Chapter 42 Protocols for Imaging Studies in the Oncologic Patient
Well-thought-out protocols imaging sophisticated imaging studies are critical to ensure that the resultant images have the best possible chance to answer the clinical question. In the case of oncologic patients, this usually hinges on whether disease is stable, has regressed, or has progressed and whether there are new sites of disease. Beyond this fundamental question, our patients may have unexpected findings as well as complications from therapy. The ability to answer such questions relies on high-quality images and, in the case of computed tomography (CT), the best quality titrated with the least radiation exposure because patients generally go into a lifetime of surveillance. This is a significant challenge. In patients undergoing imaging for surgical intervention, especially for cure, these studies need to be directly targeted to the most likely sites of metastases (e.g., high-quality liver imaging for metastases in patients with orbital, choroidal melanoma) and have optimal image quality to detect metastatic disease.1–5 Imaging with multidetector computed tomography (MDCT) can be performed in multiple phases, and developing protocols to detect hyper- as well as hypovascular metastases is critical in evaluating patients with tumors such as carcinoid, islet cell tumors of the pancreas, and a number of other primaries. Timing of the contrast bolus and subsequent imaging is critical in magnetic resonance imaging (MRI) as well as current MDCT scanning.6–8
MDCT: CT Imaging
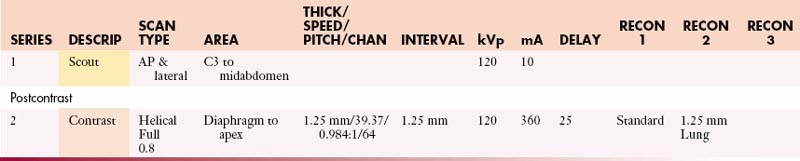
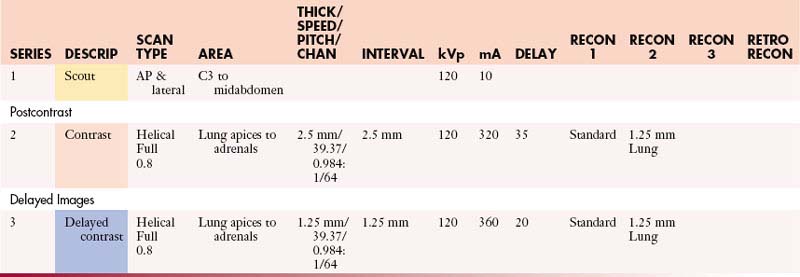
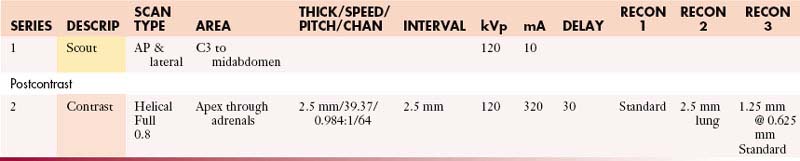
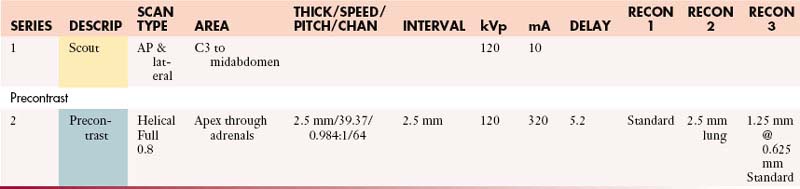
Chest Protocols (MDCT 64 Slice)
Abdomen/Pelvis Protocols (MDCT 64 Slice)
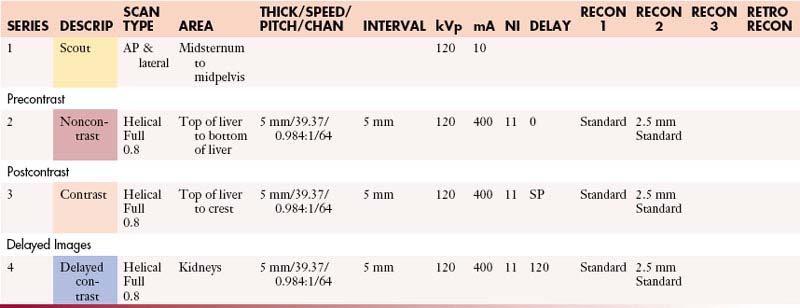
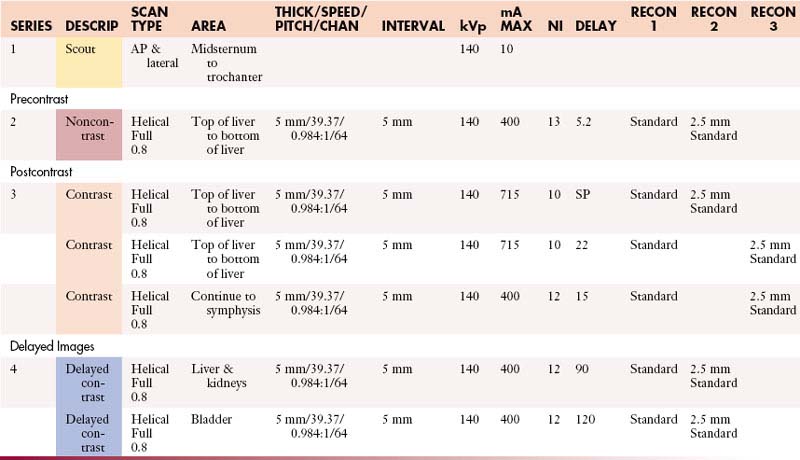
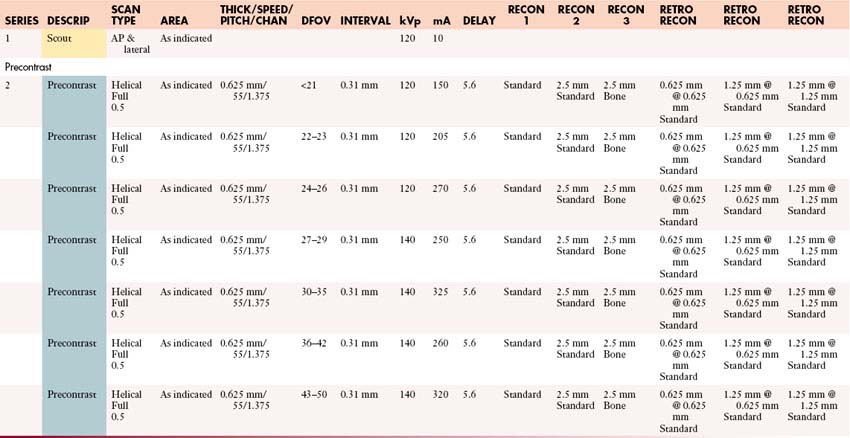
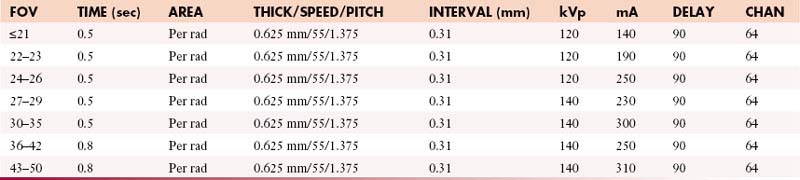
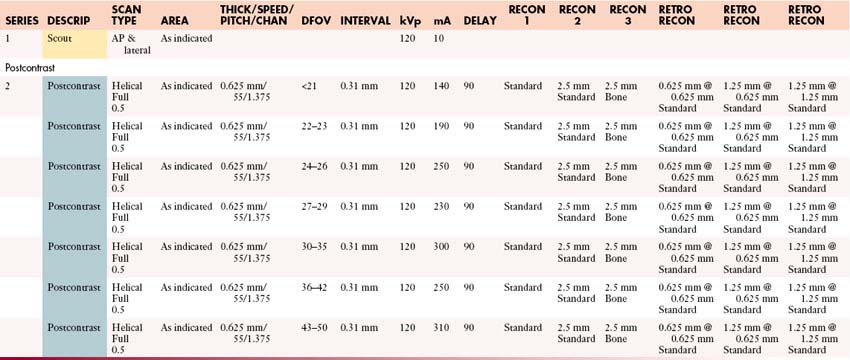
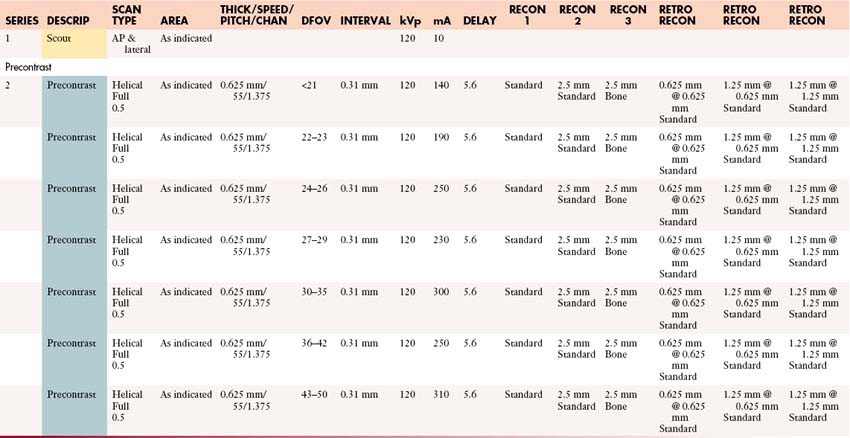
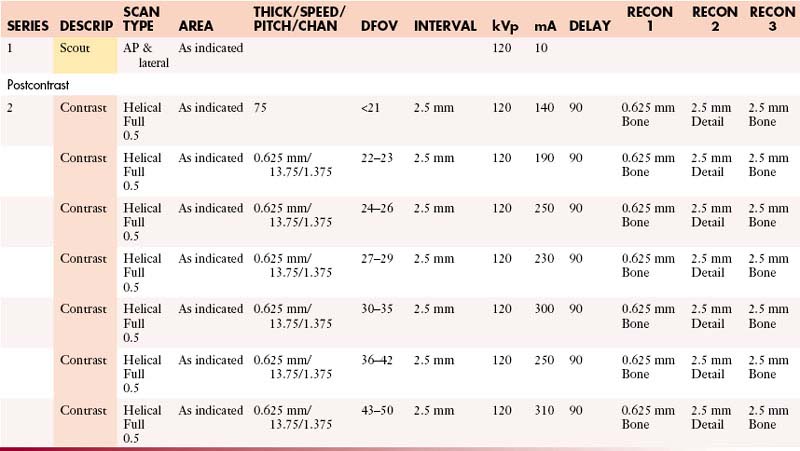
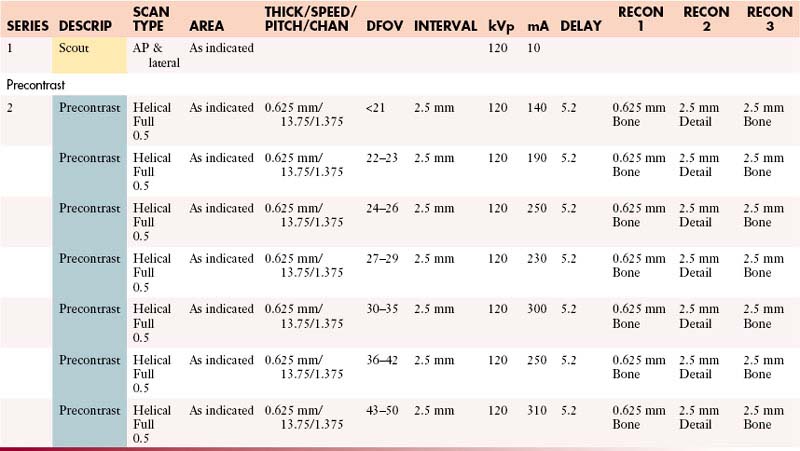
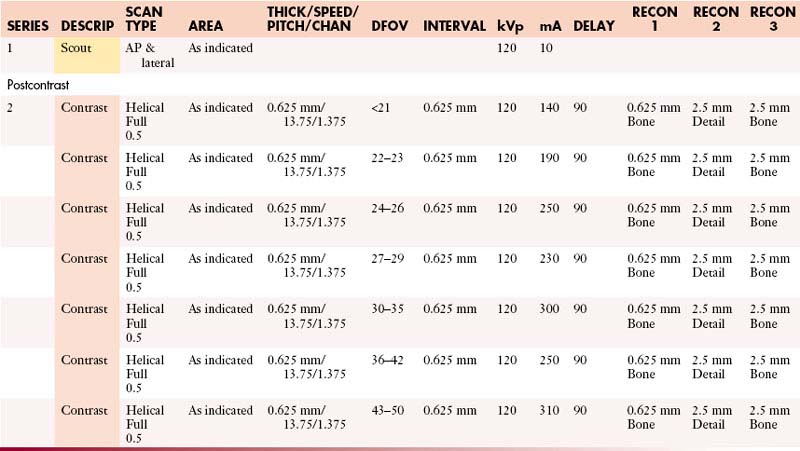
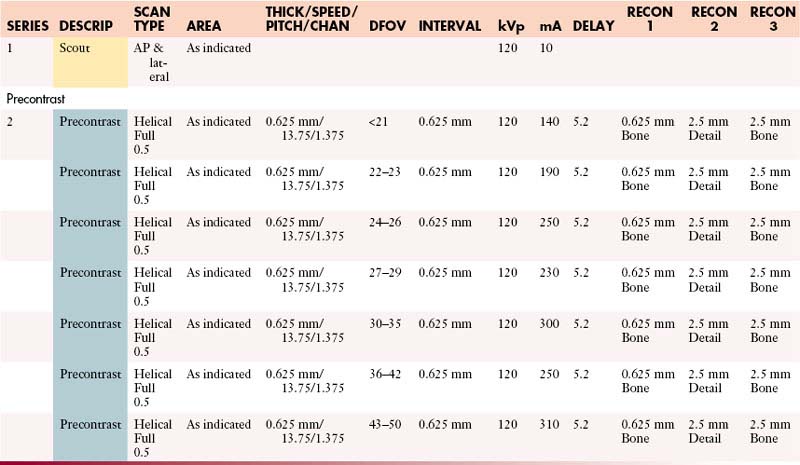
Abdomen without and with Contrast
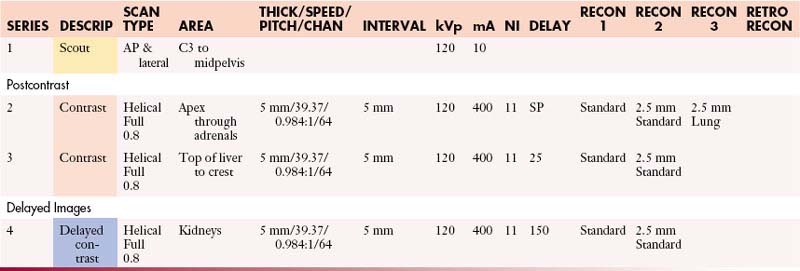
Abdomen and Pelvis with Contrast
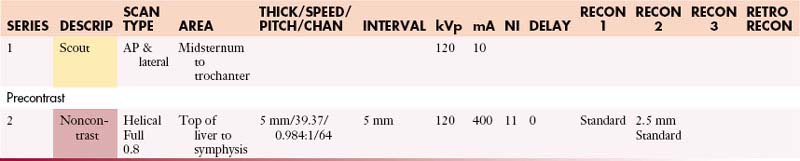
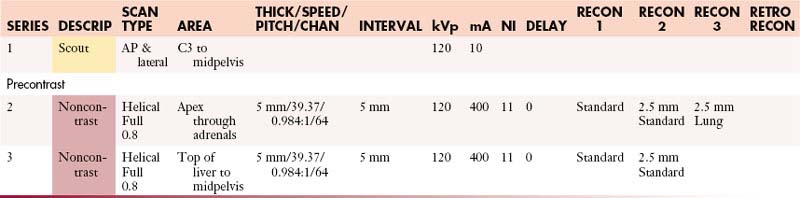
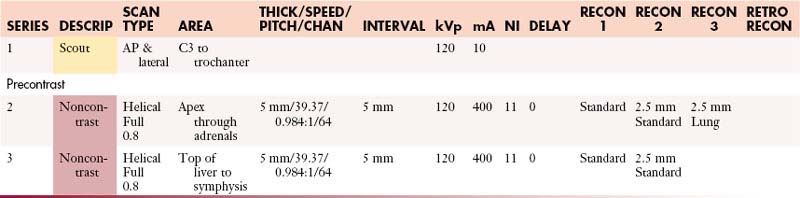
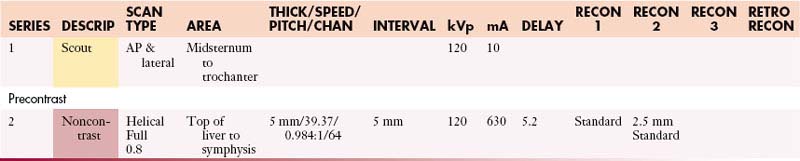
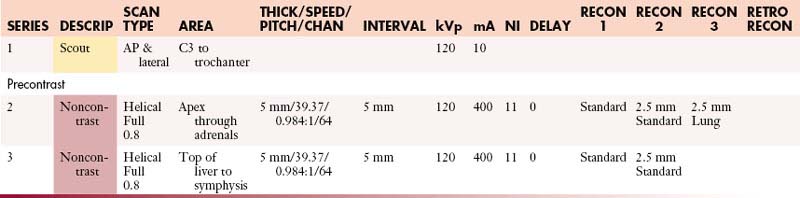
Abdomen and Pelvis without Contrast
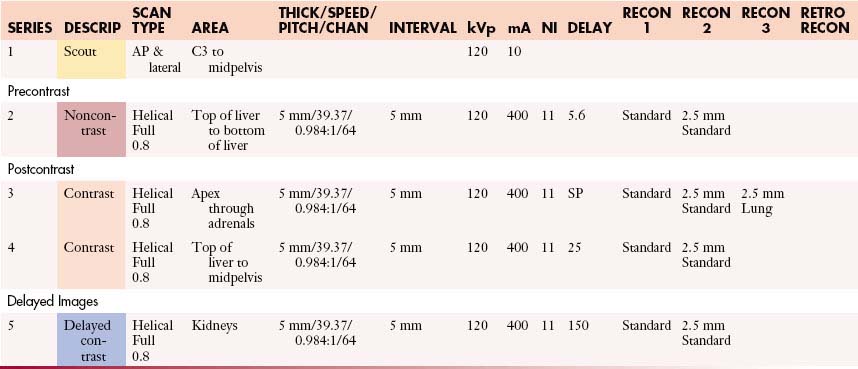
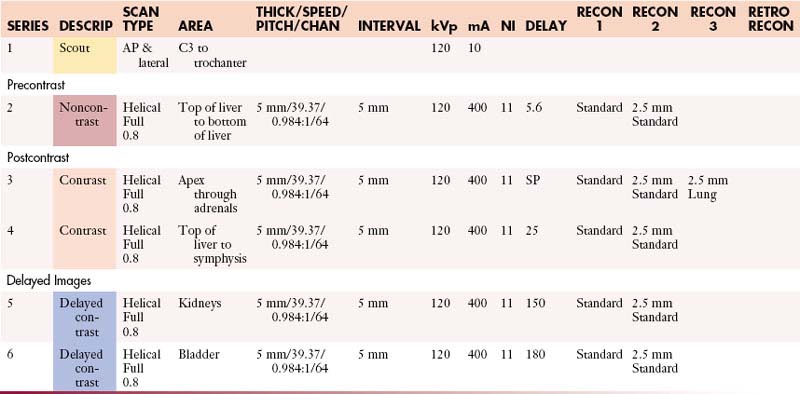
Abdomen and Pelvis without and with Contrast
Adrenals: Abdomen with Contrast
Adrenals: Abdomen without and with Contrast
Adrenals: Abdomen and Pelvis with Contrast
Adrenals: Abdomen and Pelvis without and with Contrast
Adrenals: Chest and Abdomen with Contrast
Adrenals: Chest and Abdomen without and with Contrast
Adrenals: Chest, Abdomen, and Pelvis with Contrast
Adrenals: Chest, Abdomen, and Pelvis without and with Contrast
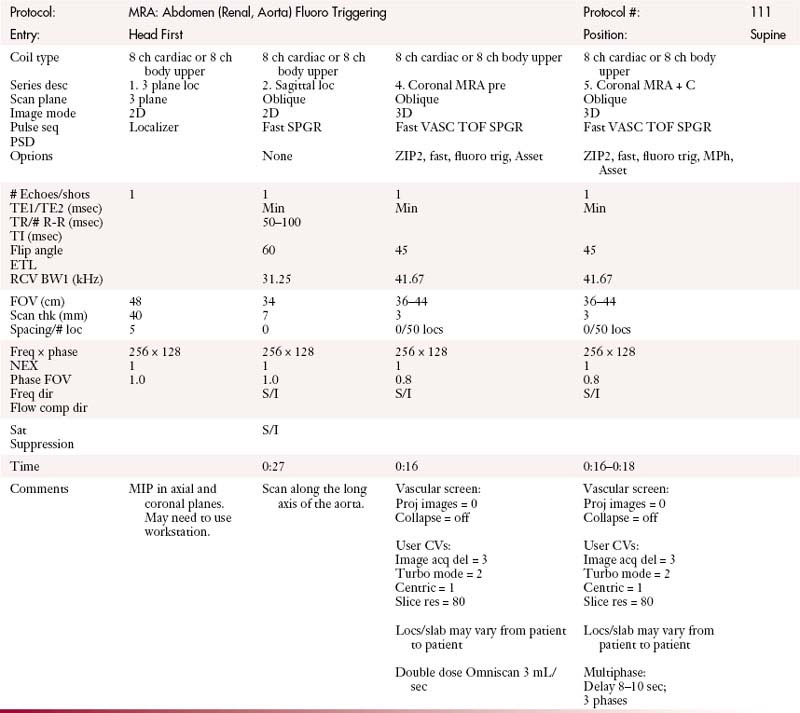
Angiogram/Venogram: Abdomen and Pelvis
Appendiceal/Peritoneal: Abdomen and Pelvis without and with Contrast
Appendiceal/Peritoneal: Chest, Abdomen, and Pelvis without and with Contrast
Bowel Carcinoid: Abdomen and Pelvis without and with Contrast
Chest and Abdomen with Contrast
Chest and Abdomen without Contrast
Chest and Abdomen without and with Contrast
Chest, Abdomen, and Pelvis with Contrast
Chest, Abdomen, and Pelvis without Contrast
Chest, Abdomen, and Pelvis without and with Contrast
Gastric: Abdomen and Pelvis without and with Contrast
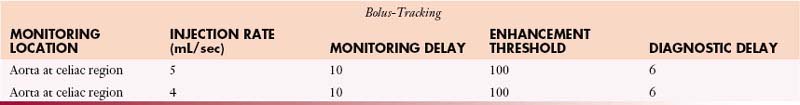
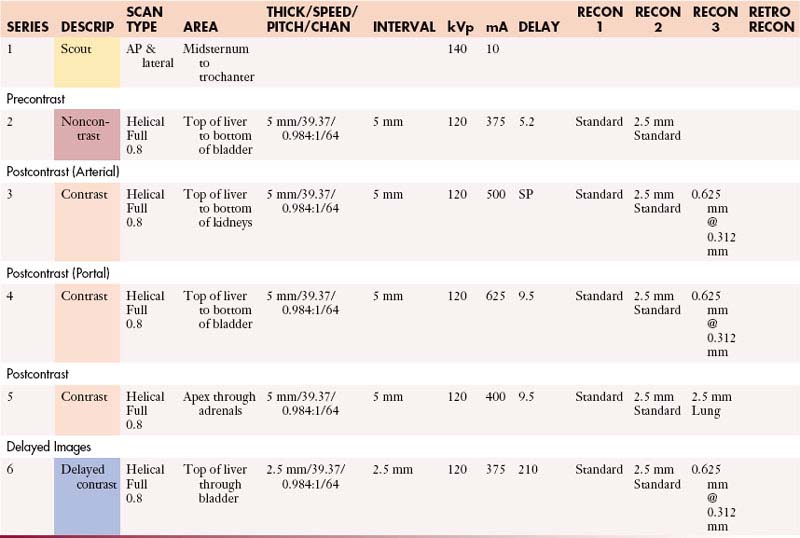
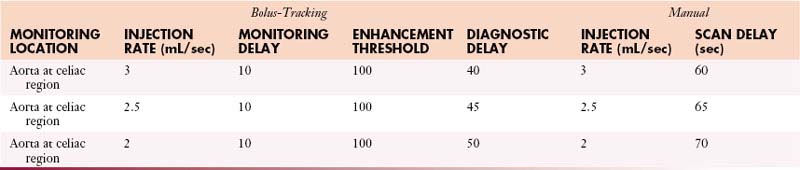
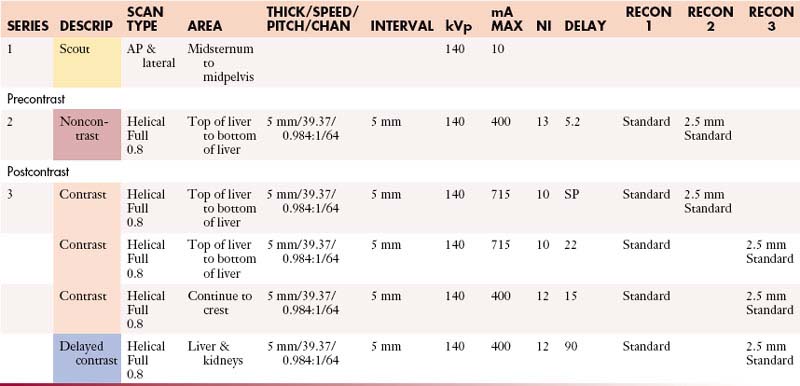
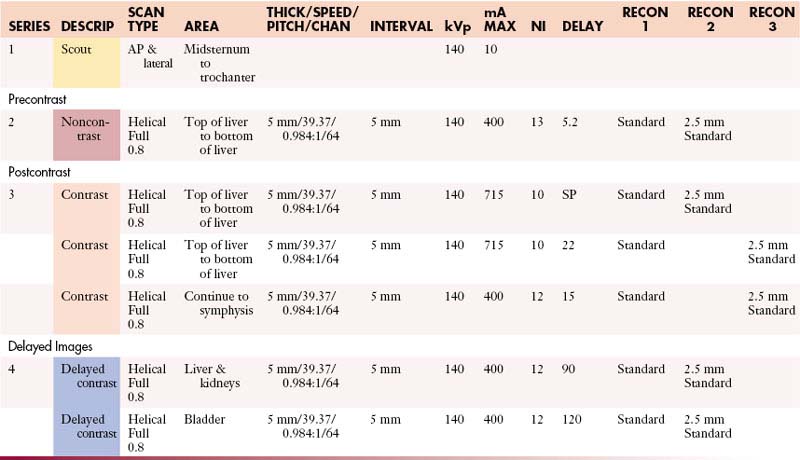
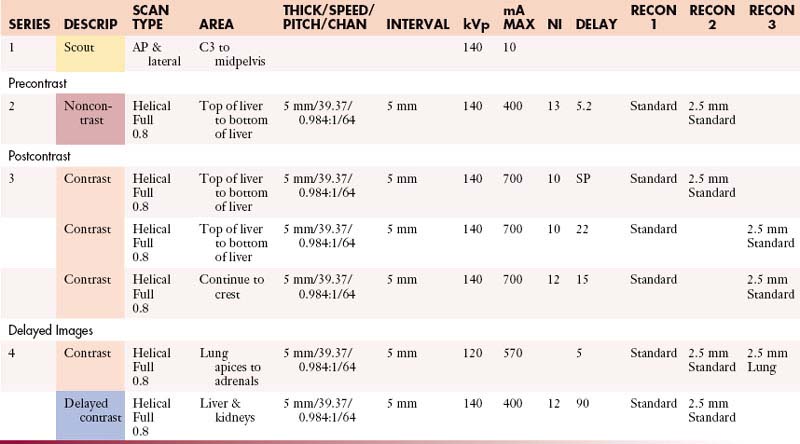
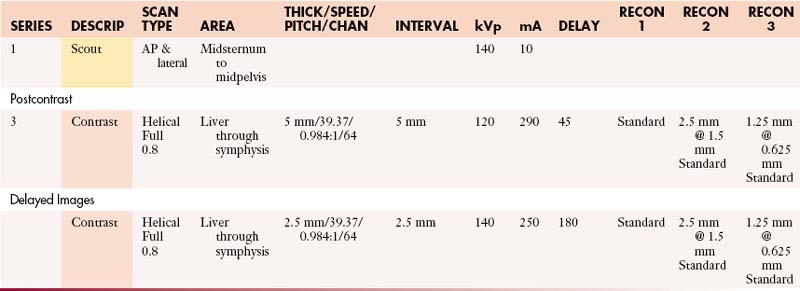
Liver: Abdomen without and with Contrast
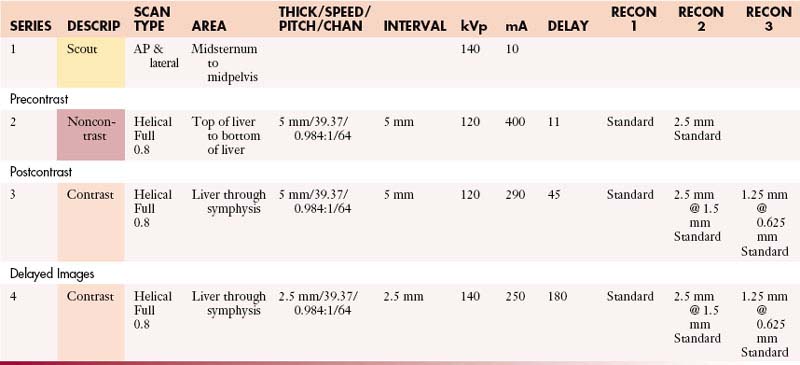
Liver: Abdomen and Pelvis without and with Contrast
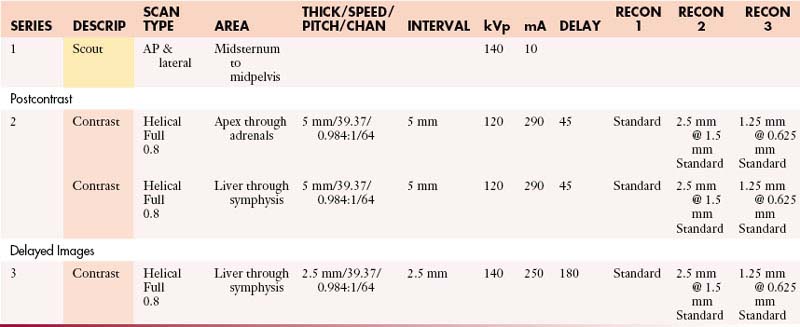
Liver: Chest and Abdomen without and with Contrast
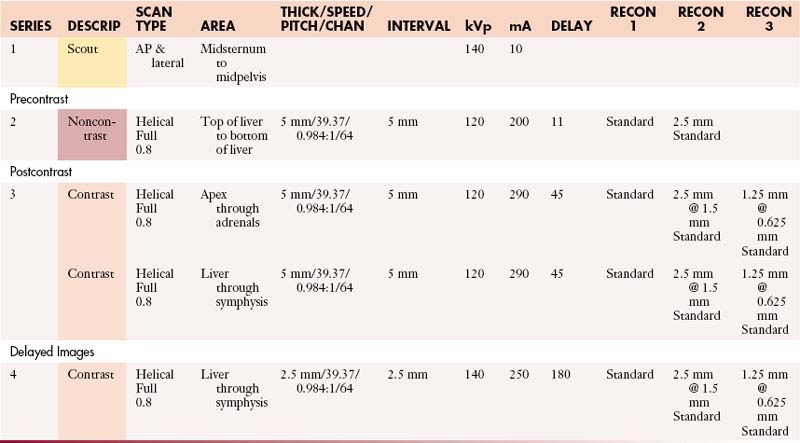
Liver: Chest, Abdomen, and Pelvis without and with Contrast
Lymphoma without and with Contrast
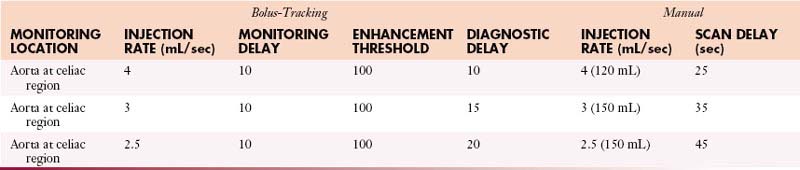
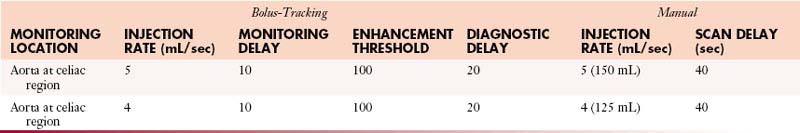
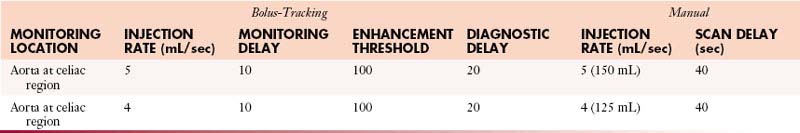
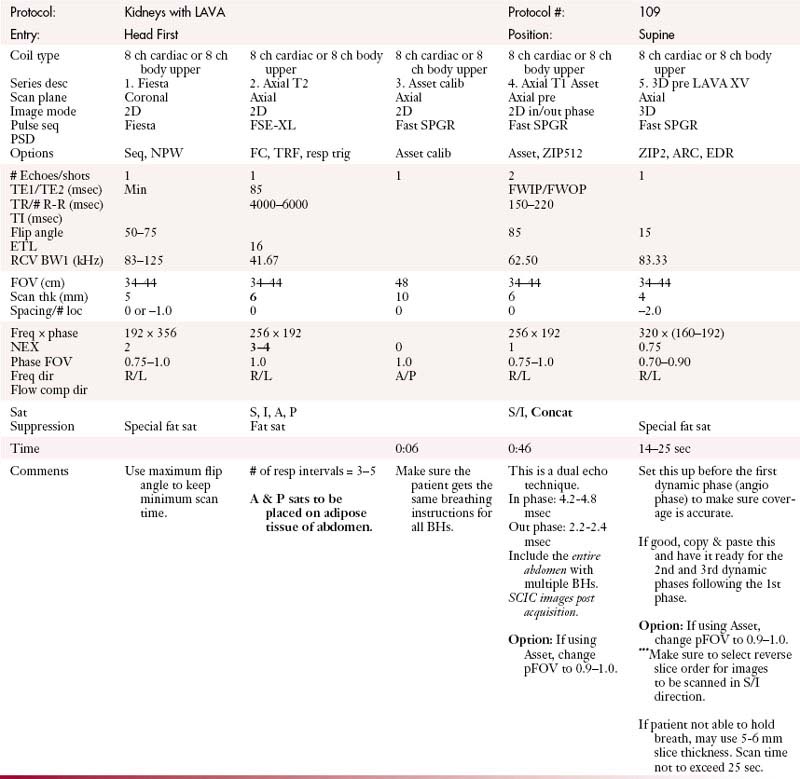
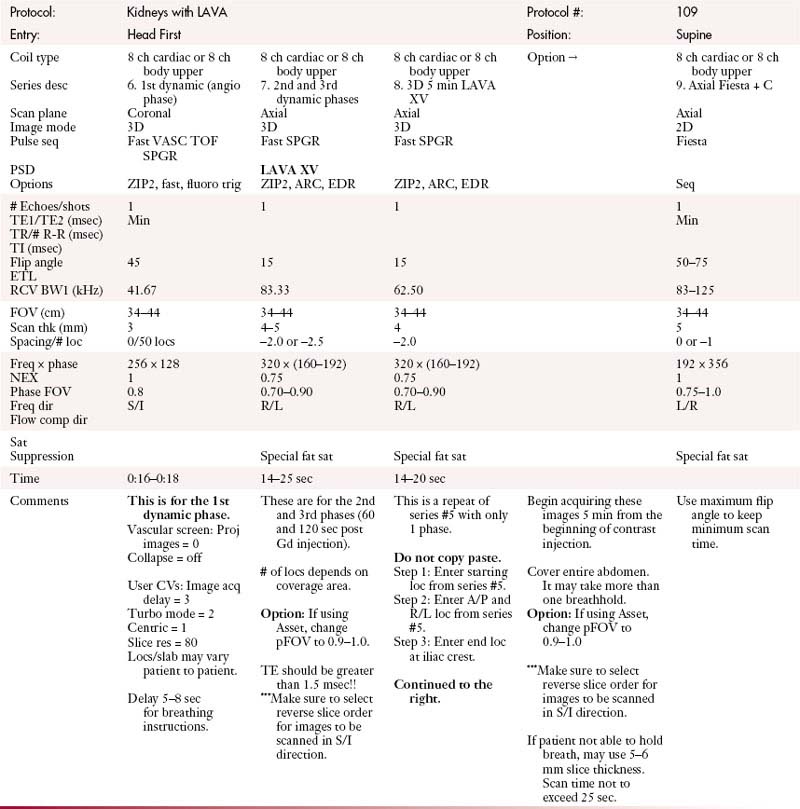
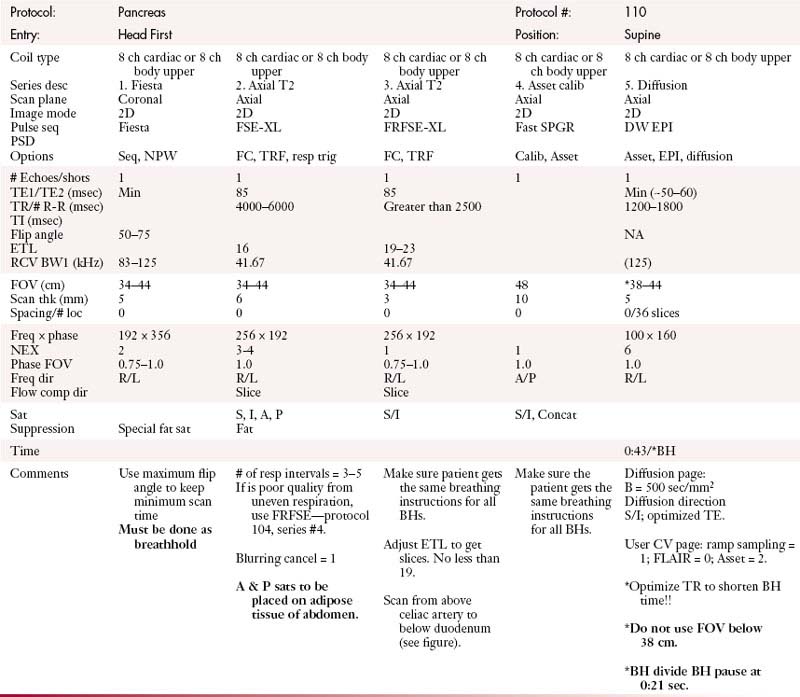
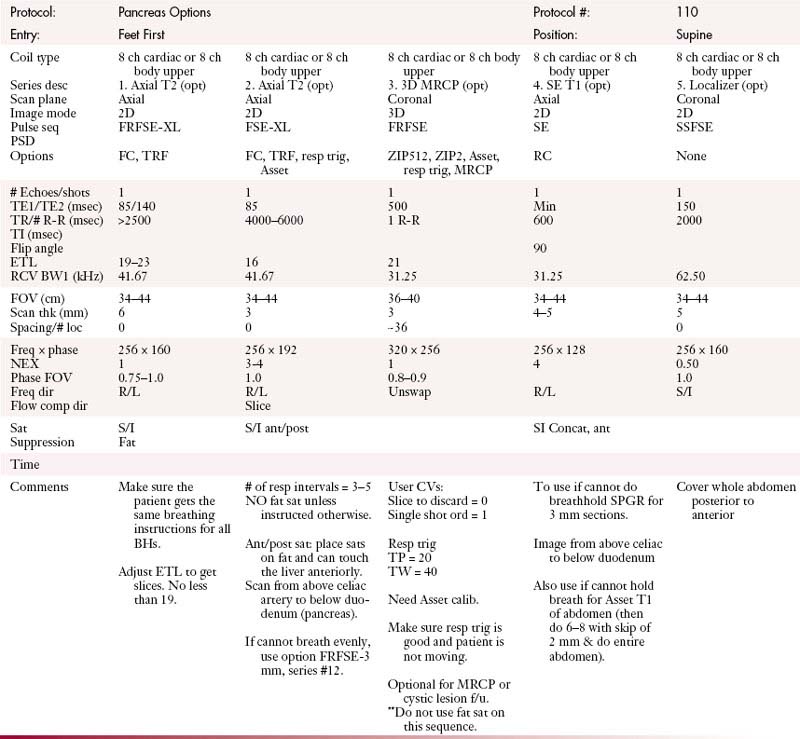
Pancreas: Abdomen without and with Contrast
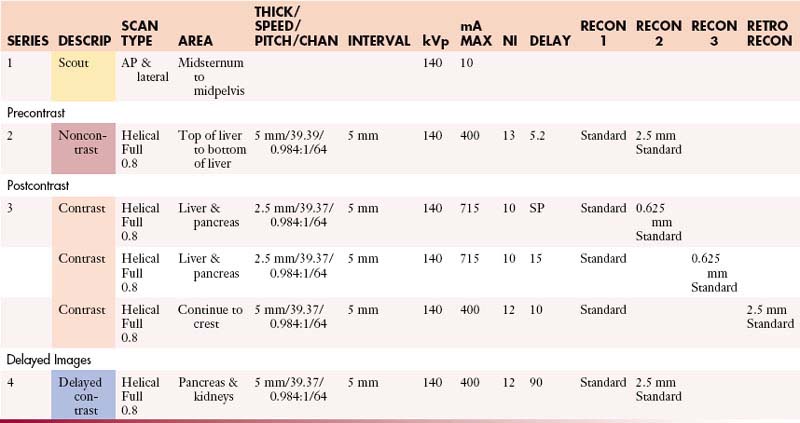
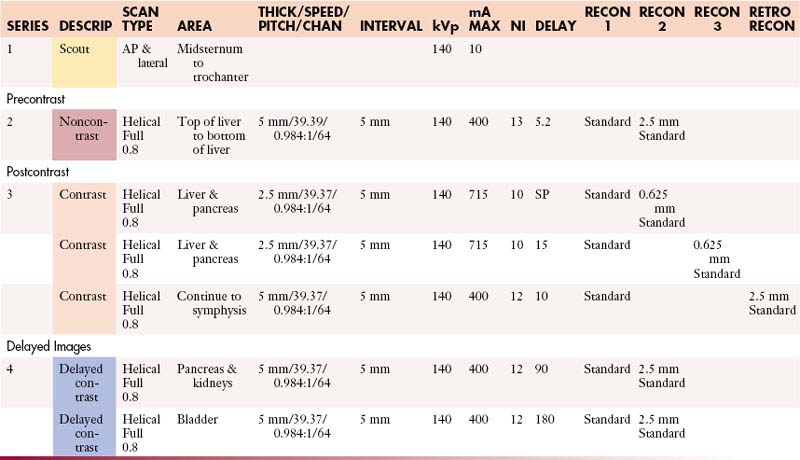
Pancreas: Abdomen and Pelvis without and with Contrast
Pancreas: Chest, Abdomen, and Pelvis without and with Contrast
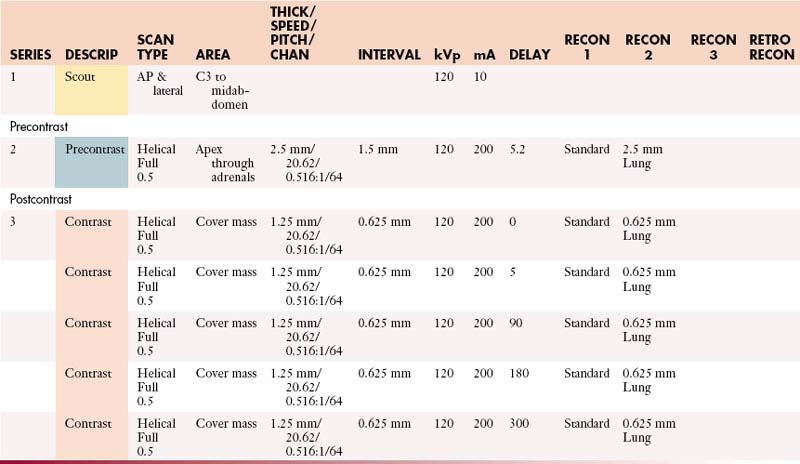
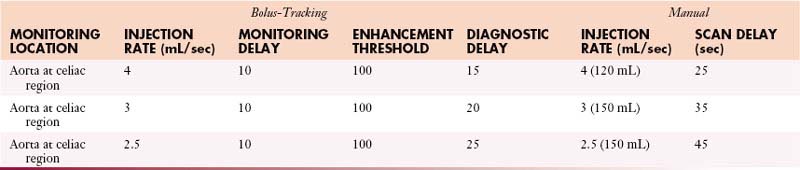
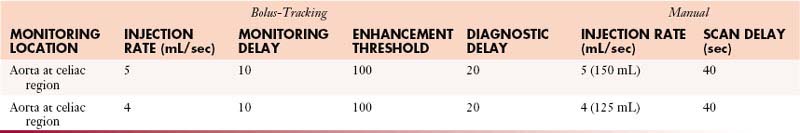
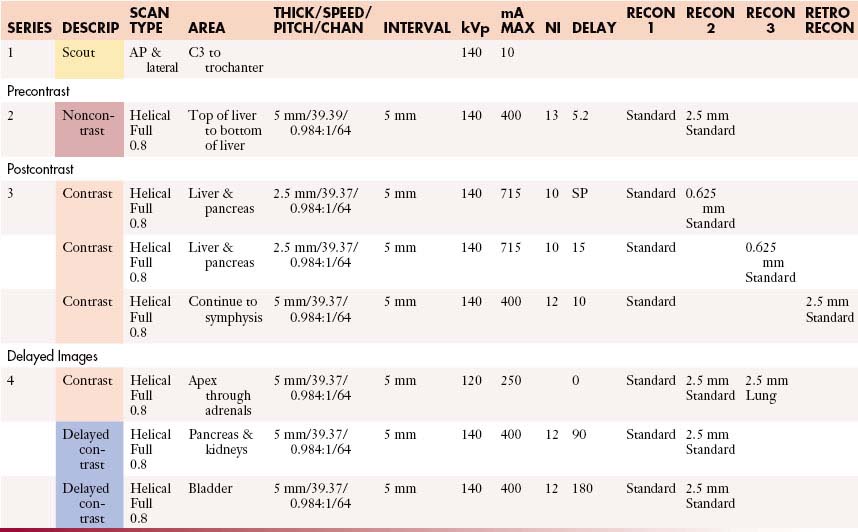
Pancreatic Islet Cell: Abdomen without and with Contrast
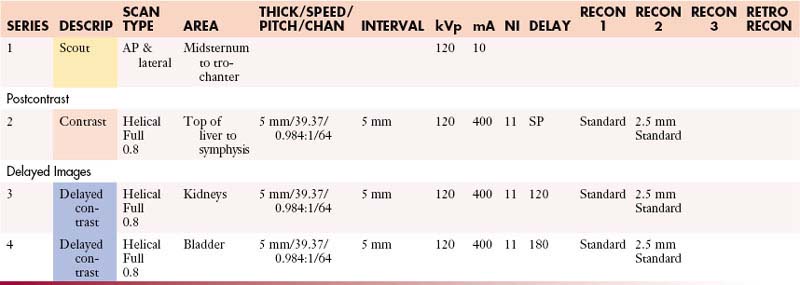
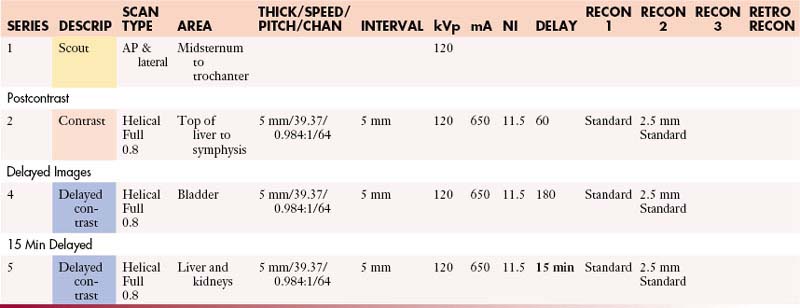
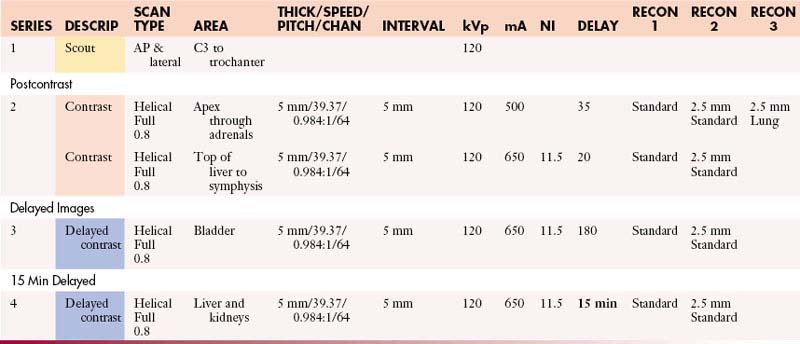
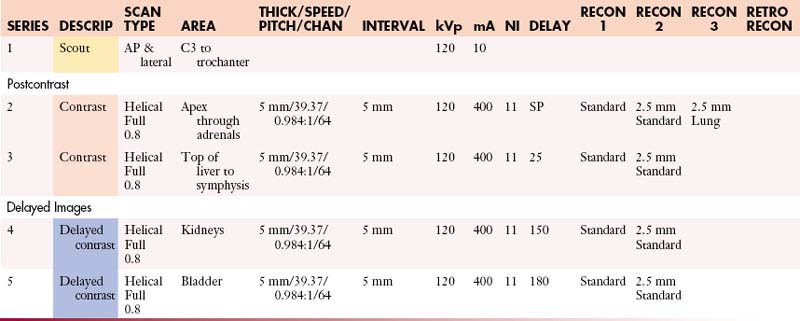
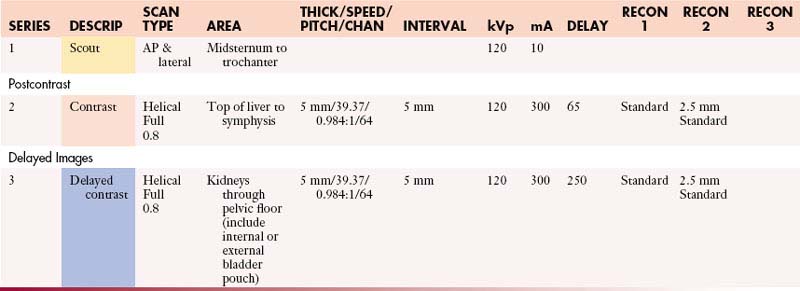
Post Cystectomy: Abdomen and Pelvis with Contrast
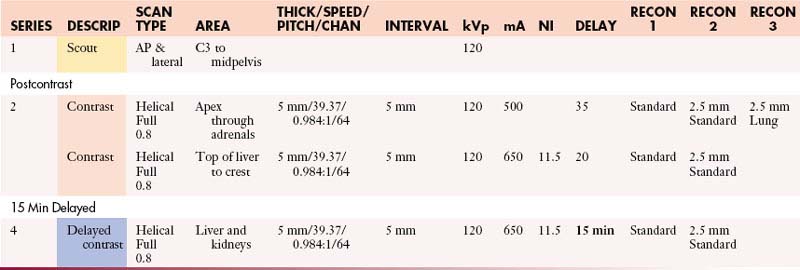
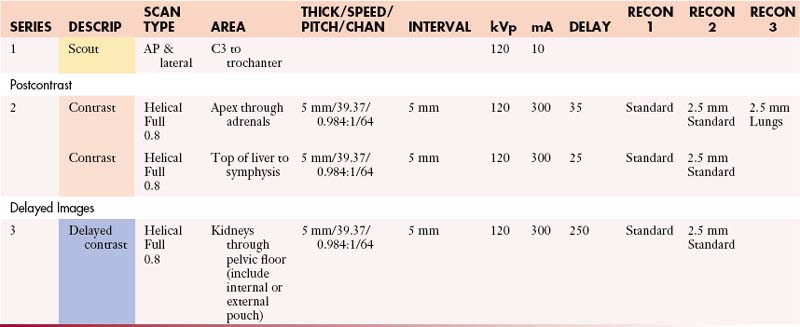
Post Cystectomy: Chest, Abdomen, and Pelvis with Contrast
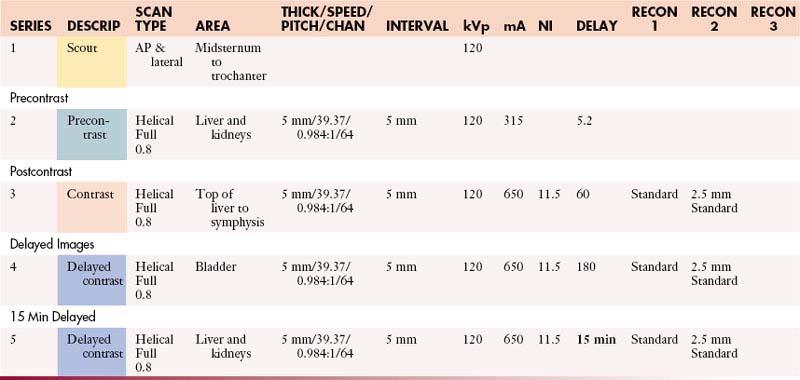
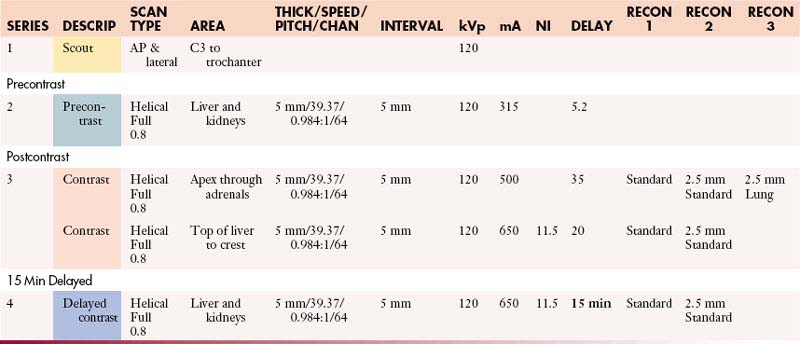
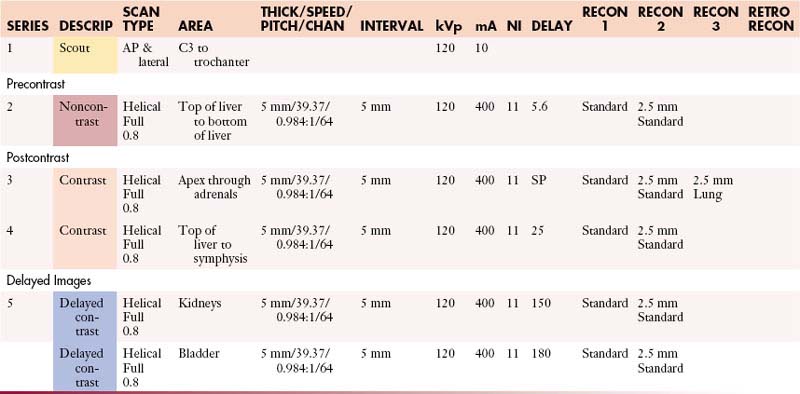
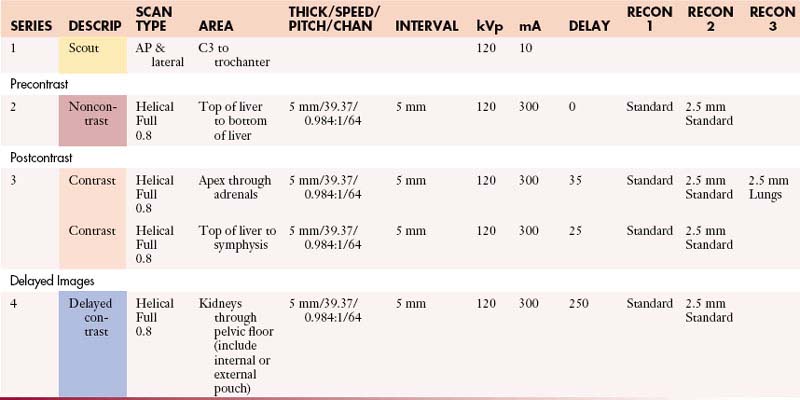
Post Cystectomy: Chest, Abdomen, and Pelvis without and with Contrast
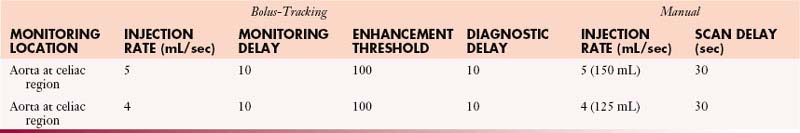
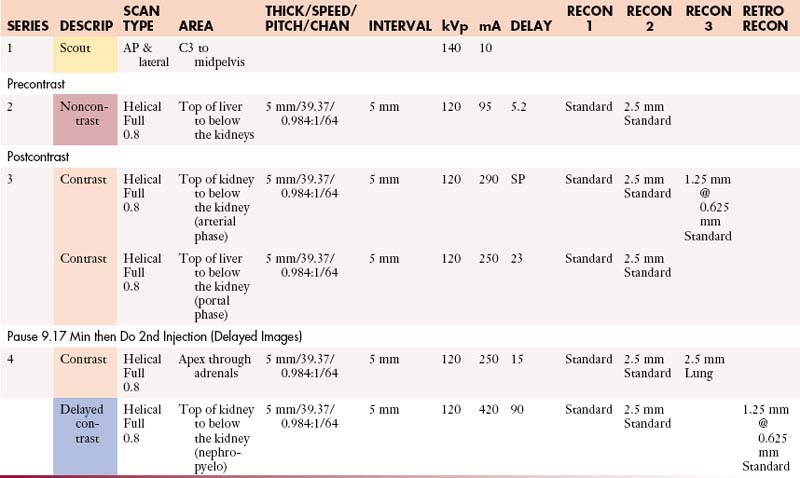
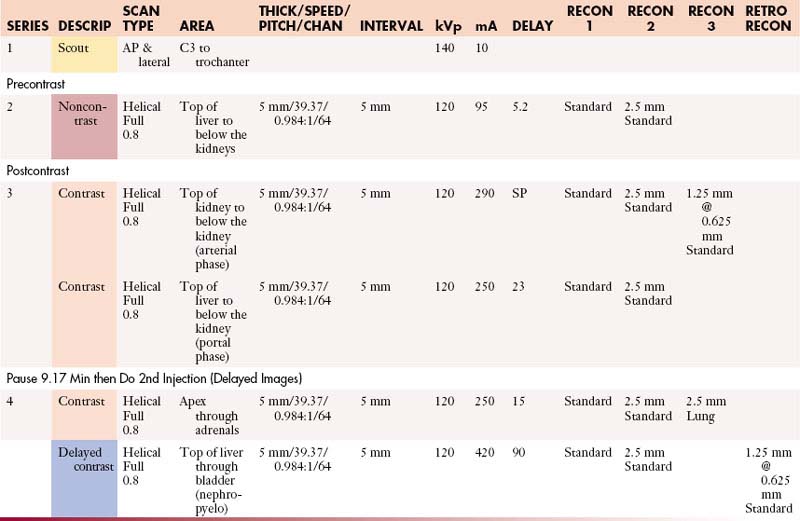
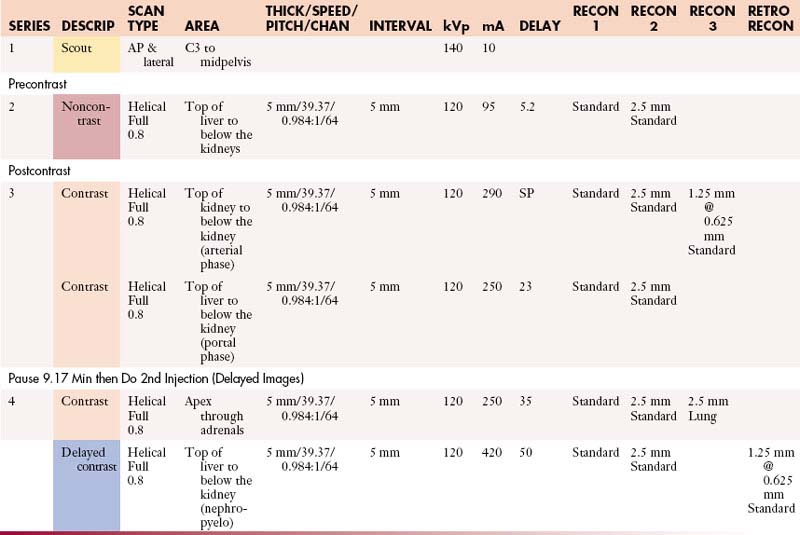
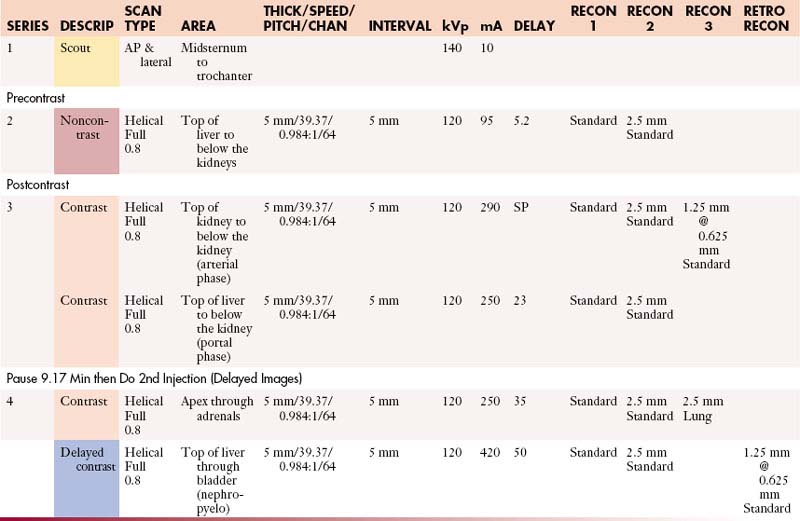
Renal: Chest and Abdomen without and with Contrast
Renal: Chest, Abdomen, and Pelvis without and with Contrast
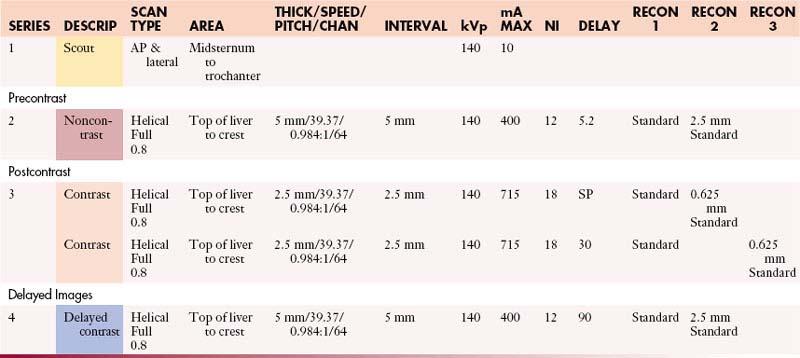
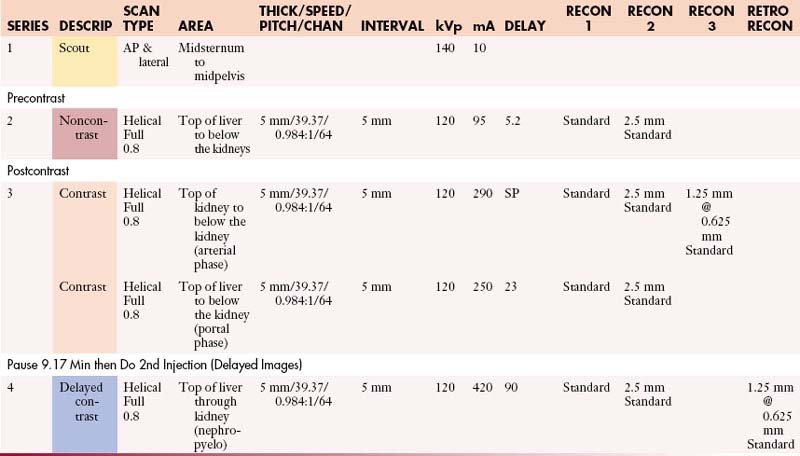
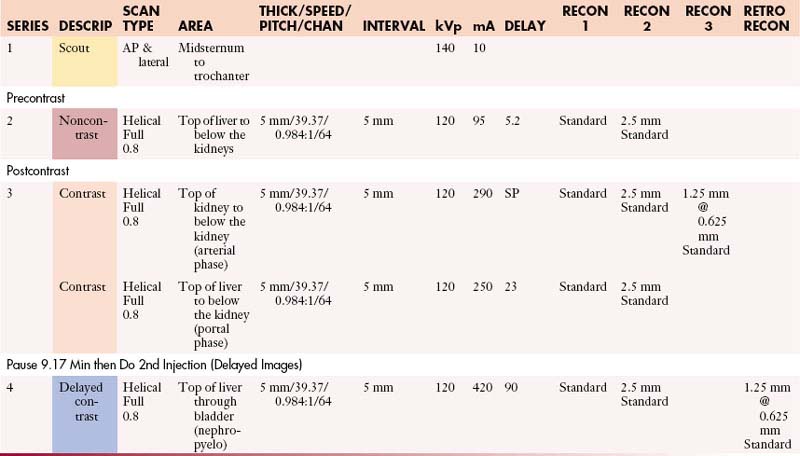
Renal + 3D: Abdomen without and with Contrast
Renal + 3D: Abdomen and Pelvis without and with Contrast
Renal + 3D: Chest and Abdomen without and with Contrast
Renal + 3D: Chest, Abdomen, and Pelvis without and with Contrast
Enterography (Small Bowel): Abdomen and Pelvis with Contrast
Enterography (Small Bowel): Abdomen and Pelvis without and with Contrast
Enterography (Small Bowel): Chest, Abdomen, and Pelvis with Contrast
Enterography (Small Bowel): Chest, Abdomen, and Pelvis without and with Contrast
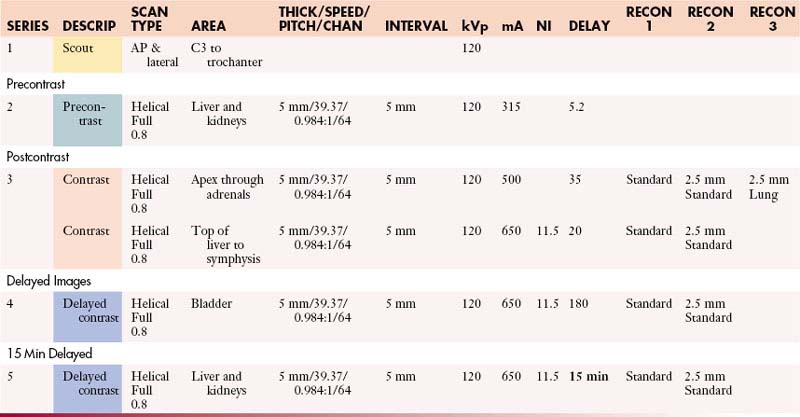
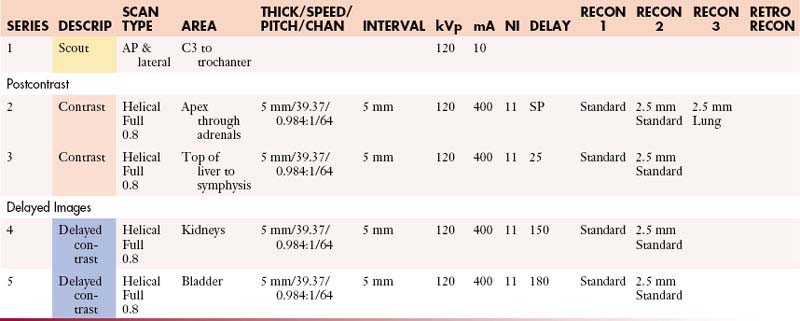
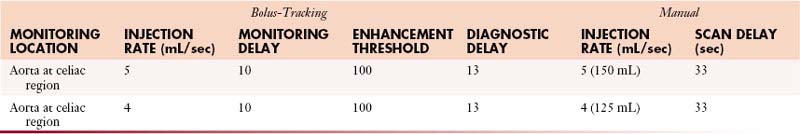
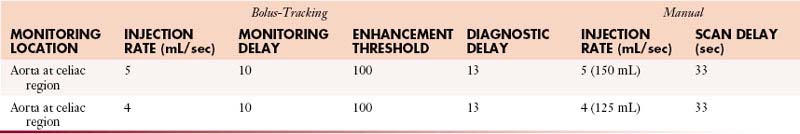
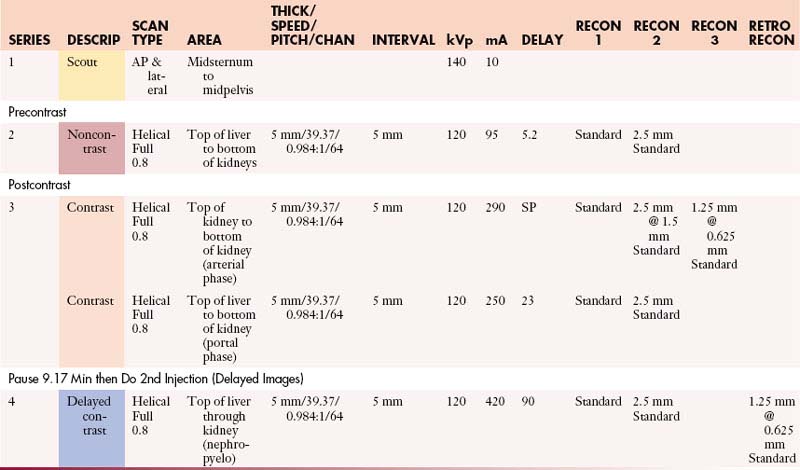
Urogram: Abdomen and Pelvis without and with Contrast
Urogram: Chest, Abdomen, and Pelvis without and with Contrast
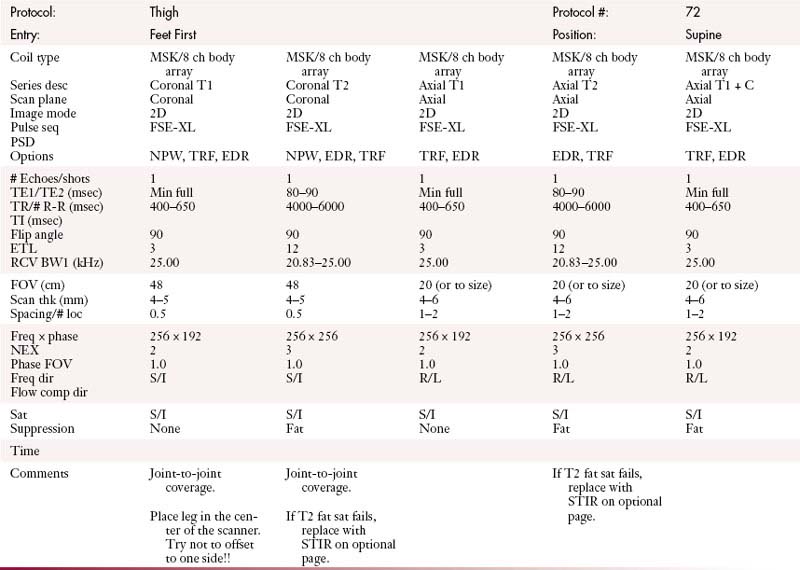
Musculoskeletal (MSK) Protocols (MDCT 64 Slice)
MSK (Bridging Protocol) with Contrast
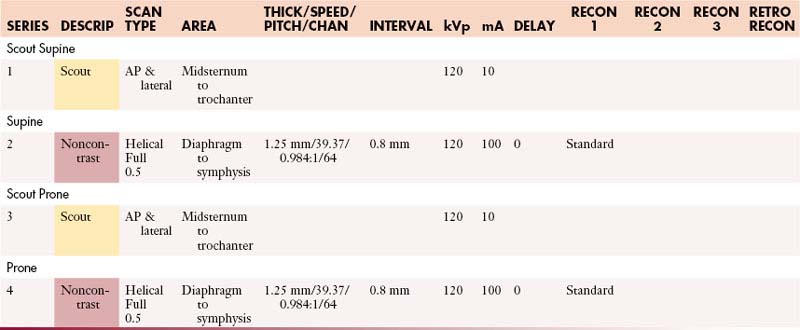
MSK (Bridging Protocol) without Contrast
MSK (Metal Protocol) with Contrast
MSK (Metal Protocol) without Contrast
MSK Operating Room Hi-Res Protocol (64 Slice)
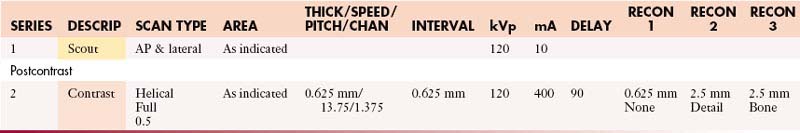
Operating Room High-Res Protocol with Contrast
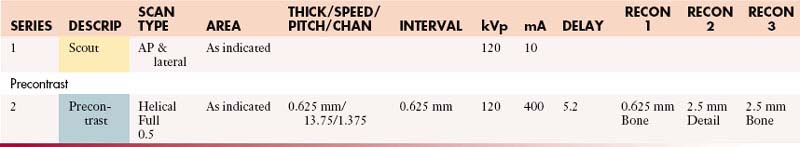
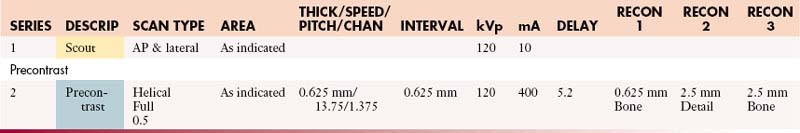
Operating Room High-Res Protocol without Contrast
Operating Room Standard Protocol (64 Slice)
Operating Room Standard Protocol with Contrast
Operating Room Standard Protocol without Contrast
MSK (Soft Tissue Protocol) with Contrast
MSK (Soft Tissue Protocol) without Contrast
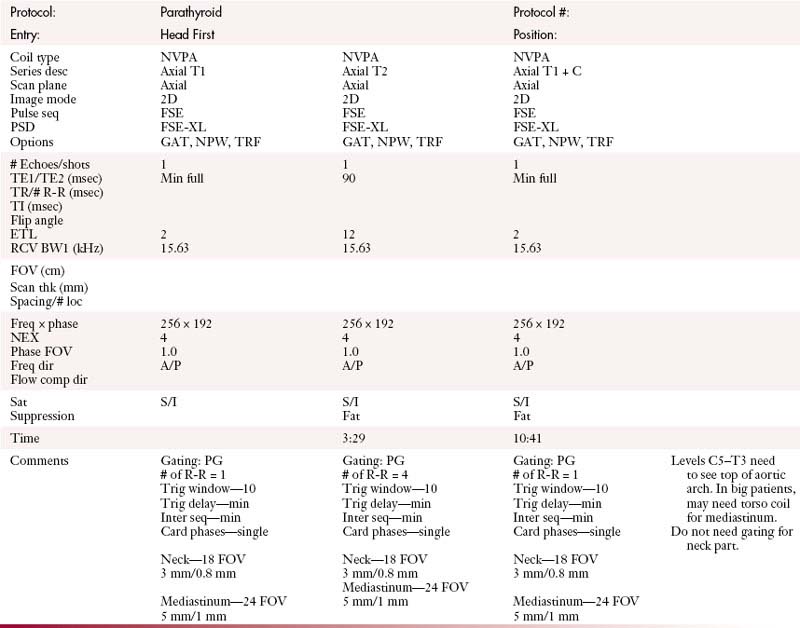
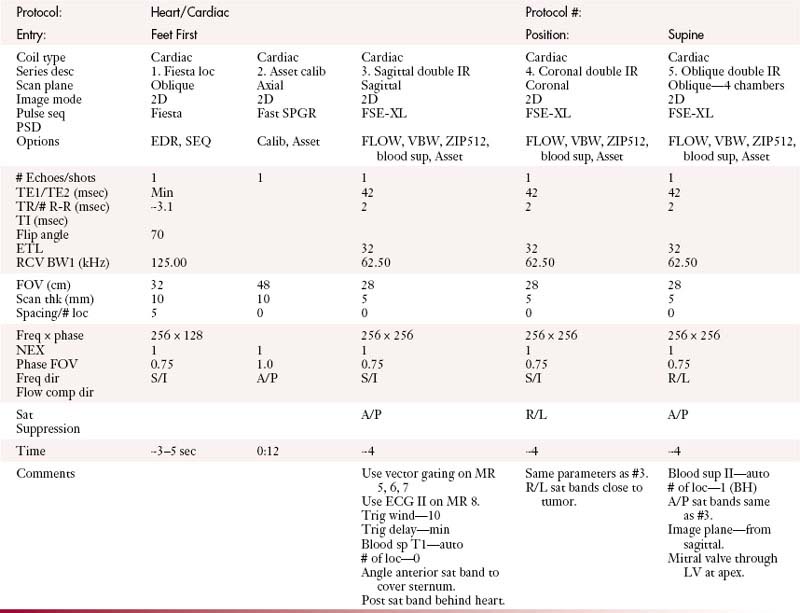
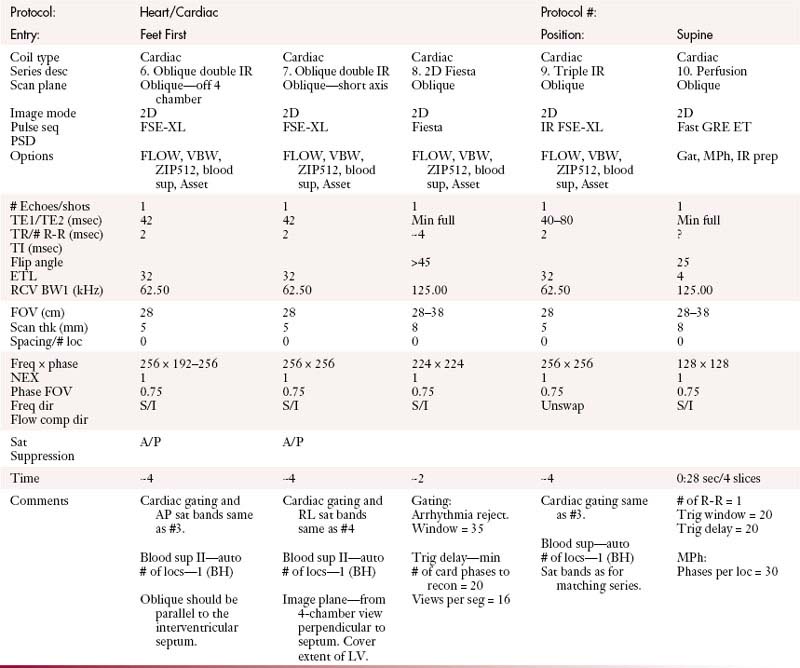
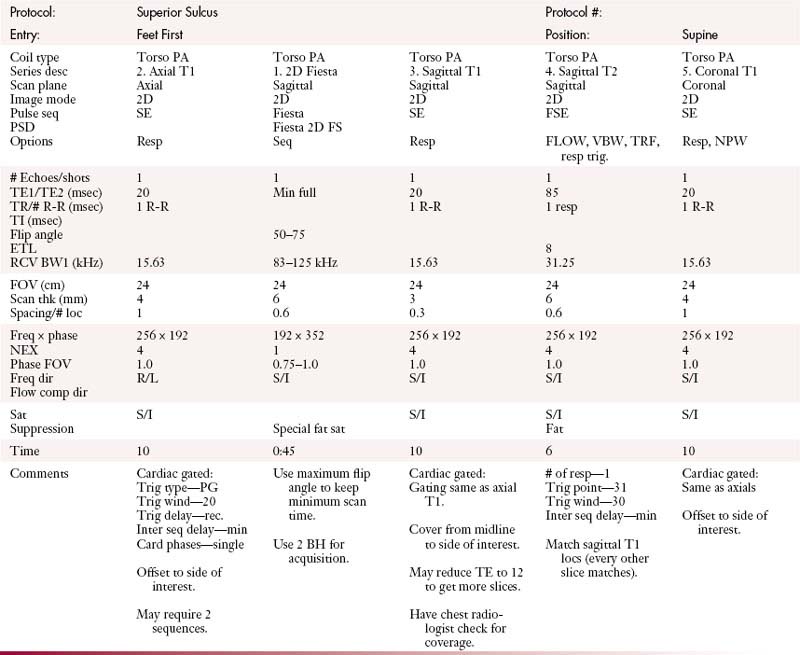
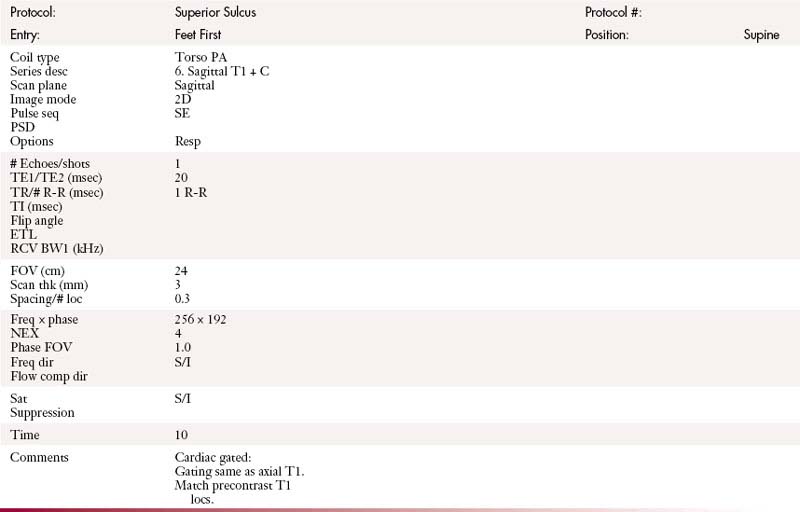
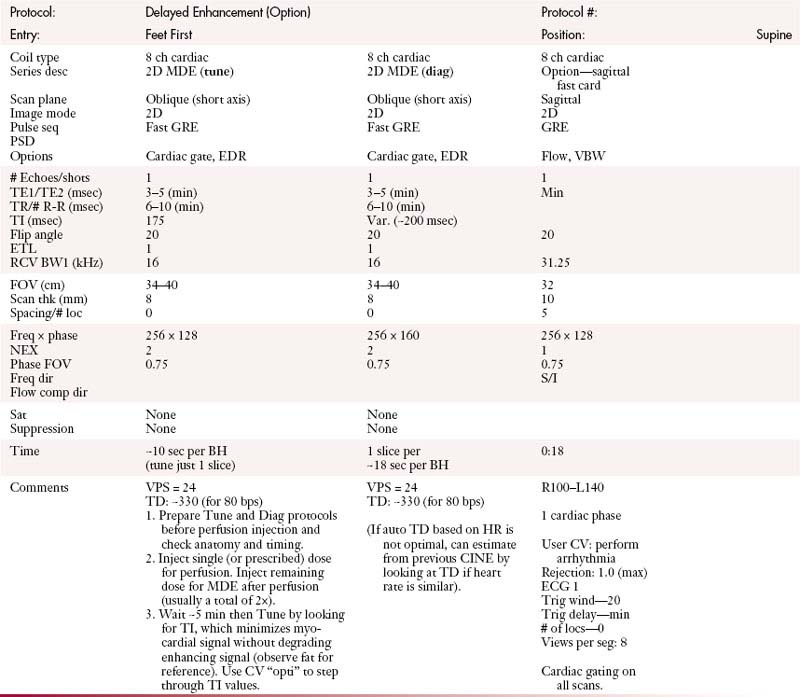
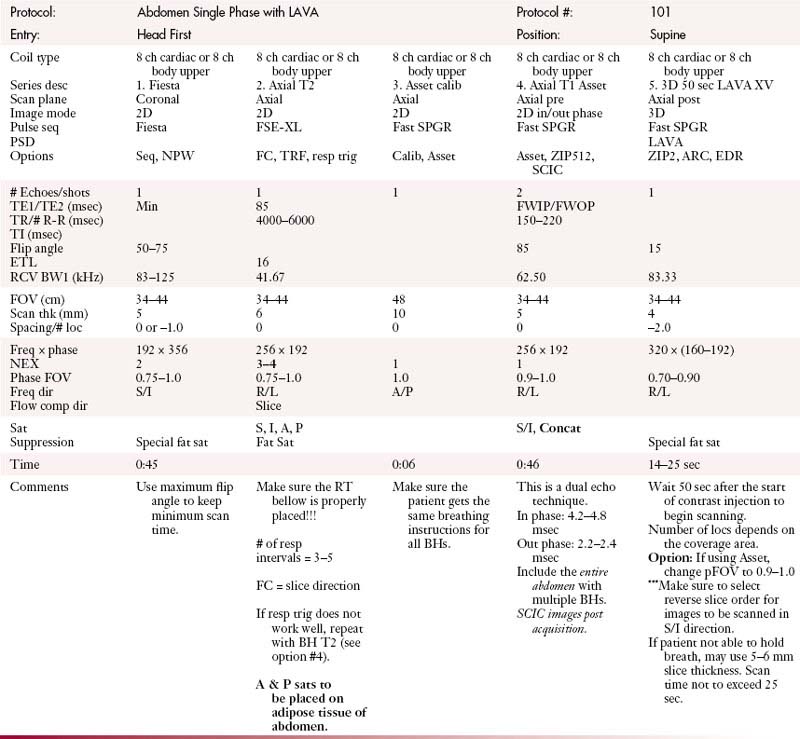
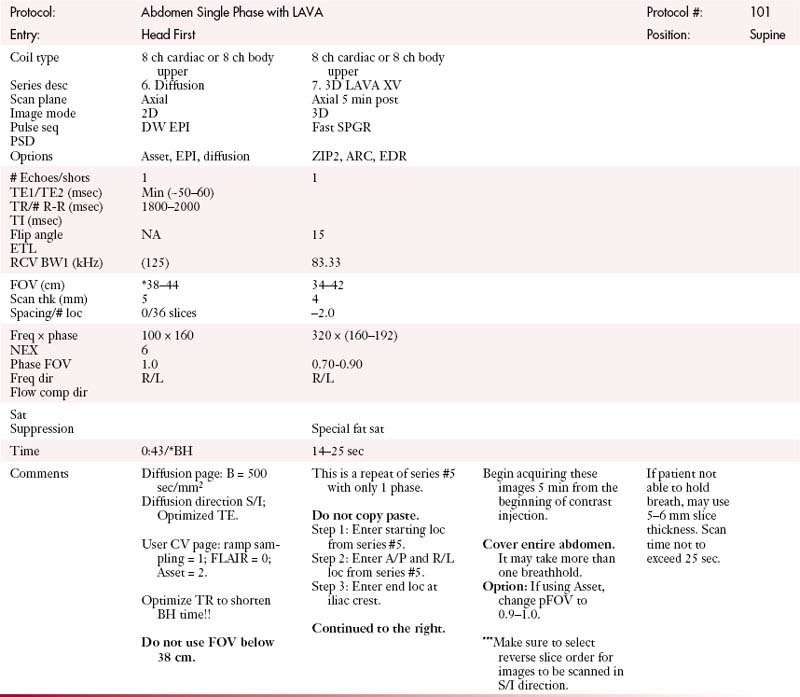
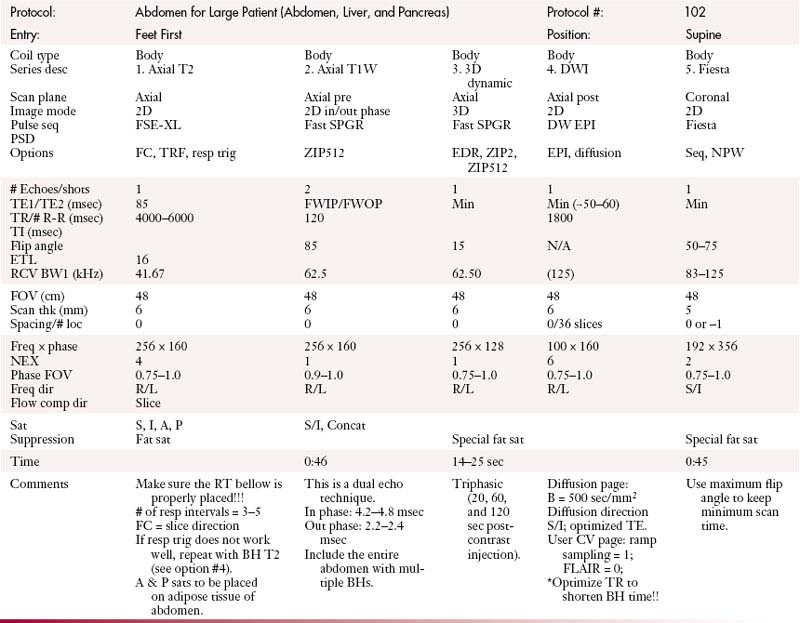
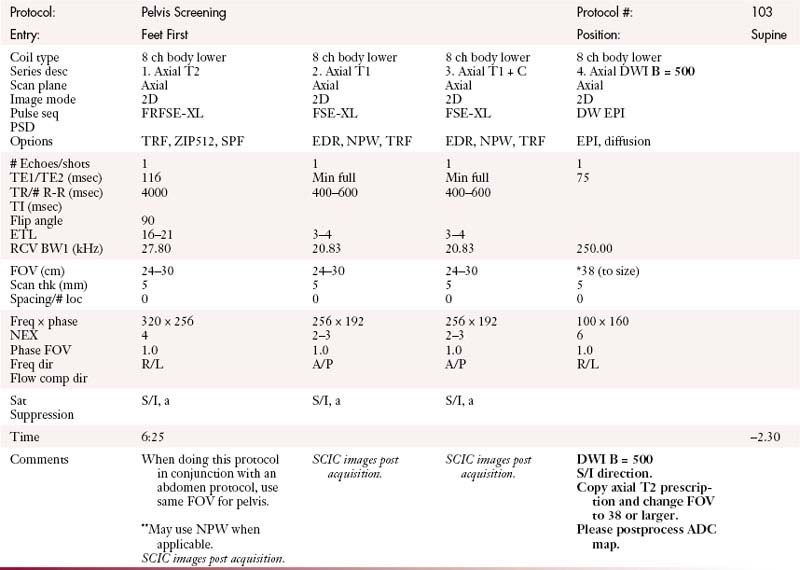
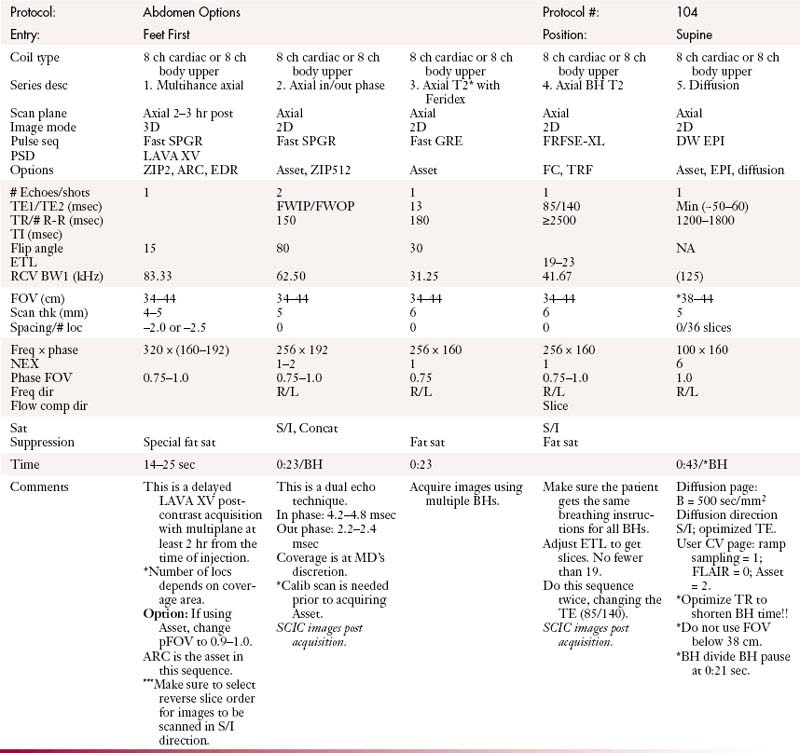
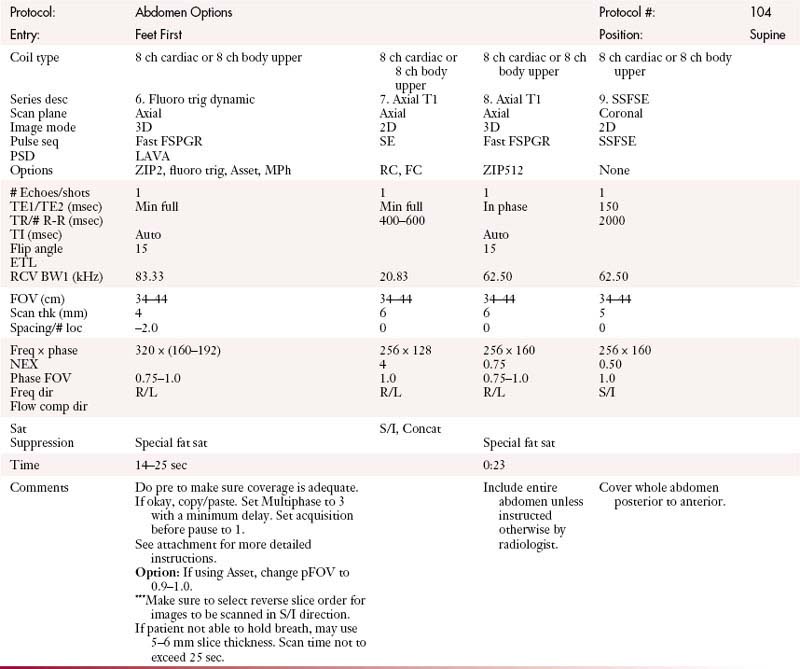
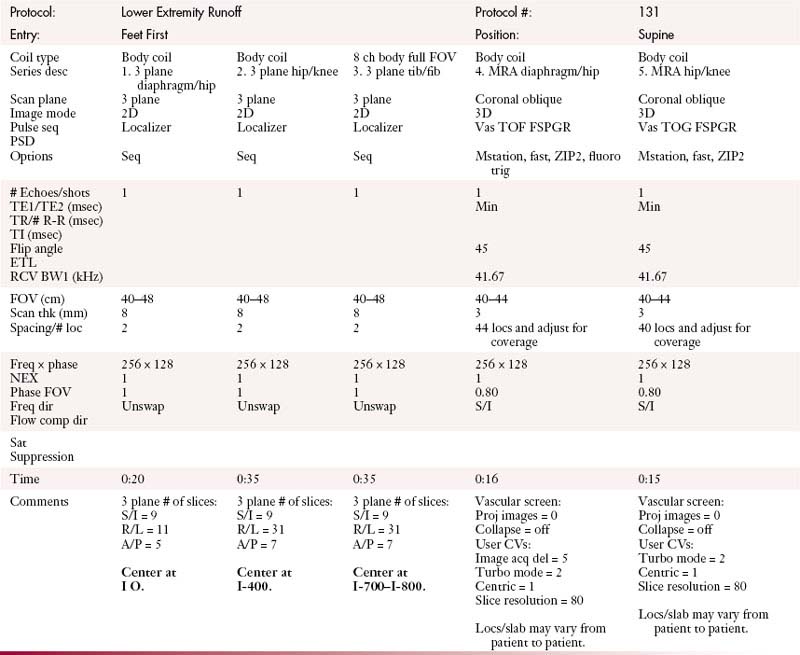
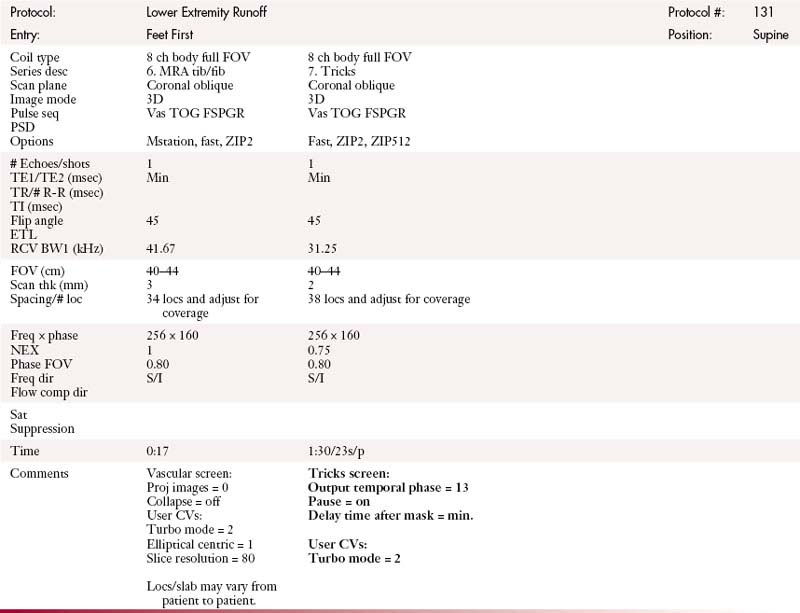
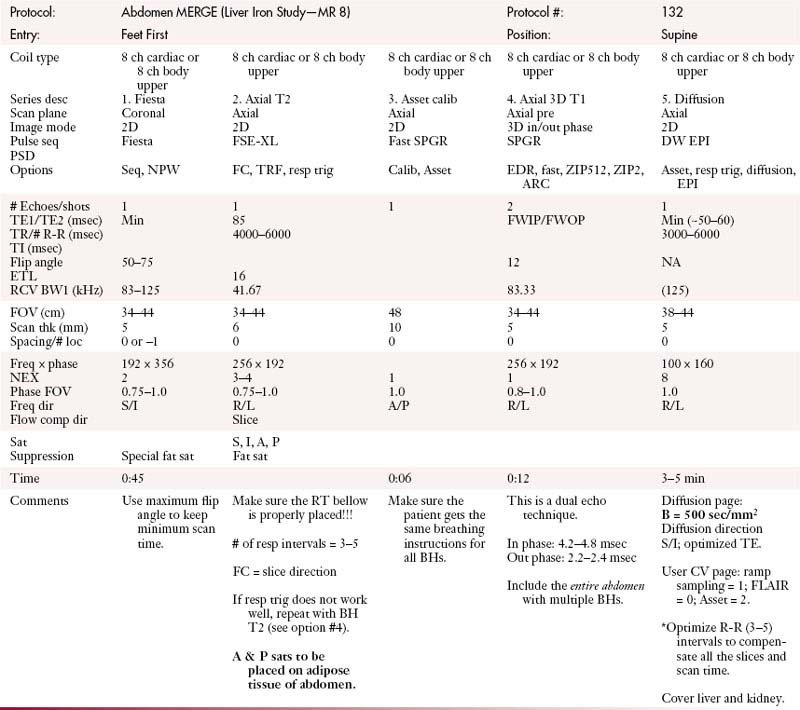
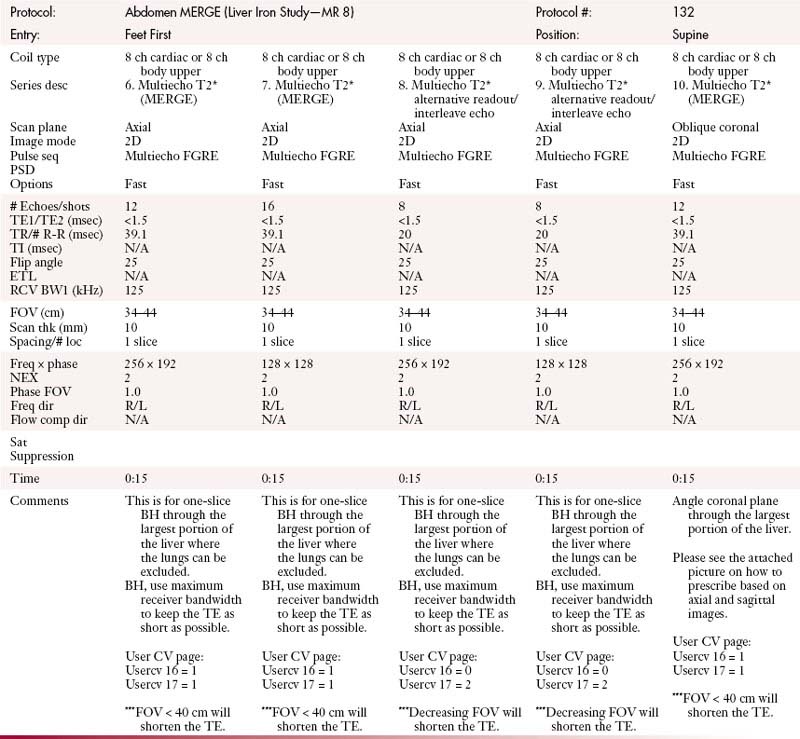
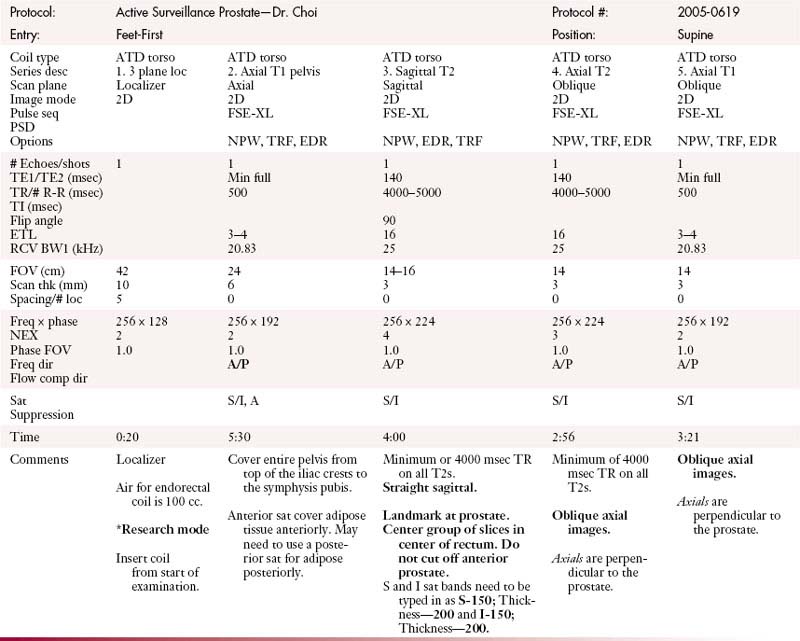
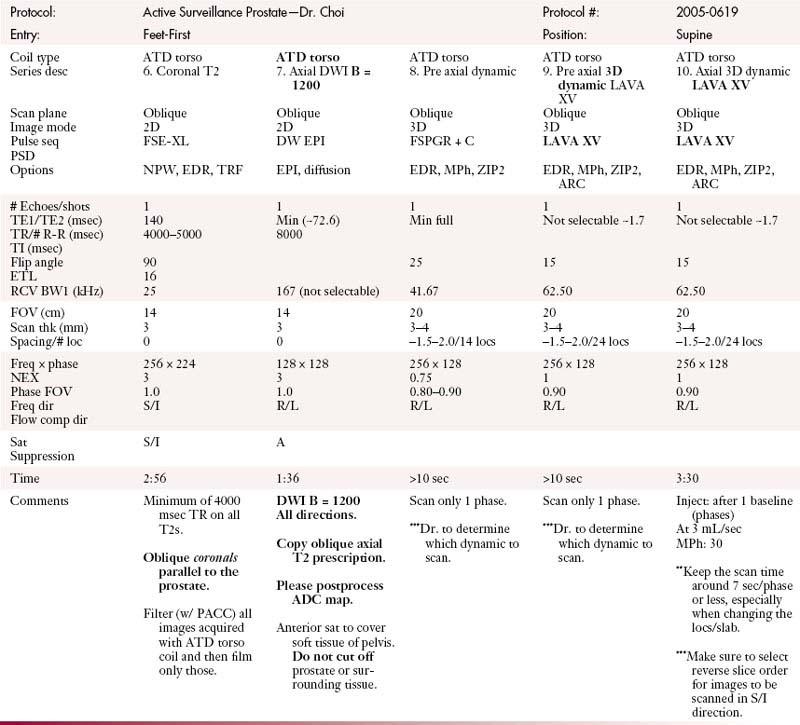
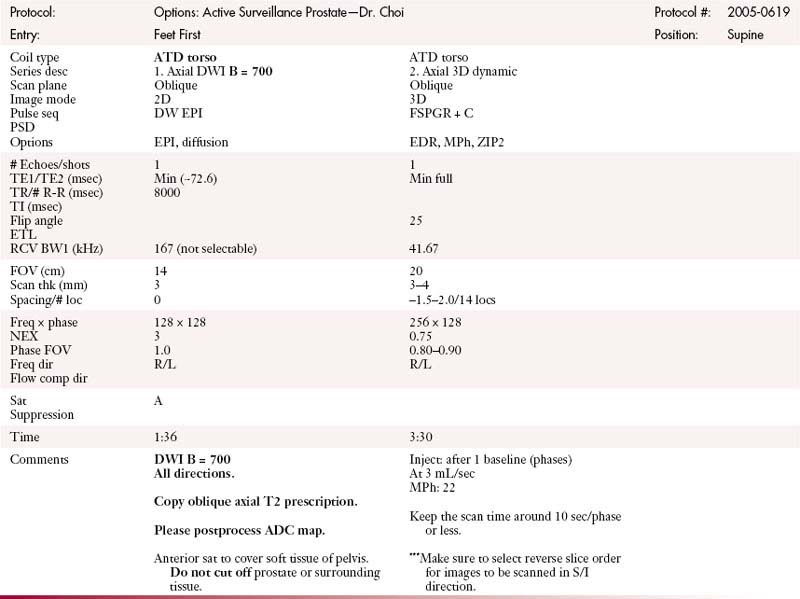
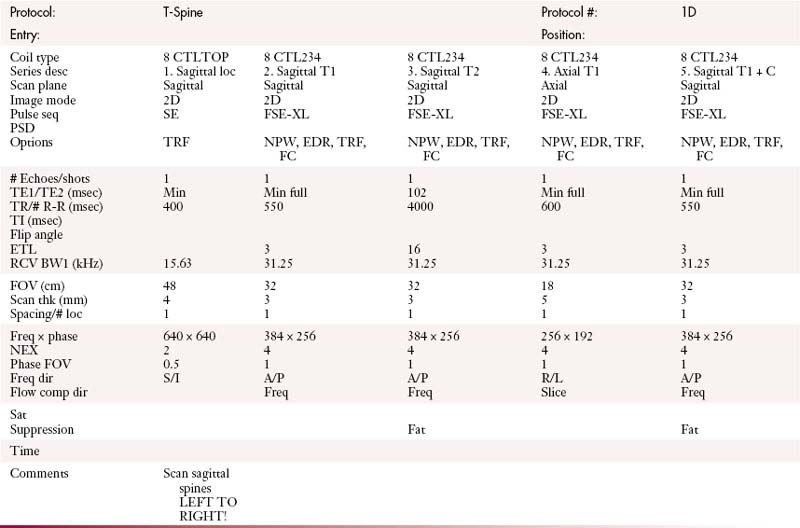
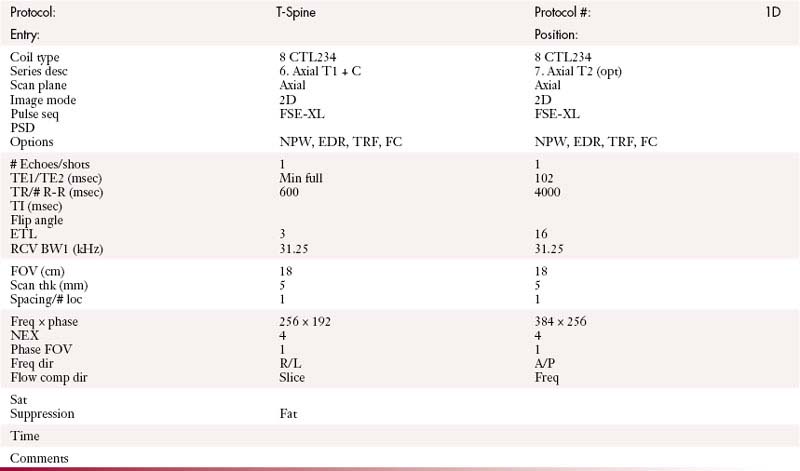
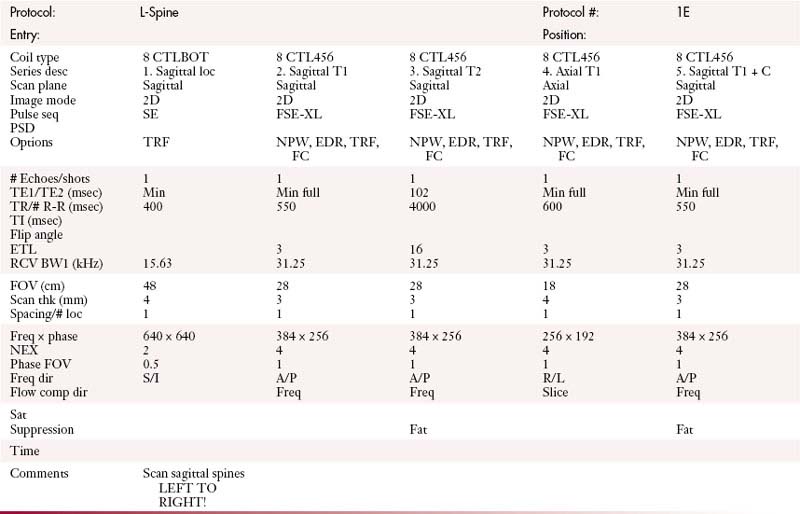
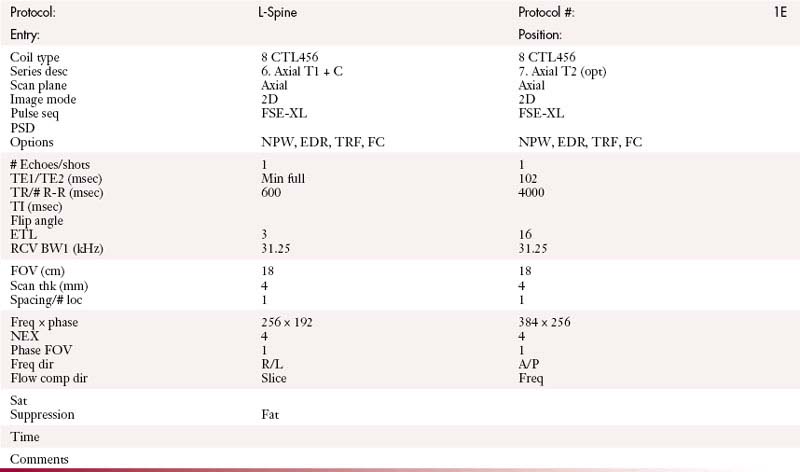
MRI Protocols
MDCT: CT Imaging
Chest Protocols (MDCT 64 Slice)
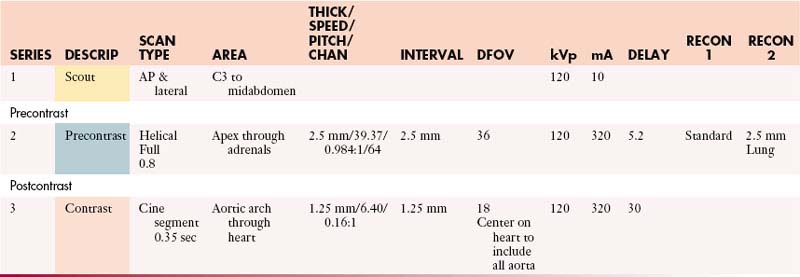
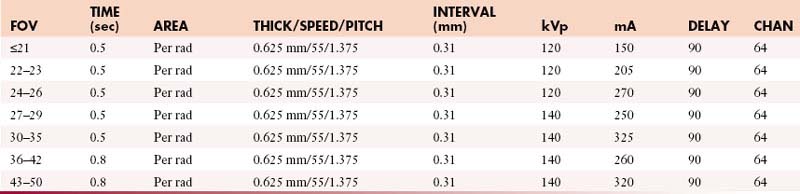
Aorta (Gated Study)
IV Contrast: Iso-osmolar and saline
| ISO-OSMOLAR (mL/sec) | SALINE (mL/sec) | SCAN DELAY (sec) |
|---|---|---|
| 5 | 5 | 30 |
Coronal: 2.5 mm @ 0.8 mm or default—standard algorithm
Sagittal: 2.5 mm @ 0.8 mm or default—lung algorithm
Oblique-sagittal: 0.8 mm @ 2.5 mm default—standard algorithm (candy cane view)
Scanning direction from superior to inferior.
Check heart rate on arrival. Call radiologist for heart rate > 70 bpm.
Select postcontrast pitch and FOV based on heart rate and patient size.
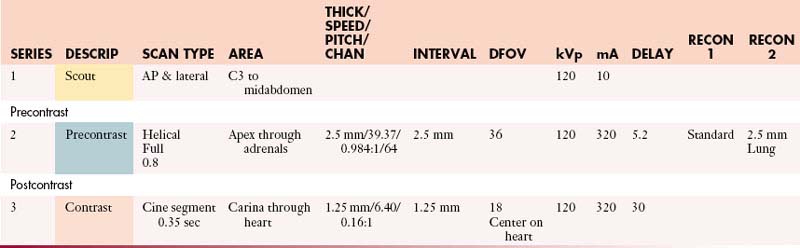
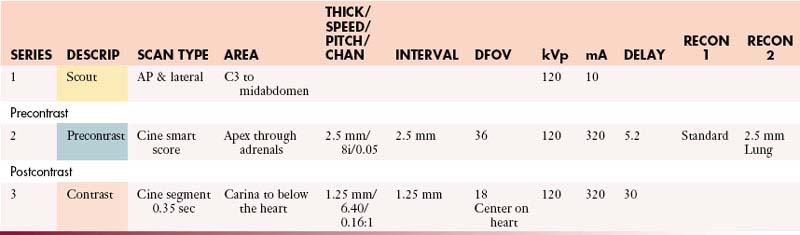
Cardiac Tumor (Gated Study)
IV Contrast: Iso-osmolar & saline
| VISIPAQUE (mL/sec) | SALINE (mL/sec) | SCAN DELAY (sec) |
|---|---|---|
| 5 | 5 | 30 |
Coronal: 0.8 mm @ 2.5 mm or default—standard algorithm
Sagittal: 0.8 mm @ 2.5 mm or default—lung algorithm
Scanning direction from superior to inferior.
Check heart rate on arrival. Call radiologist for heart rate > 70 bpm.
Select postcontrast pitch and FOV based on heart rate and patient size.
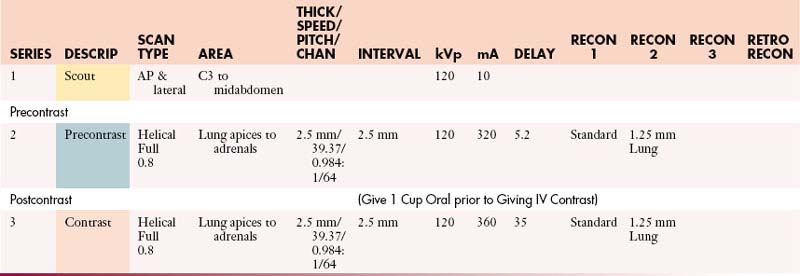
Chest with Contrast
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 3 | 30 |
| 2.5 | 35 |
| 2 | 40 |
Coronal: 2.5 mm @ 0.8 mm or default—standard algorithm
Chest without Contrast
Coronal: 2.5 mm @ 0.8 mm or default—standard algorithm
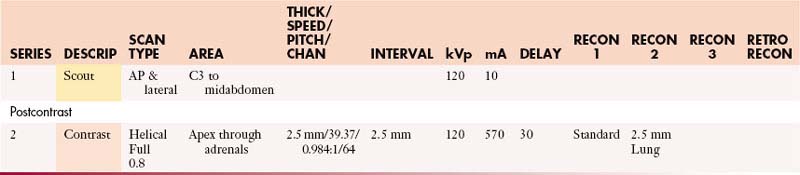
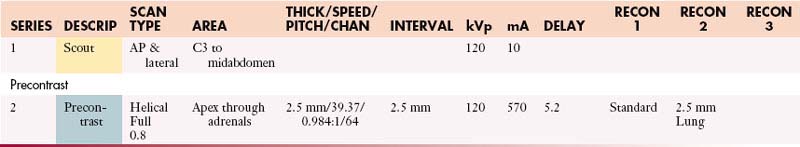
Coronary Artery Screening (Gated Study)
IV Contrast: Iso-osmolar & saline
| ISO-OSMOLAR (mL/sec) | SALINE (mL/sec) | SCAN DELAY (sec) |
|---|---|---|
| 5 | 5 | 30 |
Coronal 0.8 mm @ 2.5 mm or default—standard algorithm
Sagittal 0.8 mm @ 2.5 mm or default—lung algorithm
Scanning direction from superior to inferior.
Check heart rate on arrival. Call radiologist for heart rate > 70 bpm.
Select postcontrast pitch and FOV based on heart rate and patient size.
Esophageal Leak Protocol
16 oz 2% barium sulfate or Gastroview for postcontrast chest
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 3 | 35 |
Coronal: 1.25 mm @ 0.8 mm or default—standard algorithm
Sagittal: 1.25 mm @ 0.8 mm or default—lung algorithm
Low-Dose Surveillance Chest with Contrast (Nodule or Lung Cancer)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 3 | 30 |
| 2.5 | 35 |
| 2 | 40 |
Perfusion Chest without and with Contrast
Scanning direction from superior to inferior.
Schedule patient in rose & green zones ONLY and before 5:00 PM.
PE Protocol
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 4.2 | 20 |
Coronal: 1.25 mm @ 0.8 mm or default—standard algorithm
Sagittal: 1.25 mm @ 0.8 mm or default—lung algorithm
Superior Vena Cava Venogram
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 3 | 35 |
Coronal: 0.8 mm @ 2.5 mm or default—standard algorithm
Sagittal: 0.8 mm @ 2.5 mm or default—lung algorithm
Coronal: 0.8 mm @ 2.5 mm or default—standard algorithm
Sagittal: 0.8 mm @ 2.5 mm or default—lung algorithm
Scanning direction from superior to inferior.
Bilateral arm injection will be determined by the radiologist.
Chest with Contrast (Virtual Bronchoscopy)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 3 | 30 |
| 2.5 | 35 |
| 2 | 40 |
Coronal: 2.5 mm @ 0.8 mm or default—standard algorithm
Abdomen/Pelvis Protocols (MDCT 64 Slice)
Abdomen and Pelvis with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
Abdomen and Pelvis without Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
Abdomen and Pelvis without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
AdrenalsAbdomen with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 5 | 60 |
AdrenalsAbdomen without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 5 | 60 |
AdrenalsAbdomen and Pelvis with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 5 | 60 |
AdrenalsAbdomen and Pelvis without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 5 | 60 |
AdrenalsChest and Abdomen with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 5 | 60 |
AdrenalsChest and Abdomen without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 5 | 60 |
AdrenalsChest, Abdomen, and Pelvis with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 5 | 60 |
AdrenalsChest, Abdomen, and Pelvis without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 5 | 60 |
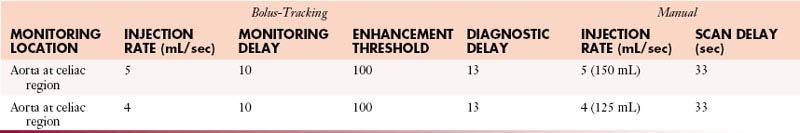
Appendiceal/PeritonealAbdomen and Pelvis without and with Contrast
GI Contrast: Gastroview 15 mL/400 mL (oral & rectal)
IV Contrast: 350 mgI/mL or iso-osmolar 320 mgI/mL
Volume: 150 mL contrast @ 4 mL/sec followed by 100 mL normal saline @ 3 mL/sec
Scanning direction from superior to inferior.
Do coronal and sagittal re-format on all phases of the postcontrast images.
Appendiceal/PeritonealChest, Abdomen, and Pelvis without and with Contrast
GI Contrast: Gastroview 15 mL/400 mL (oral & rectal)
IV Contrast: 350 mgI/mL or iso-osmolar 320 mgI/mL
Volume: 150 mL contrast @ 4 mL/sec followed by 100 mL normal saline @ 3 mL/sec
Scanning direction from superior to inferior.
Do coronal and sagittal re-format on all phases of the postcontrast images.
Bowel CarcinoidAbdomen and Pelvis without and with Contrast
1st Dose: 1 bottle (450 mL) 60 min prior to scan
2nd Dose: 1 bottle (450 mL) 40 min prior to scan Rectal Contrast: Water
3rd Dose: ½ bottle (225 mL) 20 min prior to scan
4th Dose: ½ bottle (225 mL) on table
Chest and Abdomen without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral)
Chest, Abdomen, and Pelvis with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
Chest, Abdomen, and Pelvis without Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
Chest, Abdomen, and Pelvis without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
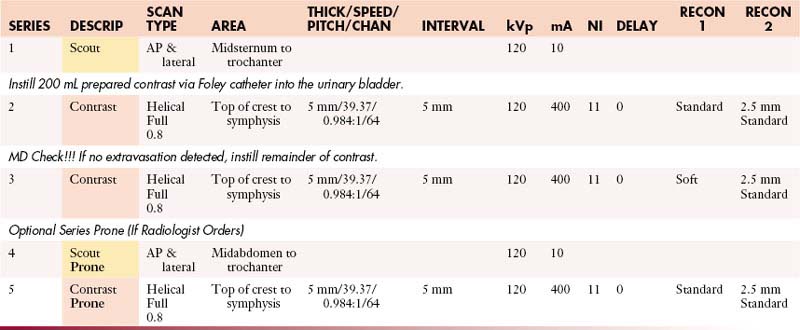
CT Cystogram
Instructions: Prepare contrast by injecting 75 mL of Optiray 320 into a 500-mL bag of normal saline.
KUB for Barium
Scanning direction from superior to inferior.
MD check to see if patient can continue with the preparation.
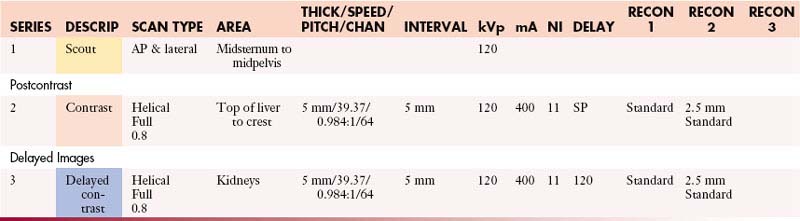
LiverAbdomen without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral)
LiverAbdomen and Pelvis without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
LiverChest and Abdomen without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral)
LiverChest, Abdomen, and Pelvis without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
Lymphoma with Contrast:(Body—H/N Studies)
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
Lymphoma without Contrast(Body—H/N Studies)
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
Lymphoma without and with Contrast(Body—H/N Studies)
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
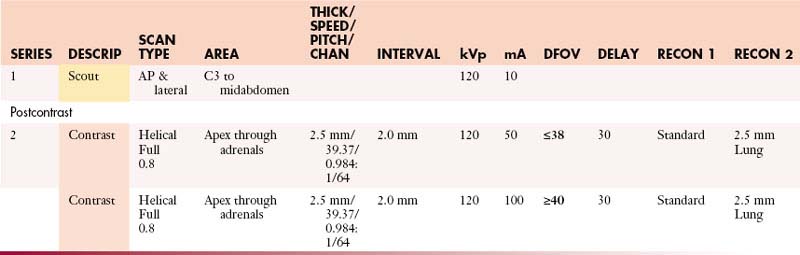
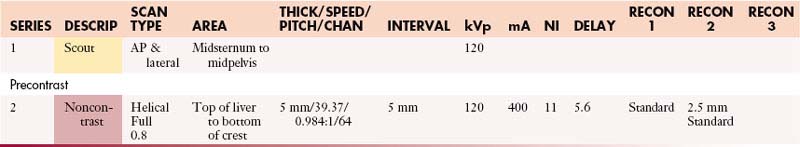
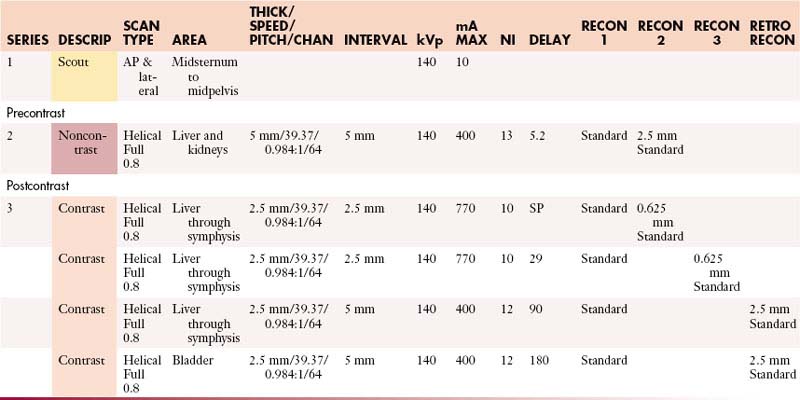
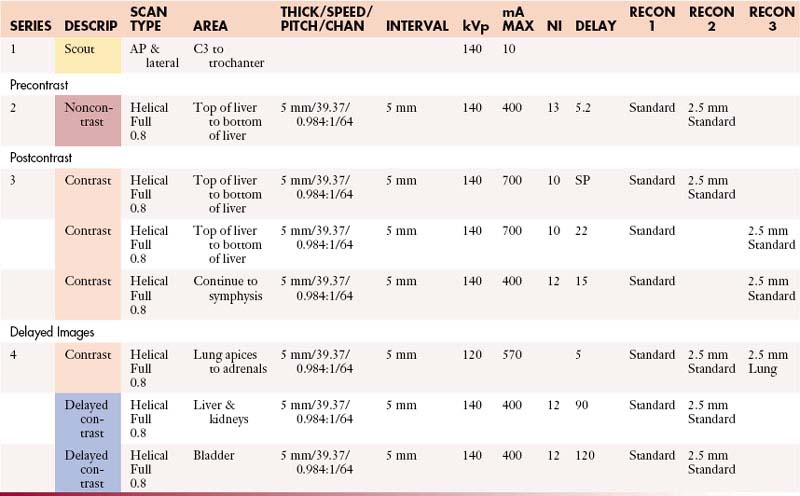
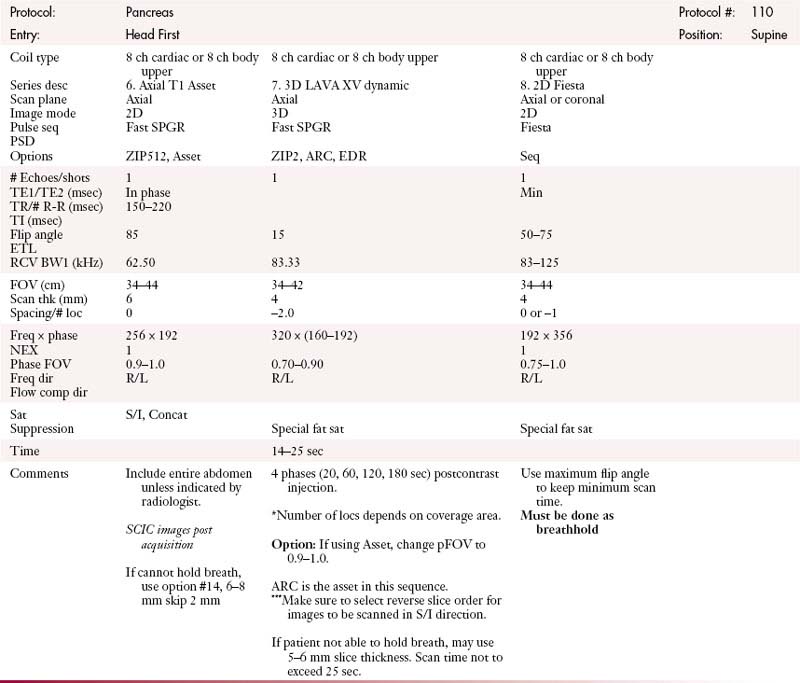
PancreasAbdomen without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
PancreasAbdomen and Pelvis without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
PancreasChest, Abdomen, and Pelvis without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
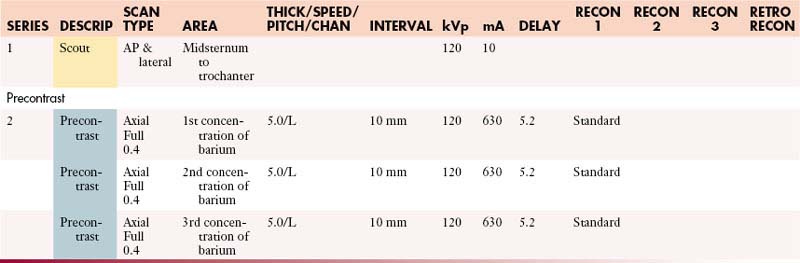
Pancreatic Islet CellAbdomen without and with Contrast
1st Dose: 1 bottle (450 mL) 60 min prior to scan
2nd Dose: 1 bottle (450 mL) 40 min prior to scan
3rd Dose: ½ bottle (225 mL) 20 min prior to scan
4th Dose: ½ bottle (225 mL) on table
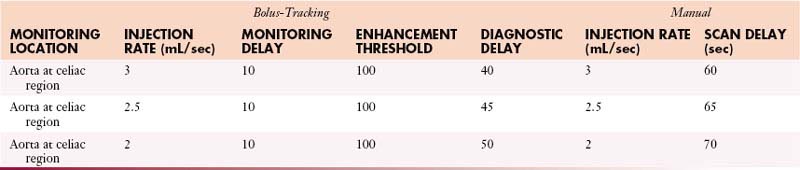
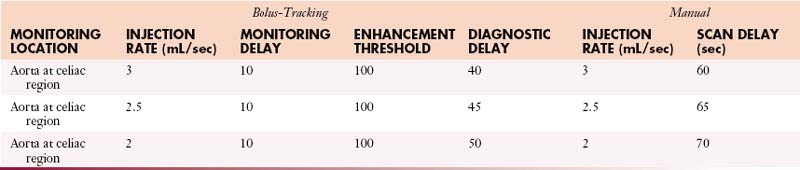
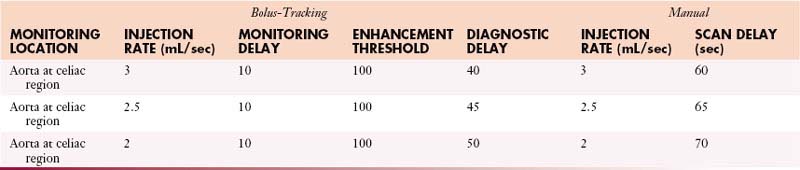
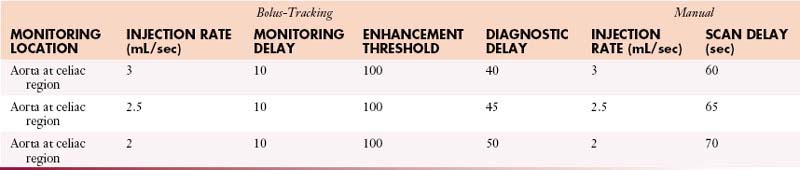
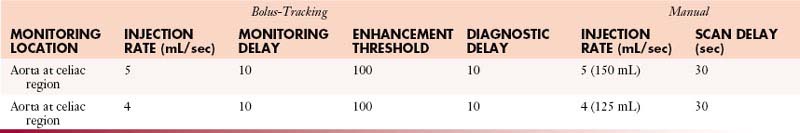
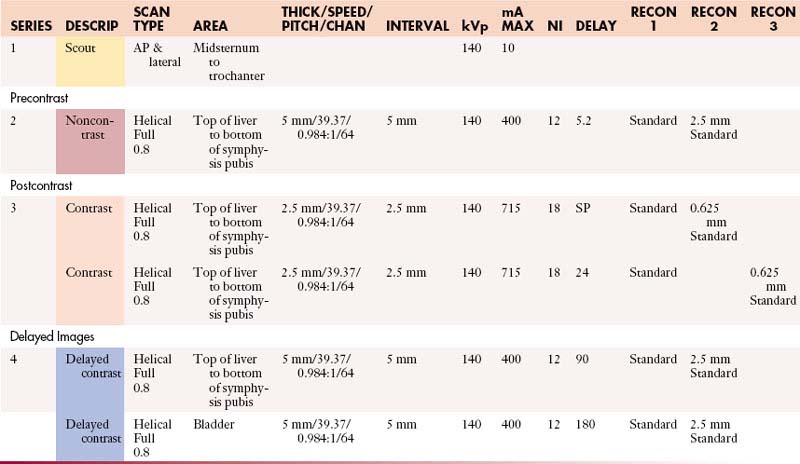
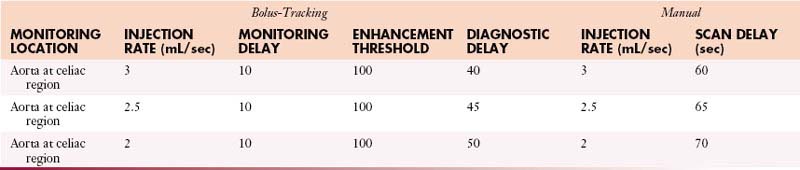
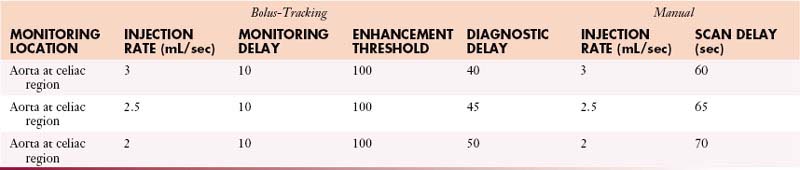
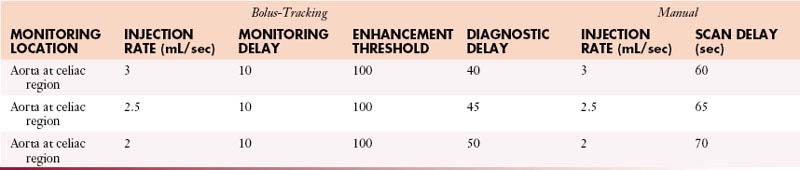
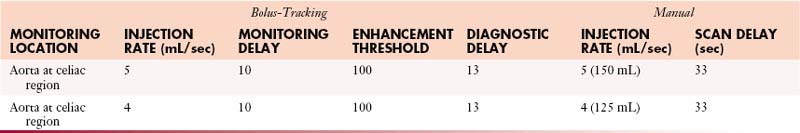
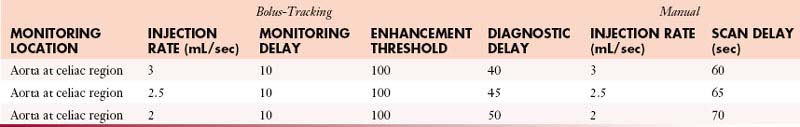
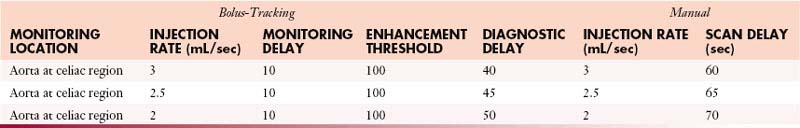
Post Cystectomy (Formerly “Bladder”)Abdomen and Pelvis with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 3 | 60 |
| 2.5 | 65 |
| 2 | 70 |
Post Cystectomy (Formerly “Bladder”)Chest, Abdomen, and Pelvis with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 3 | 60 |
| 2.5 | 65 |
| 2 | 70 |
Post Cystectomy (Formerly “Bladder”)Chest, Abdomen, and Pelvis without and with Contrast
GI Contrast: 2% barium sulfate or Gastrografin or water (oral & rectal)
| Manual | |
|---|---|
| INJECTION RATE (mL/sec) | SCAN DELAY (sec) |
| 3 | 60 |
| 2.5 | 65 |
| 2 | 70 |
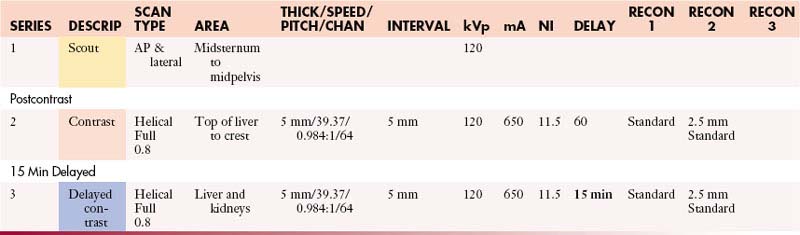
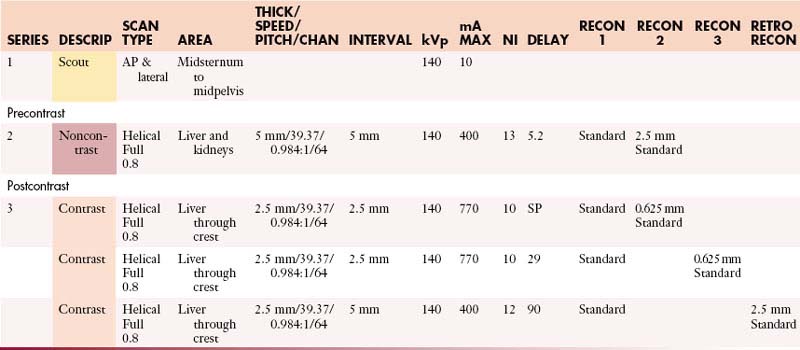
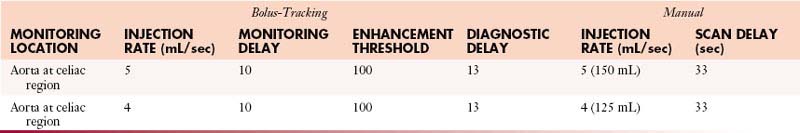
RenalAbdomen with Contrast
1st Dose: 1 bottle (450 mL) 90 min prior to scan
2nd Dose: 1 bottle (450 mL) 60 min prior to scan
3rd Dose: ½ bottle (225 mL) on table
IV Preparation: 250 mL normal saline 15–40 min prior to scan
IV Contrast: 320 mgI/mL or iso-osmolar 320 mgI/mL
1st Injection: 100 mL contrast @ 5 mL/sec followed by 30 mL normal saline @ 5 mL/sec
2nd Injection: 50 mL contrast @ 3 mL/sec followed by 30 mL normal saline @ 3 mL/sec
RenalChest and Abdomen without and with Contrast
1st Dose: 1 bottle (450 mL) 90 min prior to scan
2nd Dose: 1 bottle (450 mL) 60 min prior to scan
3rd Dose: ½ bottle (225 mL) on table
IV Preparation: 250 mL normal saline 15–40 min prior to scan
IV Contrast: 320 mgI/mL or iso-osmolar 320 mgI/mL
1st Injection: 100 mL contrast @ 5 mL/sec followed by 30 mL normal saline @ 5 mL/sec
2nd Injection: 50 mL contrast @ 3 mL/sec followed by 30 mL normal saline @ 3 mL/sec
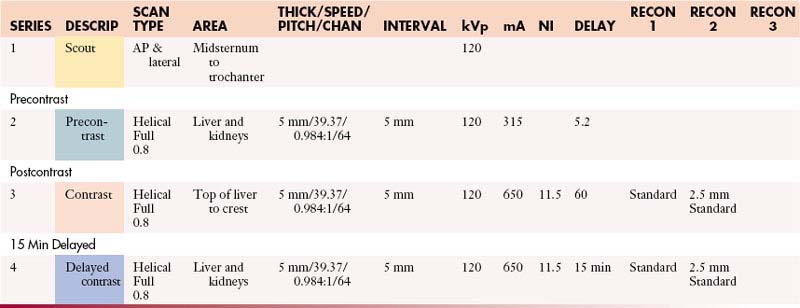
RenalChest, Abdomen, and Pelvis without and with Contrast
1st Dose: 1 bottle (450 mL) 90 min prior to scan
2nd Dose: 1 bottle (450 mL) 60 min prior to scan
3rd Dose: ½ bottle (225 mL) on table Rectal Contrast: None
IV Preparation: 250 mL normal saline 15–40 min prior to scan
IV Contrast: 320 mgI/mL or iso-osmolar 320 mgI/mL
1st Injection: 100 mL contrast @ 5 mL/sec followed by 30 mL normal saline @ 5 mL/sec
2nd Injection: 50 mL contrast @ 3 mL/sec followed by 3 mL normal saline @ 3 mL/sec
Renal + 3DAbdomen without and with Contrast
1st Dose: 1 bottle (450 mL) 90 min prior to scan
2nd Dose: 1 bottle (450 mL) 60 min prior to scan
3rd Dose: ½ bottle (225 mL) on table
IV Preparation: 250 mL normal saline 15–40 min prior to scan
IV Contrast: 320 mgI/mL or iso-osmolar 320 mgI/mL
1st Injection: 100 mL contrast @ 5 mL/sec followed by 30 mL normal saline @ 5 mL/sec
2nd Injection: 50 mL contrast @ 3 mL/sec followed by 30 mL normal saline @ 3 mL/sec
Renal + 3DAbdomen and Pelvis without and with Contrast
1st Dose: 1 bottle (450 mL) 90 min prior to scan
2nd Dose: 1 bottle (450 mL) 60 min prior to scan Rectal Contrast: None
3rd Dose: ½ bottle (225 mL) on table
IV Preparation: 250 mL normal saline 15–40 min prior to scan
IV Contrast: 320 mgI/mL or iso-osmolar 320 mgI/mL
1st Injection: 100 mL contrast @ 5 mL/sec followed by 30 mL normal saline @ 5 mL/sec
2nd Injection: 50 mL contrast @ 3 mL/sec followed by 30 mL normal saline @ 3 mL/sec
Renal + 3DChest and Abdomen without and with Contrast
1st Dose: 1 bottle (450 mL) 90 min prior to scan
2nd Dose: 1 bottle (450 mL) 60 min prior to scan
3rd Dose: ½ bottle (225 mL) on table
IV Preparation: 250 mL normal saline 15–40 min prior to scan
IV Contrast: 320 mgI/mL or iso-osmolar 320 mgI/mL
1st Injection: 100 mL contrast @ 5 mL/sec followed by 30 mL normal saline @ 5 mL/sec
2nd Injection: 50 mL contrast @ 3 mL/sec followed by 30 mL normal saline @ 3 mL/sec
Renal + 3DChest, Abdomen, and Pelvis without and with Contrast
1st Dose: 1 bottle (450 mL) 90 min prior to scan
2nd Dose: 1 bottle (450 mL) 60 min prior to scan
3rd Dose: ½ bottle (225 mL) on table Rectal Contrast: None
IV Preparation: 250 mL normal saline 15–40 min prior to scan
IV Contrast: 320 mgI/mL or iso-osmolar 320 mgI/mL
1st Injection: 100 mL contrast @ 5 mL/sec followed by 30 mL normal saline @ 5 mL/sec
2nd Injection: 50 mL contrast @ 3 mL/sec followed by 30 mL normal saline @ 3 mL/sec
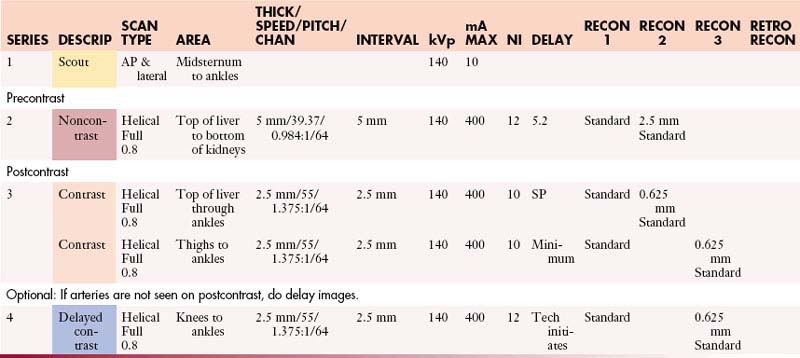
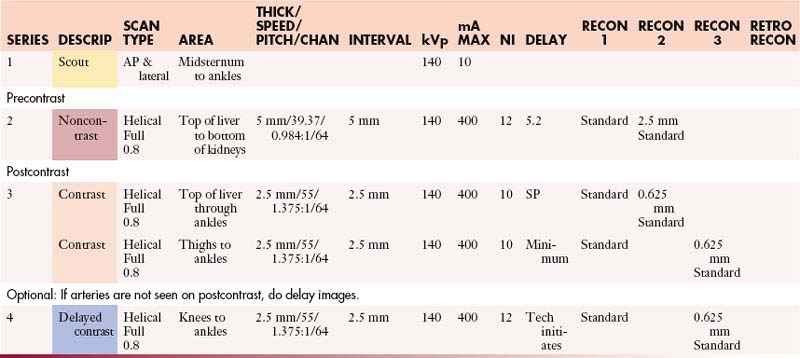
CT Runoff
Re-format: Sagittal and coronal—postcontrast.
CT Runoff (Fast)
Re-format: Sagittal and coronal—postcontrast.
Scanning direction from superior to inferior.
Have patient hold breath then gently release breath to avoid motion in pelvis through ankle regions.
Enterography (Small Bowel)Abdomen and Pelvis with Contrast
IV Contrast: 320 mgI/mL @ 4 mL/sec followed by 50 mL saline flush @ 4 mL/sec
Enterography (Small Bowel)Abdomen and Pelvis without and with Contrast
IV Contrast: 320 mgI/mL @ 4 mL/sec followed by 50 mL saline flush @ 4 mL/sec
Enterography (Small Bowel)Chest, Abdomen, and Pelvis with Contrast
IV Contrast: 320 mgI/mL @ 4 mL/sec followed by 50 mL saline flush @ 4 mL/sec
Enterography (Small Bowel)Chest, Abdomen, and Pelvis without and with Contrast
IV Contrast: 320 mgI/mL @ 4 mL/sec followed by 50 mL saline flush @ 4 mL/sec
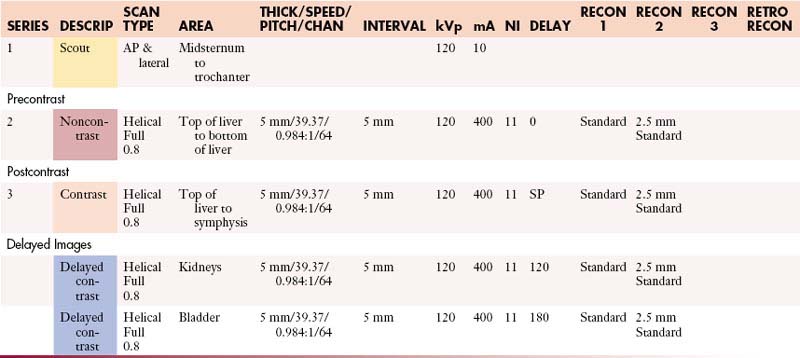
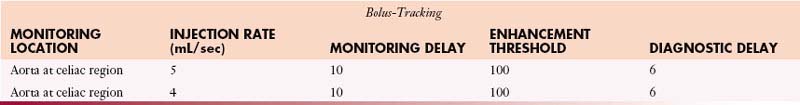
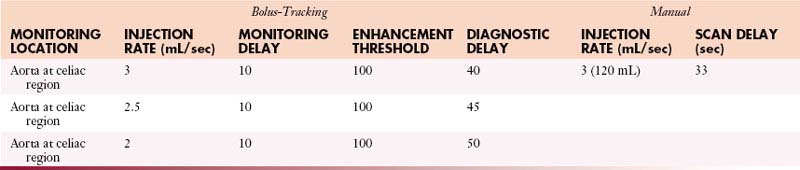
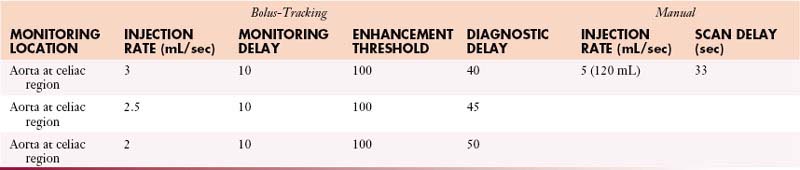
UrogramAbdomen and Pelvis without and with Contrast
1st Dose: 1 bottle (450 mL) 90 min prior to scan
2nd Dose: ½ bottle (225 mL) on table Rectal Contrast: None
IV Preparation: 250 mL normal saline 15–40 min prior to scan
Medication: 10 mL Lasix IV to be given after precontrast
IV Contrast: 320 mgI/mL or iso-osmolar 320 mgI/mL
1st Injection: 120 mL contrast @ 3 mL/sec followed by 150 mL normal saline @ 3 mL/sec
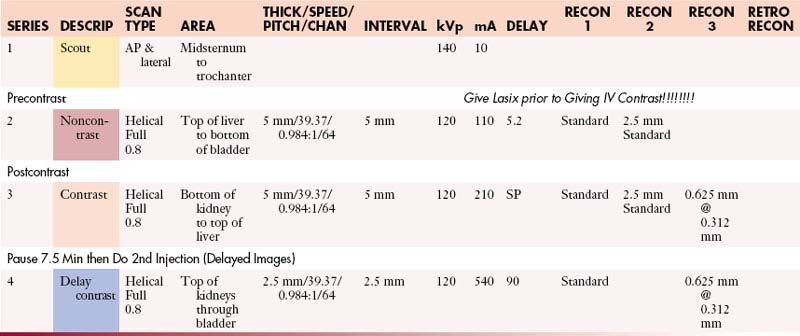
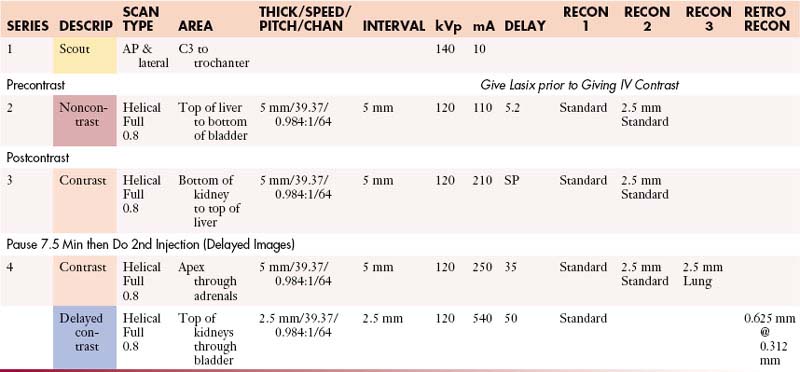
UrogramChest, Abdomen, and Pelvis without and with Contrast
1st Dose: 1 bottle (450 mL) 90 min prior to scan
2nd Dose: ½ bottle (225 mL) on table
IV Preparation: 250 mL normal saline 15–40 min prior to scan Rectal Contrast: None
IV Contrast: 320 mgI/mL or iso-osmolar 320 mgI/mL
1st Injection: 120 mL contrast @ 3 mL/sec followed by 150 mL normal saline @ 5 mL/sec
Musculoskeletal (MSK) Protocols (MDCT 64 Slice)
MSK (Bridging Protocol) with Contrast
Sagittal and coronal re-formatting is to be done at each bridging site using a small FOV.
The third re-format will include the entire length of the bone.
MSK (Bridging Protocol) without Contrast
Sagittal and coronal re-formatting is to be done at each bridging site using a small FOV.
The third re-format will include the entire length of the bone.
MSK Operating Room Hi-Res Protocol (64 Slice)
| Oral Contrast | N/A |
| Precontrast | N/A |
| IV Contrast | As indicated by radiologist |
| Volume | 125 mL |
| Injection Rate | 3 mL/sec |
| Scan Delay | 90 sec |
| Scan Mode | Helical |
| Scan Algorithm | Standard and bone |
| Scan Direction | Superior to inferior |
| Recon Algorithm | Standard and bone (0.625 mm @ 0.31 mm) |
| Reconstruction
Retro Recon |
Recon 2: 2.5 mm thickness @ 2.5 mm interval standard algorithm Recon 3: 2.5 mm thickness @ 2.5 mm interval bone algorithm Retro: 0.625 mm thickness @ 0.625 mm interval standard algorithm Retro: 1.25 mm thickness @ 0.625 mm interval standard algorithm Retro: 1.25 mm thickness @ 1.25 mm interval standard algorithm |
Sagittal and coronal re-formats for every musculoskeletal patient
1.25 mm @ 1.25 mm standard and bone algorithms
All patients with metal implants—140 kVp and 360 mA/0.5 sec.
Operating Room Hi-Res Protocol with Contrast
Scanning direction from superior to inferior.
Operating Room Hi-Res Protocol without Contrast
Scanning direction from superior to inferior.
Operating Room Standard Protocol (64 Slice)
| Oral Contrast | N/A |
| Precontrast | N/A |
| IV Contrast | As indicated by radiologist |
| Volume | 125 mL |
| Injection Rate | 3 mL/sec |
| Scan Delay | 90 sec |
| Scan Mode | Helical |
| Scan Algorithm | Standard and bone |
| Scan Direction | Superior to inferior |
| Recon Algorithm | Standard and bone (0.625 mm @ 0.31 mm) |
| Reconstruction
Retro Recon |
Recon 2: 2.5 mm thickness at 2.5 mm interval standard algorithm Recon 3: 2.5 mm thickness at 2.5 mm interval bone algorithm Retro: 0.625 mm thickness at 0.625 mm interval standard algorithm Retro: 1.25 mm thickness at 0.625 mm interval standard algorithm Retro: 1.25 mm thickness at 1.25 mm interval standard algorithm |
Sagittal and coronal re-formats for every musculoskeletal patient.
1.25 mm @ 1.25 mm standard and bone algorithms.
All patients with metal implants—140 kVp and 360 mA/0.5 sec.
Operating Room Standard Protocol with Contrast
Scanning direction from superior to inferior.
Operating Room Standard Protocol without Contrast
Scanning direction from superior to inferior.
1. Einhorn L.H., Burgess M.A., Gottlieb J.A. Metastatic patterns of choroidal melanoma. Cancer. 1974;34:1001-1004.
2. Zakka K.A., Foos R.Y., Omphroy C.A., et al. Malignant melanoma: analysis of an autopsy population. Ophthalmology. 1980;87:549-556.
3. Rajpal S., Moore R., Karakousis C.P. Survival in metastatic ocular melanoma. Cancer. 1983;52:334-336.
4. Bedikian A.Y., Legha S.S., Mavligit G., et al. Treatment of uveal melanoma metastatic to the liver. Cancer. 1995;76:1665-1670.
5. Collaborative Ocular Melanoma Study Group. Assessment of metastatic disease status at death in 435 patients with large choroidal melanoma in the Collaborative Ocular Melanoma Study (COMS). COMS Report No. 15. Arch Ophthalmol. 2001;119:670-676.
6. Silverman P.M. Liver metastases: optimizing detection with multislice CT (MSCT). Cancer Imaging. 2004;4(Spec. No. B):S108-S113. Epub 2005;January 3
7. Silverman P.M., Roberts S., Tefft M.C., et al. Helical CT of the liver: clinical application of an automated computer technique, SmartPrep, for obtaining images with optimal contrast enhancement. AJR Am J Roentgenol. 1995;165:73-78.
8. Silverman P. Multislice (MSCT) Computed Tomography: A Practical Approach to Clinical Protocols. Philadelphia: Lippincott Williams & Wilkins; 2002.