Prone Positioning
A There is currently only one indication for prone positioning: Acute respiratory distress syndrome (ARDS).
B The specific level of oxygenation deficit indicating a need for prone positioning has not been precisely defined.
C However, many would agree that if the following is required and the Pao2 is still <70 mm Hg, prone positioning should be considered.
D Animal studies indicate that prone positioning is lung protective (i.e., ventilator-induced lung injuries are less severe in the prone position than in the supine position).
II Contraindications of Prone Positioning
B Recent thoracic or abdominal surgery
F However, correcting hemodynamic and airway instability eliminates the contraindication.
A In the supine position, especially in ARDS because of the increased weight of the lung, there is a large transpulmonary pressure gradient between nondependent and dependent lung.
B The reasons for this gradient when supine are the following.
1. Approximately 60% of the lung is in the dependent position. This is because the lung in the supine position is essentially triangular shaped with the base of the triangular most dependent.
2. The heart and great vessels sit on top of the lungs.
3. The posterior basilar segments of the lungs are under the diaphragm.
C In ARDS the force exerted by these factors pulls the lung from the anterior chest wall, creating a negative anterior transpulmonary pressure gradient and a positive posterior or dependent transpulmonary pressure gradient.
D This causes most of the functional residual capacity (FRC) to occupy the nondependent lung and most of the tidal volume (Vt) to go to the nondependent lung.
E A large V/Q mismatch is created because most perfusion in the supine position goes to the dependent lung.
F On positioning in the prone position many of these issues are reversed.
1. The majority of the lung is now nondependent.
2. The heart and great vessels are now dependent.
3. The impact of the abdomen on the posterior-basilar lung segments is eliminated.
4. Prone positioning also decreases chest wall compliance.
5. As a result, the transpulmonary pressure gradient is more evenly distributed from nondependent to dependent lung.
6. Blood flow also is more evenly distributed from nondependent to dependent lung.
7. In the prone position a greater percentage of the FRC volume is dependent and Vt is more evenly distributed.
8. All of this results in improved V/Q matching and Pao2 increases.
IV Response to Prone Positioning
A Numerous care series indicate that approximately 70% of ARDS patients when placed in the prone position experience a >20% increase in Pao2 at the same ventilator settings.
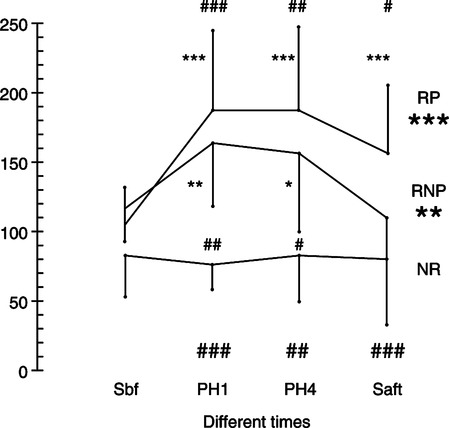
B Figure 45-1 depicts the possible responses of patients turned prone. Unfortunately no good explanation is available as to why some respond to prone positioning and others do not.
1. No response in approximately 20% to 30% of patients (nonresponders)
2. An increase in Pao2 that is sustained when returned supine occurs in approximately 30% to 40% of patients (persistent responders).
3. An increase in Pao2 when prone but a loss of the Pao2 benefit when returned to the supine position occurs in approximately 30% to 40% of patients (nonpersistent responders).
C Some patients mobilize a large amount of secretions when turned prone. This may account for the sustained increase in Pao2.
D In some patients the areas of atelectasis/consolidation seem to change when moved supine to prone to supine. Thus when turned supine the benefit of prone positioning is lost.
V The Process of Turning Prone
A At least four staff members are necessary to turn a patient prone.
1. One therapist to only pay attention to the airway
B Before turning care should be taken to ensure
1. The endotracheal tube is properly placed and secured.
2. Vascular lines are properly placed and secured.
C The therapist maintaining the airway and the nurse maintaining the vascular lines should also carefully observe the response of the patient during prone placement: cardiac monitor, pulse oximeter, and function of the mechanical ventilator.
D As the patient is turned the therapist at the airway should be ready to immediately suction the patient’s airways.
1. In some patients a large amount of secretion is mobilized as soon as the patient is prone.
2. There are cases in which the volume is so large that the patient cannot be ventilated until the secretions are removed.
E After stabilization in the prone position, ventilator settings may need to be adjusted.
2. PEEP decreased but only after decreasing FIO2
3. Because of the lower chest wall compliance in the prone position, Vt or ventilating pressure may need to be adjusted.
F Two specific positions during prone placement have been advocated.
1. Figure 45-2 depicts complete prone positioning.
a. In this position the head, chest, and hip need to be properly supported to prevent trauma and allow free movement of the abdomen.
b. Free abdominal movement is especially critical if the patient is obese.
2. The second position is the swimmer’s position, which is the more commonly used prone position.
a. The patient’s head is turned to one side.
b. The arm on that side is placed in front of the patient’s face.
c. The leg on the same side is bent at the knee and hip.
d. The arm on the opposite side is left along the body and that leg is straight.
e. A pillow is placed under the shoulder, chest, and hip on the side the patient is facing.
A All mammals sleep in the prone position.
B When placed supine and sedated, dependent atelectasis develops in all laboratory animals.
C After approximately 2 hours supine and sedated, these animals’ Pao2 decreases markedly.
D Patients undergoing surgery in the supine position rapidly develop atelectasis and require higher FIO2.
E As a result patients needing prone positioning should be kept prone indefinitely.
F From a practical perspective patients should be kept prone >20 hours per day if the oxygenation and lung protective effects of prone positioning are to be maximized.
G Patients only need to be placed supine for nursing care, ideally only once per day for as short a time as possible.
H The greater the percentage of the day patients are prone, the greater the benefit from prone positioning.
VII When to Move Patient from Prone Position
A Patients should be moved from prone position before attempts to wean begin.
B Most patients can be moved from prone position when a Pao2 >60 mm Hg can be sustained by an FIO2 ≤0.40 and a PEEP ≤8 cm H2O.
VIII Complications of Prone Positioning (Box 45-2)
A The most devastating complication of prone positioning is the loss of an artificial airway. This should be extremely infrequent if the aforementioned proper precautions are taken.
B Loss of vascular lines or urinary catheters; this can be avoided with proper care during positioning.
C From the perspective of the family, facial edema is a major concern.
1. Family should be notified that disfiguring facial edema is common.
2. Fortunately the edema resolves as quickly as it forms when patients are again placed supine.
D Development of transient cardiac arrhythmias or hyper/hypotension; it normally can be rapidly corrected with fluid or drug therapy.