Chapter 12 Prolapse and Urogynaecology
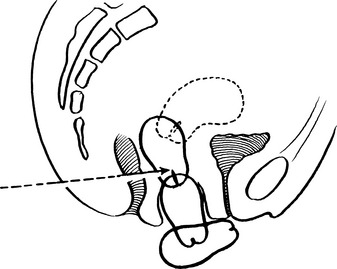
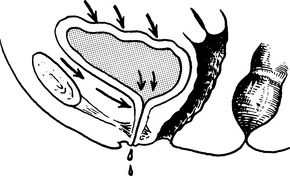
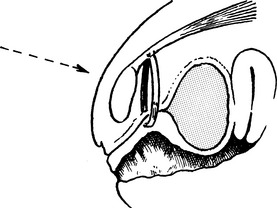
Retroversion of the uterus
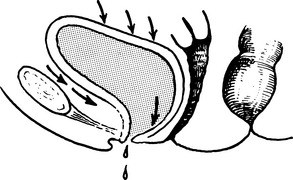
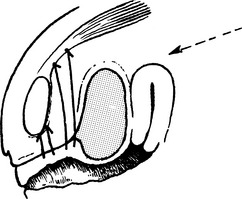
Anteverted Uterus
The uterus is approximately at right angles to the vagina and has a slight forward curve.
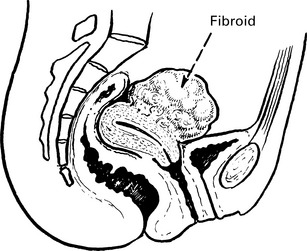
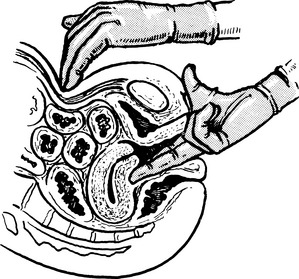
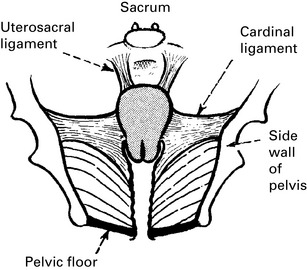
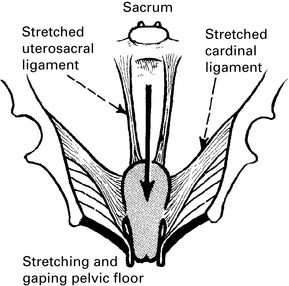
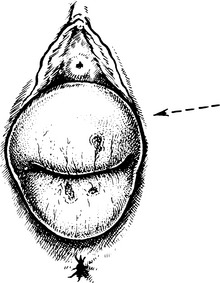
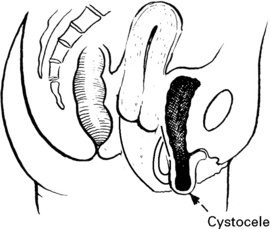
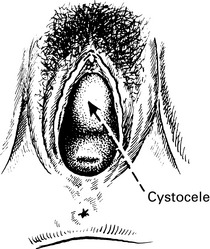
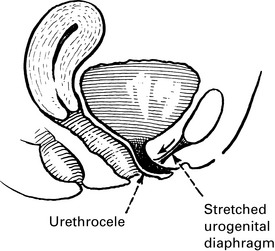
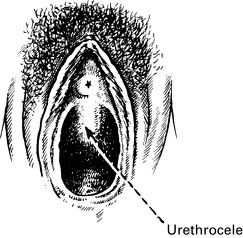
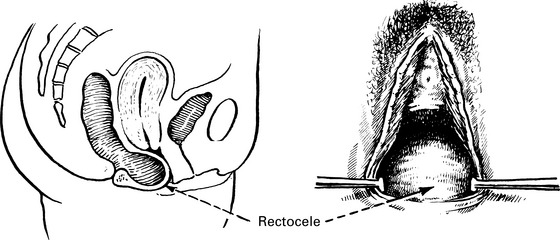
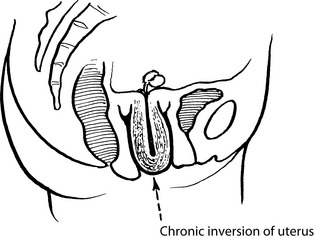
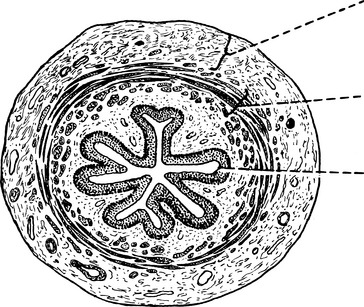
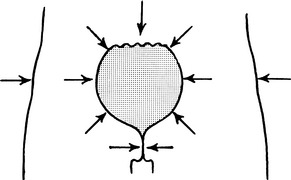
Uterovaginal prolapse
Herniation of the genital tract through the pelvic diaphragm.
The causes of prolapse are the following:
Uterovaginal prolapse
First degree: cervix still inside vagina.
Second degree: the cervix appears at the level of the introitus.
Clinical features of prolapse
Pessary treatment
Indications for pessary treatment
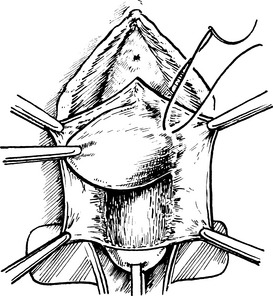
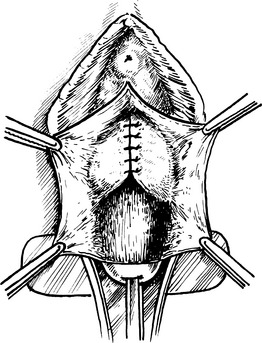
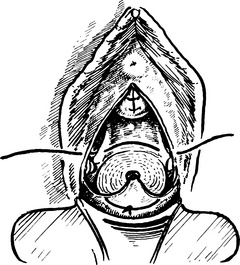
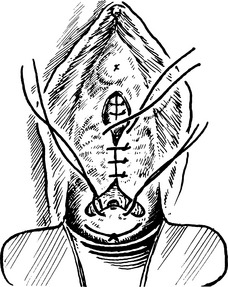
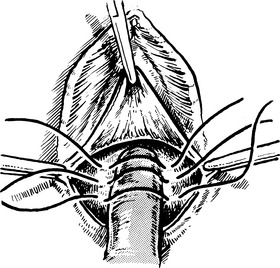
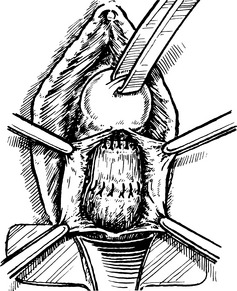
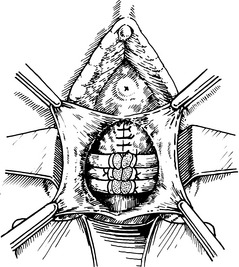
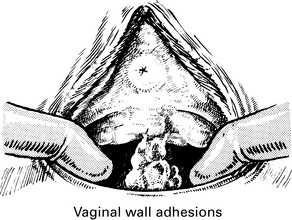
Manchester repair
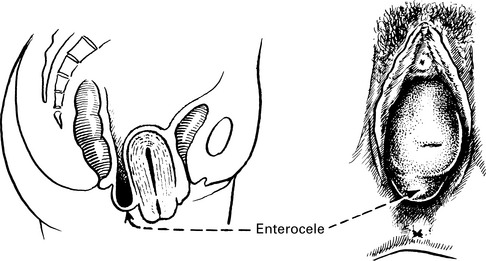
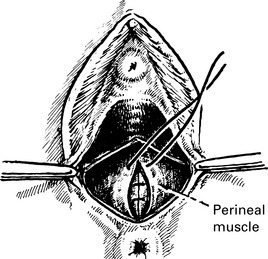
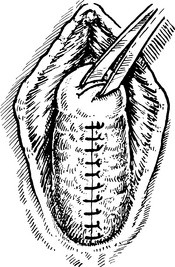
Repair of enterocele
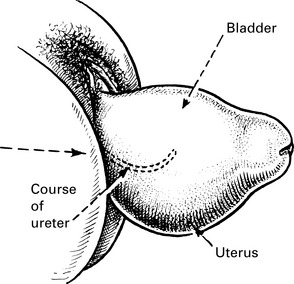
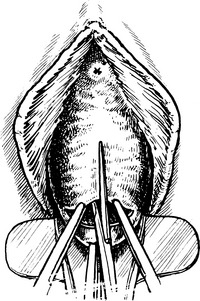
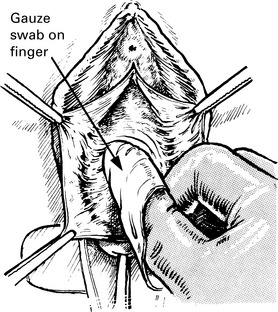
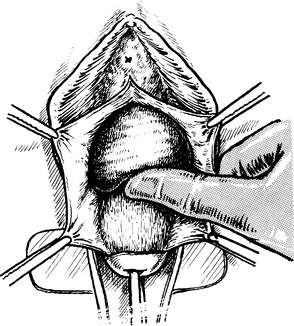
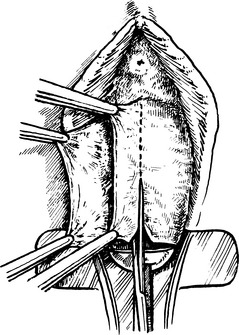
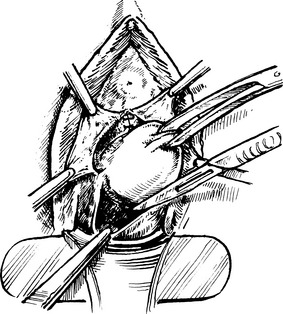
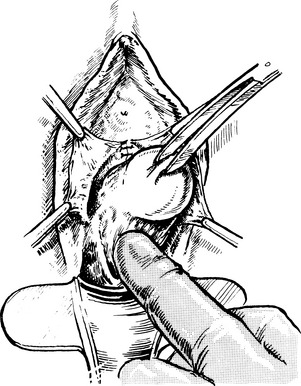
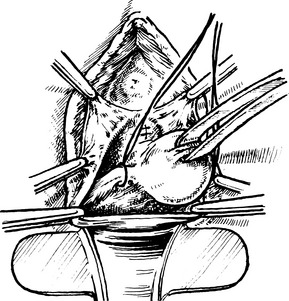
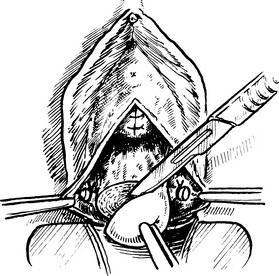
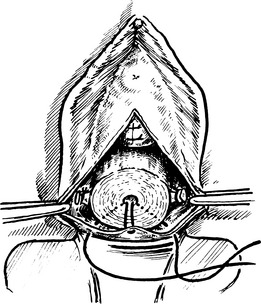
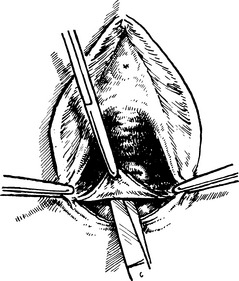
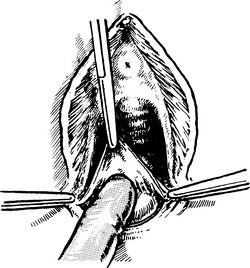
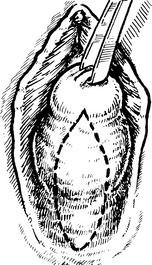
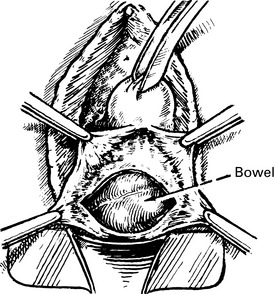
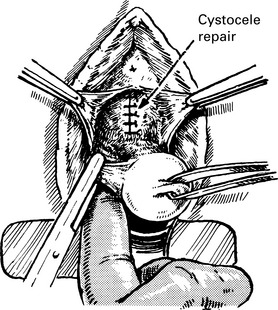
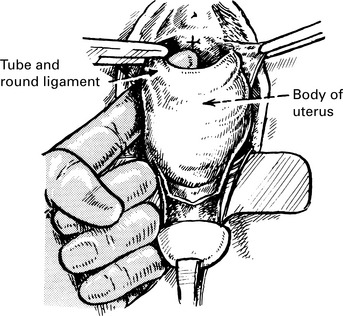
Vaginal hysterectomy
Indications
Operative and postoperative complications
Selection of Patients
Perioperatively
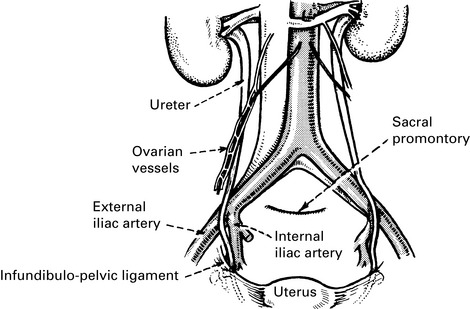
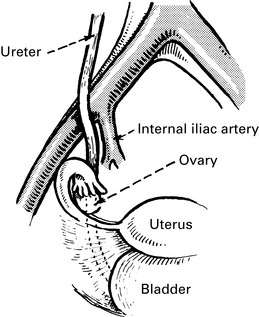
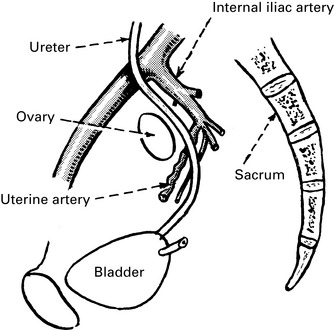
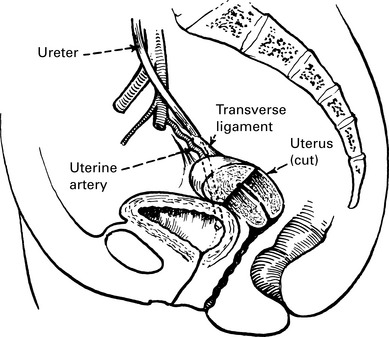
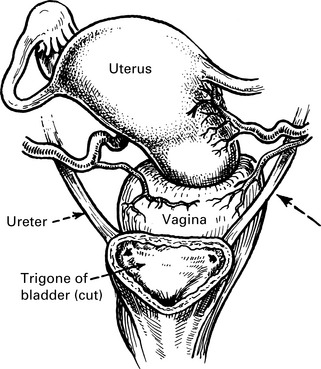
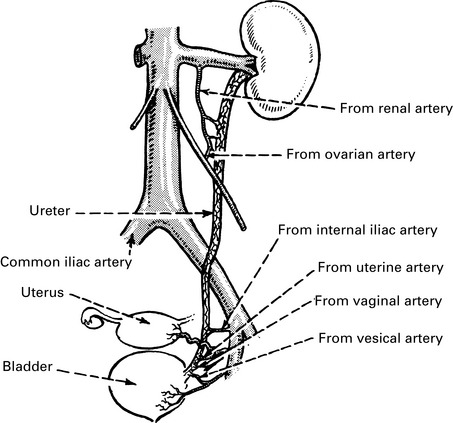
Blood supply of the ureter
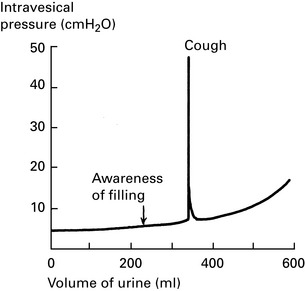
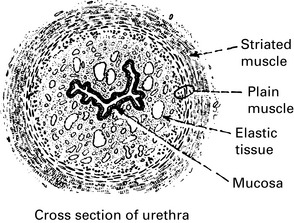
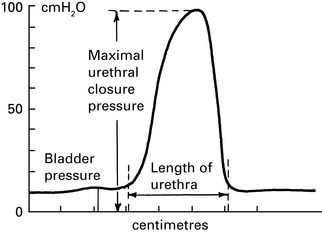
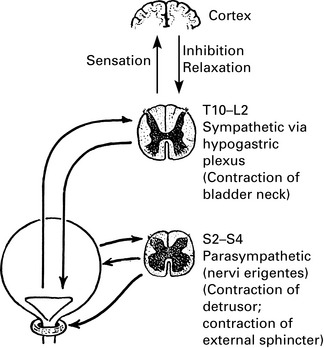
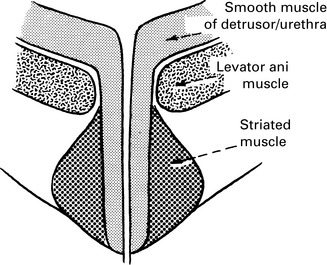
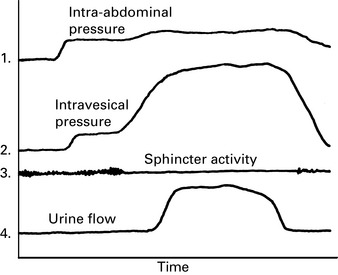
Physiology of micturition
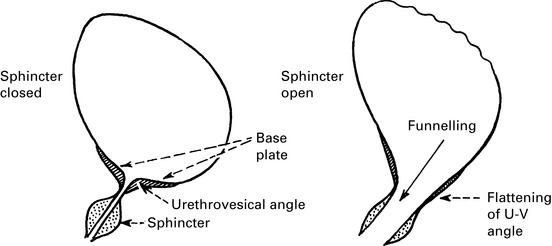
Genuine stress incontinence
Other incontinence mechanisms
Fistula incontinence is described in Chapter 14 Complications of Gynaecological Surgery.
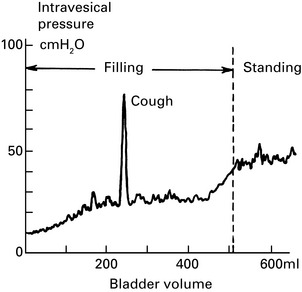
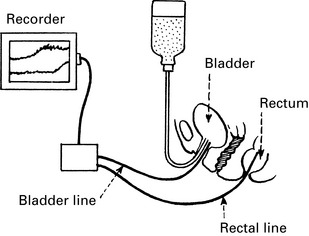
Investigation of incontinence
Incontinence may be due to the following:
Usually occurs after one or more pregnancies.
Urine appears only after effort (stress) such as coughing, laughing or running for a bus.
Usually only small quantities of urine are passed, whether the bladder is full or not.
Complaints of urge incontinence and frequency, especially at night (nocturia).
May pass large volumes of urine when bladder muscle contracts.
The social effects of urinary incontinence should be considered when planning treatment.
Examination
Signs of infection (urethritis) and scarring from previous surgery are looked for, and the usual bimanual and speculum examinations are performed (Chp. 5).
Indications for urodynamic assessment
Treatment of stress incontinence
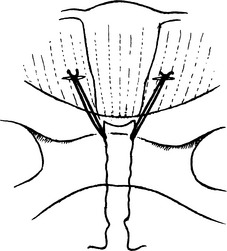
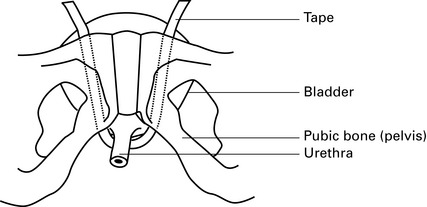
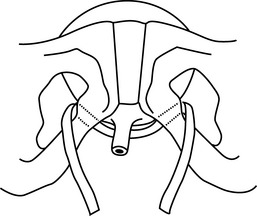
Surgical treatment of stress incontinence
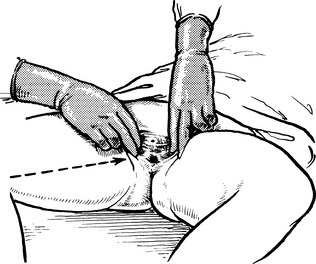
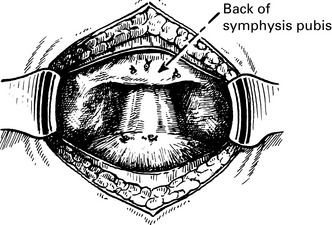
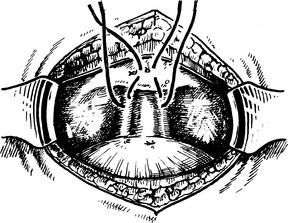
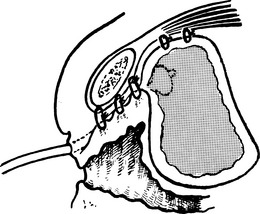
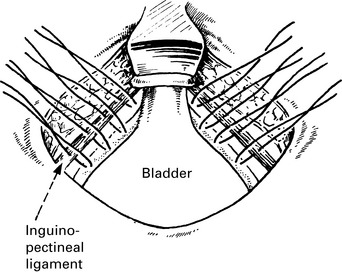
Marshall–marchetti–krantz urethropexy
Burch’s colposuspension operation
This operation elevates the anterior vaginal wall, bringing the urethra up with it.