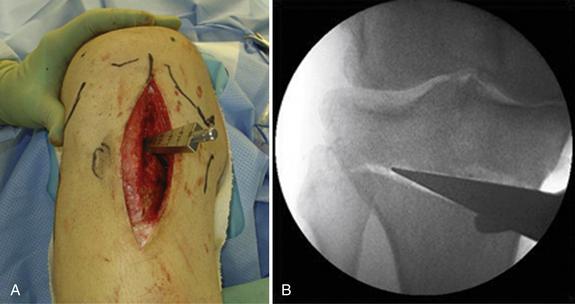
Anterior and posterior gaps of the osteotomy are then measured with a ruler, which is important to calculate the amount of increase in posterior tibial slope. If the anteromedial gap is half of the posteromedial gap, the slope will not change; for each millimeter of increase of the anterior gap, the posterior tibial slope will increase by 2 degrees. An image intensifier and alignment rod are used to control coronal and sagittal alignment during axial loading of the joint (Fig. 19-5). If the anterior gap is more than 1 cm, it is better to perform an osteotomy to lift up the tibial tubercle of the same amount to avoid patella infera (patella baja). When the correction in the two planes is achieved, the osteotomy is stabilized with a plate with four holes (Arthrex), with two 6.5-mm proximal cancellous screws and two 4.5-mm distal cortical screws (Fig. 19-6). Generally, to fill the osteotomy gap, a carefully shaped allograft bone block from a donor is used (Fig. 19-7). Under fluoroscopic contro,l the final result is checked before the tourniquet is deflated; hemostasis and skin suturing are then performed.9
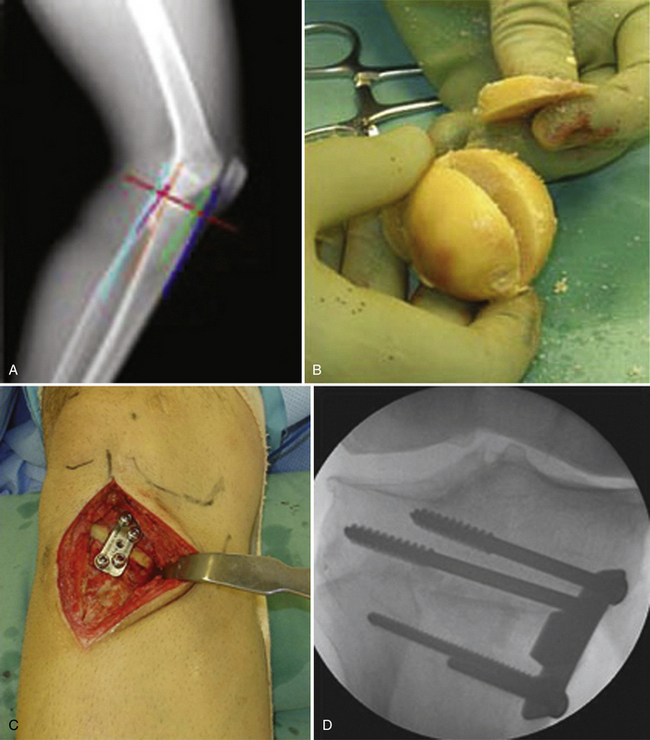
FIGURE 19-7 A-D, Generally a carefully shaped bone block from a donor is used to fill the osteotomy gap.
PEARLS& PITFALLS
Postoperative Management
External Fixation (Gradual Correction)
Use of an external fixator to achieve a gradual correction has been advocated by some for f large deformities, and good results have been reported with this technique.32 There are potential advantages with this technique. First, large corrections may be technically impossible with standard closing or opening wedge techniques because of excessive bone removal compromising fixation and creating deformity in the closed wedge technique, or excessive soft tissue tension in the opening wedge technique. External fixators also allow constant manipulation of the alignment during the healing process to optimize alignment.32 Circular external fixators also allow easy manipulation of angular and translational correction in all three planes, as required.
Special Situations with High Tibial Osteotomy
Cartilage Resurfacing Procedures
The ability of HTO to stimulate articular cartilage reparation with fibrocartilage has been reported by many authors.33 The use of cartilage resurfacing techniques in association with HTO has the rationale of trying to achieve better cartilage regeneration and potentially better outcomes. Articular cartilage defects can be managed by marrow stimulation (e.g., subchondral drilling, abrasion arthroplasty, microfracture), autologous cultured chondrocyte implantation, osteochondral autograft transplantation (e.g., mosaicoplasty), or autogenous periosteal grafts.34
The most commonly performed procedures reported in the literature are abrasion arthroplasty, microfractures, and the implantation of autologous chondrocytes. Some have demonstrated that autologous chondrocyte implantation is a management option for chondral defects, but this is contraindicated in the presence of tibiofemoral malalignment, which would impose mechanical overload to the repair tissue. For this reason, in patients with concurrent chondral defects and varus knee malalignment, we recommend correcting the malalignment with a proximal tibial osteotomy plus arthroscopic autologous chondrocyte implantation.35 Some researchers have agreed that the degenerative knee can be treated by using a chondral resurfacing procedure, such as microfracture or abrasion arthroplasty, will improve results obtained with an osteotomy alone.36 Akizuki and colleagues,36 in a prospective study, compared the cartilage regeneration in osteoarthritic knees treated with HTO alone and HTO plus abrasion arthroplasty. At approximately 12 months after arthroscopy, they observed better regeneration in the abrasion arthroplasty group. They did not find any significant clinical difference between the two groups at 2 to 9 years of follow-up.
Matsunaga and associates37 have compared patients with medial knee OA treated with proximal lateral closing wedge tibial osteotomy alone, osteotomy plus microfracture, and osteotomy plus abrasion arthroplasty. They observed that the repair of the cartilage was better in the abrasion arthroplasty group than in the other two groups at 1 year after surgery. No difference in the clinical outcome was found among the three groups at 5 years after surgery. In conclusion, all these techniques demonstrated the ability to stimulate cartilage regeneration better than osteotomy alone, but the clinical benefit has still to be demonstrated.
Meniscal Transplantation
Generally, meniscectomy results in joint overload and osteoarthritis in the long term. The use of meniscal transplantation has been popularized and described in many studies and reviews. The association of an osteotomy with meniscal transplantation proposes to relieve pain in a compromised medial compartment and protect the transplanted tissue from overload, improving its long-term viability.38
Medial meniscus transplantation is indicated when the mechanical axis lies within that compartment on double-limb standing x-rays. The preferred technique is opening wedge HTO to correct the mechanical axis to the lateral tibial spine (do not overcorrect). Lateral meniscus transplantation is also indicated when the mechanical axis lies within that compartment on double-limb standing x-rays. The preferred technique is opening wedge distal lateral femoral osteotomy to correct the mechanical axis just to the medial tibial spine (do not overcorrect). Better results were reported when meniscal transplantation was associated with the osteotomy than with medial meniscal transplantation without osteotomy.39
Ligament Instability
Traditionally, knee instability has been considered a contraindication. Currently however, the indications for HTO include patients with chronic ligament deficiencies and malalignment, because this procedure can change not only the coronal but also the sagittal plane of the knee. The sagittal plane modification has a significant impact on biomechanics and joint stability. Decreased posterior tibial slope causes posterior tibia translation and helps the ACL-deficient knee. Conversely, increased tibial slope causes anterior tibial translation and helps the PCL-deficient knee (Fig. 19-8). A medial opening wedge HTO increases posterior tibial slope if the plate is placed anteromedially but does not change the posterior tibial slope if the plate is placed posteromedially. A lateral closing wedge HTO that has equal anterior and posterior gaps along the lateral tibial cortex would have little effect on posterior tibial slope. Some have noted that soft tissue techniques alone, without correction of the alignment, often have poor results because a bone deformity overstresses them.40 Furthermore, soft tissue destruction causes a decrease in neuromuscular joint control, which over time can worsen the malalignment.41 Some studies26 have found satisfying results after HTO in monocompartmental knee OA and varus alignment, but there are few studies about the results of HTO in the unstable knee.42,43 Rupture of the ACL, if untreated, leads to chronic anterior knee instability. Recurrent nonphysiologic translation-rotation movements of the unstable knee cause increased stress for menisci and cartilage, which often results in meniscal tears and medial cartilage degeneration. However, the problem of the combination of painful unicompartmental degeneration and symptomatic instability cannot be addressed by osteotomy or ACL reconstruction alone. There is no agreement in the literature about which patients require one and which require both procedures, and whether they are to be performed staged or simultaneously.9,44
Generally, the most common indication for simultaneous HTO and ACL replacement is anterior knee instability (chronic) in symptomatic varus malalignment. If malalignment is constitutional and no medial symptoms are present, osteotomy in addition to ACL replacement should only be performed if there is considerable meniscal loss and varus angulation is significant. The extent of unicompartmental joint degeneration should be mild. Usually, patients who are considered for the combined HTO and cruciate ligament reconstruction procedures is younger than 40 years. However, there is no absolute contraindication for the simultaneous procedure in older patients. Factors more important than age in the diagnostic assessment include the patients’ level of activity and extent of the medial degenerative changes. For example, if degeneration is advanced and the primary complaint is pain rather than instability, only HTO should be performed because in advanced osteoarthritis, tight joint play may even worsen the symptoms. In this case, a staged procedure, with HTO initially followed by ACL reconstruction if instability problems persist, may be considered.
CONCLUSIONS
Proximal tibial osteotomy can be used to correct varus and valgus deformities in the management of isolated medial or lateral compartment osteoarthritis. There are a number of operative techniques described to achieve this goal and the relative merits of each have been outlined. Whatever the technique used, critical to the success of the procedure are the selection of the appropriate patient and the attainment of a precise correction without complications. If these goals are met, proximal tibial osteotomy should provide long-term relief of pain and restoration of function.
1. Naudie D, Bourne RB, Rorabeck CH, Bourne TJ. The Insall Award. Survivorship of the high tibial valgus osteotomy. A 10- to -22-year followup study. Clin Orthop Relat Res. 1999:18-27.
2. Yasuda K, Majima T, Tsuchida T, Kaneda K. A ten- to 15-year follow-up observation of high tibial osteotomy in medial compartment osteoarthrosis. Clin Orthop Relat Res. 1992;(282):186-195.
3. Phisitkul P, Wolf BR, Amendola A. Role of high tibial and distal femoral osteotomies in the treatment of lateral-posterolateral and medial instabilities of the knee. Sports Med Arthrosc Rev. 2006;14:96-104.
4. Dejour H, Bonnin. Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br. 1994;76:745-749.
5. Brazier J, Migaud H, Gougeon F, et al. Evaluation of methods for radiographic measurement of the tibial slope. A study of 83 healthy knees. Rev Chir Orthop Reparatrice Appar Mot. 1996;82:195-200.
6. Odenbring S, Egund N, Lindstrand A, et al. Cartilage regeneration after proximal tibial osteotomy for medial gonarthrosis. An arthroscopic, roentgenographic, and histologic study. Clin Orthop Relat Res. 1992;(277):210-216.
7. Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, et al. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch Orthop Trauma Surg. 2004;124:575-584.
8. Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;274:248-264.
9. Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med. 2000;28:282-296.
10. Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745-749.
11. Moore TM, Harvey JPJr. Roentgenographic measurement of tibial-plateau depression due to fracture. J Bone Joint Surg Am. 1974;56:155-160.
12. Cullù E, Aydogdu S, Alparslan B, Sur H. Tibial slope changes following dome-type high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2005;13:38-43.
13. Jacobsen K. Stress radiographical measurement of the anteroposterior, medial and lateral stability of the knee joint. Acta Orthop Scand. 1976;47:335-344.
14. Strobel MJ, Weiler A, Schulz MS, et al. Fixed posterior subluxation in posterior cruciate ligament-deficient knees: diagnosis and treatment of a new clinical sign. Am J Sports Med. 2002;30:32-38.
15. Louisia S, Siebold R, Canty J, Bartlett RJ. Assessment of posterior stability in total knee replacement by stress radiographs: prospective comparison of two different types of mobile bearing implants. Knee Surg Sports Traumatol Arthrosc. 2005;6:476-482.
16. Chassaing VDF, Touzard R, et al. Etude radiologique du L.C.P. à 90 de flexion. Rev Chir Orthop. 1995;81:35-38.
17. Jung TM, Reinhardt C, Scheffler SU, Weiler A. Stress radiography to measure posterior cruciate ligament insufficiency: a comparison of five different techniques. Knee Surg Sports Traumatol Arthrosc. 2006;14:1116-1121.
18. Stäubli HU, Jakob RP. Posterior instability of the knee extension. A clinical and stress radiographic analysis of acute injuries of the posterior cruciate ligament. J Bone Joint Surg Br. 1990;2:225-230.
19. Puddu G, Gianni E, Chambat P, De Paulis F. The axial view in evaluating tibial translation in cases of insufficiency of the posterior cruciate ligament. Arthroscopy. 2000;16:217-220.
20. Puddu G, Cipolla M, Cerullo G, et al. Osteotomies: the surgical treatment of the valgus knee. Sports Med Arthrosc. 2007;15:15-22.
21. Jackson JP. Osteotomy for osteroarthritis of the knee. Proceedings of the Sheffield Regional Orthopaedic Club. J Bone Joint Surg Br. 1958;40:826.
22. Wardle EN. Osteotomy of the tibia and fibula. Surg Gynecol Obstet. 1962;115:61-64.
23. Coventry MB. Upper tibial osteotomy. Clin Orthop Relat Res. 1984;(182):46-52.
24. Insall J, Shoji H, Mayer V. High tibial osteotomy. A five-year evaluation. J Bone Joint Surg Am. 1974;56:1397-1405.
25. Amendola A, Rorabeck CH, Bourne RB, Apyan PM. Total knee arthroplasty following high tibial osteotomy for osteoarthritis. J Arthroplasty. 1989;4(suppl):S11-S17.
26. Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten- to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69:332-354.
27. Hofmann AA, Wyatt RW, Beck SW. High tibial osteotomy. Use of an osteotomy jig, rigid fixation, and early motion versus conventional surgical technique and cast immobilization. Clin Orthop Relat Res. 1991;(271):212-217.
28. Puddu G. High tibial osteotomy. The arthritic knee in the young athlete, SYM 15. Paper presented at: 11th ESSKA 2000 Congress and 4th World Congress on Sports Trauma; 2004; Athens.
29. Fowler PJ, Tan JL, Brown GA. Medial opening wedge high tibial osteotomy: how I do it?. Oper Tech Sports Med. 2000;1:32-38.
30. Lobenhoffer P, De Simoni C, Staubli AE. Open-wedge high tibial osteotomy with rigid plate fixation. Tech Knee Surg. 2002;1:93-105.
31. Rodner CM, Adams DJ, Diaz-Doran V, et al. Medial opening wedge tibial osteotomy and the sagittal plane: the effect of increasing tibial slope on tibiofemoral contact pressure. Am J Sports Med. 2006;34:1431-1441.
32. Magyar G, Ahl TL, Vibe P, et al. Open-wedge osteotomy by hemicallotasis or the closed-wedge technique for osteoarthritis of the knee. A randomised study of 50 operations. J Bone Joint Surg Br. 1999;81:444-448.
33. Amendola A. Panarella L. High tibial osteotomy for the treatment of unicompartmental arthritis of the knee. Orthop Clin North Am. 2005;36:497-504.
34. Peterson L, Brittberg M, Kiviranta I, et al. Autologous chondrocyte transplantation. Biomechanics and long-term durability. Am J Sports Med. 2002;30:2-12.
35. Alford JW, Cole BJ. Cartilage restoration, part 2: techniques, outcomes, and future directions. Am J Sports Med. 2005;33:443-460.
36. Akizuki S, Yasukawa Y, Takizawa T. Does arthroscopic abrasion arthroplasty promote cartilage regeneration in osteoarthritic knees with eburnation? A prospective study of high tibial osteotomy with abrasion arthroplasty versus high tibial osteotomy alone. Arthroscopy. 1997;13:9-17.
37. Matsunaga D, Akizuki S, Takizawa T, et al. Repair of articular cartilage and clinical outcome after osteotomy with microfracture or abrasion arthroplasty for medial gonarthrosis. Knee. 2007;14:465-471.
38. Cameron JC, Saha S. Meniscal allograft transplantation for unicompartmental arthritis of the knee. Clin Orthop Relat Res. 1997;(337):164-171.
39. Annunziato A. Knee osteotomy and meniscal transplantation: indications, technical considerations and results. Sports Med Arthrosc Rev. 2007;15:32-38.
40. Christel P. Basic principles for surgical reconstruction of the PCL in chronic posterior knee instability. Knee Surg Sports Traumatol Arthrosc. 2003;11:289-296.
41. Lephart SM, Pincivero DM, Rozzi SL. Proprioception of the ankle and knee. Sports Med. 1998;25:149-155.
42. Fowler PJ, Kirkley A, Roe J. Osteotomy of the proximal tibia in the treatment of chronic anterior cruciate ligament insufficiency. J Bone Joint Surg Br. 1994;76(suppl):26.
43. Naudie DD, Amendola A, Fowler PJ. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med. 1994;32:60-70.
44. Williams RJ 3rd, Wickiewicz TL, Warren RF. Management of unicompartmental arthritis in the anterior cruciate ligament-deficient knee. Am J Sports Med. 2000;28:749-760.