Process Improvement and Patient Safety
Perspective
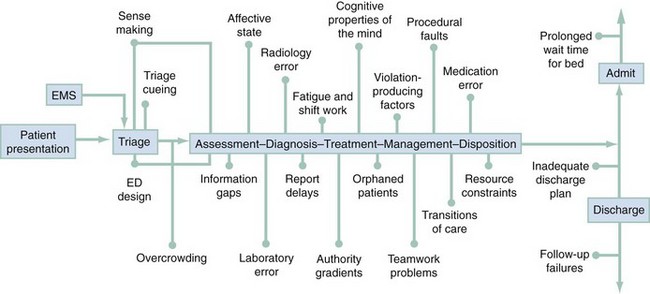
The overall process of patient care in the emergency department (ED) begins with the initial decision by the patient (or caregiver or family) to seek emergency assistance and ends with the patient’s disposition and follow-up. The care process is highly complex, with many separate components, people, and interfaces with other processes in the health care organization (Fig. 197-1). This complexity, among other things, provides many opportunities for process failures, “errors,” and adverse outcomes.
Although process failures in health care have been studied for decades, most of that effort originated from outside of the field of health care, with health care professionals largely unaware of it.1 This began to change in the early 1990s when the Harvard Medical Practice Study reported that almost 4% of hospitalized patients suffered significant adverse events during their care and that almost 30% of these were due to human error.2 The study noted that failures in ED care accounted for only approximately 3% of all adverse events, but more than 90% of adverse ED events were judged to be preventable. This study and others ultimately led the Institute of Medicine to issue a report in 1999 titled To Err Is Human: Building a Safer Health System.3 This report provoked the interest of the media and the general public and thrust the issue of safety in health care onto the national agenda. The major accomplishment of the Institute of Medicine report was the introduction of some of the fundamental concepts regarding safety in complex systems for the first time into the world of health care. The most transforming concept was the idea that failures (or errors) in care are not the result of bad decisions or bad individuals but are instead intrinsic properties of the processes of care in the health care system. Thus efforts to reduce these failures should be focused on changing the processes of care rather than on identifying, retraining, or punishing the workers.
The response within health care was mixed. Most health care professionals focused on the projected number of deaths due to error, arguing that they were either too high4,5 or too low,6 and a third, smaller group argued that the concept of error is essentially contestable and thus an approach aimed at counting errors is fundamentally flawed.7 The transforming concept of “system failure” rather than “human error” gradually gained acceptance, despite going against the natural human tendency to believe that individuals cause outcomes. This viewpoint is problematic because it undermines a clinician’s sense of free agency; health care providers prefer not to view themselves as trapped in a system that is moving inexorably toward a poor outcome.
Within emergency medicine, safety and quality have been addressed by task forces, interest groups, and special sections examining the practice of emergency care, its processes, and environments with tools from the “science of safety” to improve performance and to cultivate patient safety.8 A basic curriculum for teaching about safety at the undergraduate level was developed, with similar efforts taking place to implement safety concepts into medical education.9
Interesting lines of research on the safety and processes within emergency care have been performed, with a number of patient safety case reports published in the emergency medicine literature.10 Chisholm11 reported that emergency physicians are interrupted, on average, approximately once every 6 minutes and that two thirds of those interruptions cause a change in task; this is important because both interruptions and task switching frequently lead to process failures. Fordyce12 reported that self-detected errors occurred in almost 20% of all ED cases but that only 2% were associated with adverse events. Fordyce’s work emphasizes that errors are ubiquitous but only rarely combine with other factors to produce adverse events, and it supports the notion that focusing on elimination of errors is not likely to be a productive strategy for improvement.
Coiera13 studied emergency physicians in Australia and reported high communication loads and found similar levels of interruptions. Morey14 reported that specific training of emergency physicians and nurses to work together in teams led to reductions in failures and improved performance. Perry and colleagues15,16 identified a number of unexpected yet highly consequential failures of information technology that were difficult to detect, some occurring during emergency resuscitations. Wears and Perry17 noted ergonomic shortcomings in the workplace and pointed out their potential to contribute to failures in care. Hall18 identified significant delays related to ED layout, with time to assessment of chest pain patients being longer for patients placed behind a door or who were 25 feet or farther away from the physicians assigned to care. These examples of safety research in emergency care demonstrate the wide range of known and unknown contributors to patient safety and the importance of the work processes that overlay this complex work environment.
Sources of Failure in Emergency Care
Many characteristics of emergency medical practice make it vulnerable to failures (Table 197-1).19–26 This section focuses on some of the principal factors that contribute to adverse outcomes and how they might be better managed to improve safety.
Table 197-1
Characteristics of the Emergency Department That Affect Performance
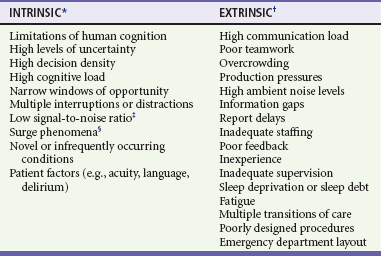
*Intrinsic factors are intimately part of the nature of emergency care and as such are not amenable to change but instead must be compensated for.
†Extrinsic factors are in principle manageable and typically relate to resource constraints.
‡Low signal-to-noise ratio refers to the low likelihood of a critical diagnosis compared with a benign diagnosis for similarly presenting symptoms and findings (e.g., subarachnoid hemorrhage vs. tension headache).
§Surge phenomena are the rapid changes in volume and acuity routinely experienced in many emergency departments.
Emergency Department Design, Human Factors, and Ergonomics
Two frequently overlooked contributors to lowered safety in any work environment are the design of the workspace and the engineering of the tools, technology, and procedures used to perform the work.27 This is especially true for EDs because the majority were not designed for the care actually being delivered there.28 ED caregivers are required to adapt to the space by creating “work-arounds” to cope with the limitations and impediments of the workspace.
Consistency is rarely found in equipment across or between areas. For instance, the blood pressure monitor in the ED is often not the same type or model as that used in the radiology department when the patient goes for diagnostic tests. In addition, tools and technology are seldom developed or assessed for their “user-centered design” or ability to be integrated into existing workspace and the associated hazards for doing so. This is most apparent with regard to health information technology, which is often introduced for improvement of safety and quality; however, embedded latent features that can produce clinical failures that are “hard to see” have been demonstrated.29,30 Study of computerized physician order entry by Koppel31 showed that the software facilitated 22 types of medication error risks, for example, displays that prevented a coherent view of the patients’ medications and inflexible ordering formats that generated wrong orders. Other contributors to information technology failure within health care are the lack of usability testing,32 delays in in-service training, and failure to reassess the impact of the new technology and changes in clinical work after implementation.33
The contribution of poor design to the difficulty in maintaining safety in a health care environment is generally overlooked by staff members, who cope with these difficulties as “part of the job.”17 Vigilance is the common solution but despite caregivers’ best efforts cannot be sustained, given competing demands for their attention. This increases the risk of a failure’s not being recognized as linked to the workplace, the procedures, or the equipment, despite being “tightly coupled” to any or all of these.
Overcrowding
ED crowding has long been recognized as a major source of time-delay failures and a threat to patient safety.34,35 Such delays are not simply an inconvenience to the patient but may give rise to significant adverse events. For example, patients with atypical presentations of severe illness who have been mis-triaged to low levels of acuity may experience inordinate and, occasionally, fatal delays. In other cases, such as community-acquired pneumonia, cellulitis, and lacerations, more expedient care may significantly improve the outcome of the illness. A significant proportion of patients who leave the ED without being seen may have serious illness and incur delays in diagnosis and treatment. At the other end of the process, when the patient is ready for admission to the hospital from the ED, further time-delay errors may occur (see Fig. 197-1). Not only do such delays create throughput problems for the ED and contribute to overcrowding by front-end loading or “entry block,” but they also give rise to discontinuities in care and may lead to adverse events that are difficult to identify because they are manifested once the patient has left the ED.36–39 Manifestations of cognitive overload associated with ED overcrowding are diminished overall with increased use of heuristics (mental shortcuts) in medical decision-making and more biased and risk-laden decisions.
Information Gaps
Missing information is common in emergency care and can significantly affect quality of care.40 Hospital records, especially discharge summaries, details of past medical history, and other important information, are often difficult to access in an expedient manner, even with electronic medical records. Referral notes sent by family physicians with the patient may not reach the emergency physician or may not contain relevant or significant details. In these situations, emergency physicians make clinical decisions and take action on the basis of incomplete, limited, or erroneous information. Emergency clinicians often end up not seeking additional or clarifying information because of time pressures, patient volume, or limited methods to obtain more information (e.g., the referring physician’s office is closed), essentially accommodating to this “gap” in continuity of care and the associated increase in patient risk.41
Performance-Shaping Factors
Blaming individuals for errors contributes little to an understanding of risk, vulnerability, and failure. A wide variety of ambient, systemic conditions in the ED contribute to the majority of adverse events and near misses that occur (see Table 197-1). Some performance-shaping factors can be considered to be “intrinsic,” part and parcel of the milieu of emergency medicine and thus not amenable to direct control (e.g., cognitive workload, multiple distractions and interruptions, and high acuity). These factors must be managed by strategies to buffer or to mitigate their effects. In contrast, other “extrinsic” performance-shaping factors typically reflect limitations of resources (e.g., staffing ratios, production pressure, and ED layout). When resources are limited, a tradeoff can occur in the ability of the ED to provide safety and quality in patient care. This condition is referred to as RACQITO (resource availability continuous quality improvement trade-off),42 a concept derived from speed-accuracy tradeoffs described in industrial settings.
Violation-Producing Factors
Although at first one might think that violations of organizational policies, rules, and procedures would always be causes of failures and adverse events, the modern approach to safety has pointed out that some violations are actually necessary for the safe functioning of the system, and others fall somewhere in between.43 Aside from recklessness, drug use on the job, moral failings, and other egregious acts, research in other domains has identified other factors that are associated with the occurrence of rule and safety violations (Box 197-1). The “normalization of deviance”44 is an accumulated tolerance of small variances from safe operating conditions that develops over time, ultimately compromising safety. This is evidenced in overtaxed EDs coping with overcrowding of patients (e.g., performing evaluation and management of patients in hallways). Violations can also occur in response to perceptions of authority. They may occur through a directive supporting violation from an authority figure (e.g., nursing supervisors order admitted patients moved to inpatient beds without calling to report if there are delays in reaching inpatient nurses), the absence of a disapproving authority (e.g., physicians leaving shifts early and the medical director does not address the behavior), or an individual’s self-perception that he or she is authorized to disregard or to deviate from prescribed procedures (e.g., ED electrocardiograms done on patients in chairs because there are no available stretchers).
Fluctuations in mood can also contribute to violations for a variety of reasons and will result in inconsistent clinical performance; men are more likely to break safety rules and to engage in more risk-taking behavior than women are.43 Risk-seeking and risk-averse attitudes are associated aspects of decision-making in the ED.45
Teamwork
Good teamwork is essential to the safe practice of emergency medicine, but emergency caregivers are not trained or evaluated as teams. Teamwork training in other fields, such as aviation, has been successful in reducing failures related to poor communication, cross-monitoring (observing others’ behaviors to reduce risk of failure and share workload), and authority gradients (both within and between professions).46 Work on transferring teamwork training principles to emergency medicine suggested that teamwork failures are involved in approximately 40% of malpractice cases.47 The lack of cross-monitoring across team members and the failure of advocacy or assertion on behalf of the patient by caregivers to avoid patient harm were two of the factors most frequently identified. A multidisciplinary teamwork training course implemented in nine EDs showed a significant improvement in quality of team behaviors and a sixfold decrease in observed clinical errors.14 Teamwork is not a specific fix for any one type of error, but it should be viewed as one type of adaptable human factor intervention with a set of teachable skills and behaviors capable of increasing system resilience and safety, which are hallmarks of high-reliability organizations.48
Teamwork training requires a change of culture, which can be difficult for ED staff. Institutional and ED leadership must be fully committed to the process before implementation of teamwork training for all staff. Resistance to behavioral change is likely to be encountered, and it will be necessary to demonstrate the clinical relevance of this training. High-fidelity medical simulation supported by audiovisual feedback offers the educational methodology to help clinicians and staff understand the necessity of behavioral change.49 A major unanswered question is how to embed teamwork behaviors into medical training and how to sustain the behaviors over time.
Authority Gradients
Almost all human groups have some form of authority gradient among members. This hierarchy can be based on profession (e.g., physicians have greater authority than nurses) or organizational rank (e.g., attending physicians have more authority than residents). Ideally, information between team members should flow freely, but this may not occur if low-authority members are inhibited by differences in seniority, stature, expertise, profession, or social status. There are clear examples of cases in which authority gradients have been responsible for adverse events.50 A work environment in which all team members feel comfortable expressing their viewpoint, especially if it is a dissenting one, requires cultural change that can begin with the physicians who occupy the highest authority position in the clinical setting. Authority figures have the ability to initiate change by recognizing the value of perspectives other than their own and eliciting them from other clinicians and staff (e.g., asking a patient’s nurse what he or she thinks may be going on with the patient). Senior clinicians are in a powerful position to bridge gradients by fostering open communication through multidisciplinary rounds, demonstrating that they are approachable (e.g., acknowledging staff by name), and using clinical narratives from their own experience that illustrate near misses and judgment failures.51
Cognitive and Affective Limitations
The human mind has characteristic dispositions to respond to particular stimuli and contexts in specific ways. A great deal of effort has gone into identifying and describing these; more than 50 cognitive dispositions to respond have been described.17,52–54 A number of strategies have been proposed to reduce the adverse outcomes associated with cognitive dispositions to respond.55
The overall process of patient care in the ED is driven by a process of making clinical sense out of multiple sets of fragmented, tangential, and interrupted stimuli. This is aimed at making an accurate diagnosis if possible or, more commonly, a useful framing of the problem, which can determine management and disposition. Although many diagnoses, such as lacerations, dislocations, fractures, and foreign bodies, are self-evident, others (e.g., chest pain, fever, headache, abdominal pain, and syncope) are often associated with high levels of diagnostic uncertainty and are more likely to lead to problems. Cognitive biases can frequently be identified in retrospect after diagnostic failures,56 but the problem of hindsight bias makes this identification problematic.57
In addition to cognitive mental properties, the emotional state of the physician can affect his or her decision-making; this has been referred to as visceral bias.17,53 Relatively little attention has been directed to the important role of affective bias in decision-making. Although processes such as countertransference, fundamental attribution error,42 and the economy of perception that underlies stereotyping are well understood in psychology, health care workers are typically less aware of them (e.g., “She’s a drug seeker,” “He’s a frequent flyer,” and “She just wants attention”) and their effect on clinical interactions.58
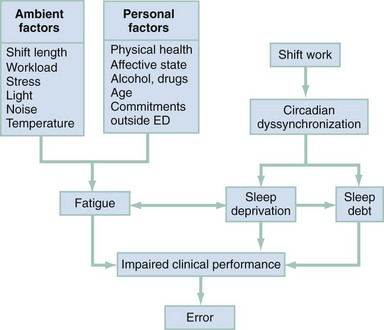
Fatigue and Shift Work
Both fatigue and shift work contribute to performance failures,59 but relatively little research has been directed to their respective impacts on clinical performance in the unique milieu of the ED.60 Although the two are often considered together, they are different entities and exert both qualitatively and quantitatively different effects on performance.61 Fatigue has a number of determinants separate from those associated with shift work (Fig. 197-2).
Shift work has extensive, well-documented, detrimental effects on health that in turn have an impact on well-being and job performance.62 Importantly, it leads to disruption of circadian rhythms that inevitably result in sleep deprivation. Circadian dyssynchronicity largely occurs through missing sleep in the anchor period, approximately midway through the sleep phase when core temperature and arousal level are at their lowest. It has been stated that the performance degradation of someone who has been up all night is roughly equal to that of a person with a blood alcohol level of 0.1% (Box 197-2).63
The acute effects of sleep deprivation are well known, but the chronic effects are less appreciated. Invariably, working a night shift results in less sleep the following day, and subsequent sleep is often disrupted and fragmented in the struggle to restore the circadian rhythm before the night-shift cycle repeats itself. This results in the accumulation of a sleep debt that has a significant impact on performance. A study of anesthesia residents on a normal work schedule, with no on-call duty in the preceding 48 hours, showed daytime sleepiness scores comparable to those of patients with narcolepsy or sleep apnea.64 The on-call schedule of these subjects (five periods per month) entailed considerably less sleep deprivation and fragmentation than an average emergency physician’s schedule. Increasing age is associated with decreased tolerance for sleep deprivation.65
Performance declines as work hours increase,66 but the optimal shift length in the ED is unknown and difficult to delineate for several reasons. The relationship with workload or acuity is not well appreciated, and some workers exhibit contradictory incentives, such as preferring to work longer shifts to get more days off. More recovery time between shifts might be expected to enhance job performance, but these issues remain relatively unexplored. A survey of emergency physicians found a preference for 8-hour over 12-hour shifts,67 but it is not known whether job satisfaction in the ED translates into improved clinical performance and fewer adverse events. Other ambient conditions within the ED, competing commitments outside the ED, age, ill health, and other factors contribute to fatigue, with evidence pointing toward additional health implications for emergency physicians.68,69
The appropriate management of shift work and fatigue to improve patient safety is not well understood, and further research is needed in this area. In most high-hazard industries, the assumption is that fatigue and long, aberrant work hours lead to poor performance; however, in the health care industry, concerns about discontinuity of care and difficulties in changing medical culture have obscured these issues. Given that medical personnel, like all human beings, function suboptimally when they are fatigued, efforts to reduce fatigue and sleepiness should be undertaken, and the burden of proof should be in the hands of the advocates of the current system to demonstrate that it is safe.63 In the meantime, shift scheduling should be optimized to reduce the impact of circadian disruption, and ED personnel should practice good sleep hygiene. Some basic approaches are listed in Box 197-3.62,66
Problem Areas in Emergency Care
Triage
Triage assessments are important contributors to process failures and adverse events. Beyond treatment delays, which can occur with undertriage or be produced by overtriage, an incorrect assessment may be the triggering event that initiates a chain of failures. Geography can become destiny, and an inappropriate triage to a specific treatment area may create a bias in the minds of the treating clinicians and staff. The use of five-level triage systems for adults and children, with excellent inter-rater reliability, offers an opportunity to reduce the risk associated with undertriage.70,71
Technical Procedures
The practice of emergency medicine requires proficiency in a wide range of procedures with varying degrees of difficulty. Patients who require procedures are at greater risk for adverse events.12 Contributors to this higher risk include not only problems with proficiency but also a low frequency for use of higher risk procedures. Critical procedures, such as cricothyrotomy, pericardiocentesis, and endotracheal intubation, are rarely performed in many EDs. When they are needed, they are highly consequential events under significant time pressure for intervention, therein reducing opportunity to refresh skills before the procedure is performed. An important challenge in emergency medicine is the acquisition and especially the maintenance of a requisite level of skill. Simulation techniques have considerable potential here72 but require both capital and human investment to be effective.
Laboratory
The interface between the ED and its ancillary services is critically important. Failures can occur at three phases of laboratory processes. Preanalytic errors mostly occur through inappropriate collection of specimens because of lapses in technique, timing, and identification of both patient and specimen. Analytic errors refer to those that arise directly from the testing process. Postanalytic errors occur after the test result has been obtained and can take many forms (e.g., keyboard entry errors, overlooked or lost data, and failure of results to reach the physician). Studies of a blood bank and a stat laboratory found that the majority of failures occurred in the preanalytic and postanalytic stages, with less than 5% in the analytic stage.73,74 Overall, the laboratory defect rate is less than 1%, but the number of exposures is large. Of the failures that do occur, up to 50% may have a moderate impact and up to 8% a severe impact on patient care.75
Radiology
Radiographic imaging is a critical aspect of diagnosis and management in the ED. Although patient identification and wrong-side problems are important sources of failure, the majority lie in interpretation. Assuming the radiologist’s interpretation to be the criterion standard, the rate of errors in interpretation by emergency physicians and residents may be as high as 16% for plain radiographs and more than double that rate for computed tomography scans.76 Clearly, not all misinterpretations are consequential, and emergency physicians typically seek the advice of the radiologist when they recognize difficult interpretations. The introduction of digital imaging and picture archiving communications systems has resulted in new patient safety issues related to usability, the effect of monitor resolution on interpretation, and reconciliation of ED physician and radiology readings.77 Significant interpretation errors can be detected with prompt review of all films by the emergency physician and radiologist, but effective procedures are required to ensure that timely and appropriate feedback and review occur. This approach has been demonstrated to substantially reduce the rate of clinically important misinterpretations.78
Transitions in Patient Care
There has been little study of these transitions of care, despite their ubiquity and importance to the specialty.20,79 Sign-overs are highly variable in their content, the number of individuals involved, the physical configuration (e.g., walking, stationary, and at bedside), the tools used to facilitate the transition (e.g., white boards, medical records, and written notes), and the length of the transition process. Although widely regarded as providing a major contribution to adverse events, sign-overs also provide an opportunity for review of decision-making by clinicians and may provide opportunities for recovery by bringing “fresh eyes” to a patient’s case.20,79
Potential threats to high-quality transitions include the following:
• Interruptions during the turnover (e.g., phone calls and sidebar conversations) can cause a loss of focus and lead to the omission of important information.
• Lack of consistent structure to the turnover: Although the traditional case presentation narrative is generally followed (chief complaint, history, physical examination, initial laboratory results, impression, and plan), the case presentation format does not automatically remind participants of pending or as yet uncompleted tasks.
• Patients are commonly “marked” in ways that can sometimes be helpful but sometimes harmful, especially for at-risk groups such as the homeless, psychiatric patients, alcoholics, and drug abusers.
Orphaned Patients
Orphaned patients are those who have suffered temporary loss or diminished supervision or accountability for their ED care. This may occur at several stages in the process. Patients who are seen and assessed at triage and then wait in the waiting area are temporarily orphaned. Those who are brought in by paramedics sometimes remain on stretchers for hours before being admitted to the ED. Patients who leave without being seen or before treatment is completed have “orphaned” themselves. Patients can also be temporarily orphaned out of the ED for radiographic studies or other special tests. On occasion, patients get “lost in the shuffle” and are overlooked at shift change, or they may get “lost” after one or more consultations with other services. With prolonged wait times, occult conditions can mature to serious and potentially catastrophic levels. A significant cause of orphaning in some EDs is the “boarding” of admitted patients because no inpatient beds are available. In such cases, patients may be put in holding areas in or adjacent to the ED and receive sporadic care from a succession of caregivers who know increasingly less about their conditions. The risk of harm to patients caught in this “gap” within the ED is not well studied.41,80
Medications
Medication errors constitute the largest proportion of failures in most general studies, with failures occurring in all six steps of the process (prescription, transcription, dispensing, administration, monitoring, and discharge).81 Many EDs take on the dispensing role, obviating input from the pharmacy, where many errors are corrected. In addition, team communication errors can contribute to many failures: missed medications, wrong medications, and duplicate dosing. Pediatric patients are at higher risk; drug errors are no more common than in adults, but they are typically more serious.82,83
The presence of a pharmacist on the clinical team has been shown to reduce medication errors in several settings.84 There is great interest in the potential for computer technologies, such as bar coding and computerized physician order entry, to enhance medication safety. However, despite some successful demonstrations, widespread implementation has not occurred, and there is evidence that such systems introduce new problems to replace old ones.85 The Institute for Safe Medication Practices has recommended that certain problem practices be avoided in writing orders or prescriptions.86 Success in this area will require more than just individual attentiveness; nurses, unit secretaries, and pharmacists will have to feel comfortable challenging improper use by physicians.
Conclusion
The safe management of patients in the ED depends on a multiplicity of processes. All appear vulnerable to failure, yet all have the potential for improvement through judicious process management. Efforts by front-line workers will not be sufficient, and so considerable effort will be required at the administrative or “blunt end” of the system.87
References
1. Bosk, C. Forgive and Remember: Managing Medical Failure. Chicago: University of Chicago Press; 1979.
2. Brennan, TA, et al. Incidence of adverse events and negligence in hospitalized patients: Results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324:370.
3. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press, 1999.
4. McDonald, CJ, Weiner, M, Hui, SL. Deaths due to medical errors are exaggerated in Institute of Medicine report. JAMA. 2000;284:93.
5. Dunn, JD, Wears, RL. The November special issue on errors [letter]. Acad Emerg Med. 2001;8:686.
6. Leape, LL. Institute of Medicine medical error figures are not exaggerated. JAMA. 2000;284:95.
7. Wears, RL. Beyond error. Acad Emerg Med. 2000;7:1175.
8. Wears, RL. The science of safety. In: Zipperer L, ed. Lessons in Patient Safety. Chicago: National Patient Safety Foundation; 2001:1–7.
9. Cosby, KS, Croskerry, P. Patient safety: A curriculum for teaching patient safety in emergency medicine. Acad Emerg Med. 2003;10:69.
10. Croskerry, P, Shapiro, MJ. “Profiles in patient safety”: A new feature. Acad Emerg Med. 2002;9:324.
11. Chisholm, CD, Collison, EK, Nelson, DR, Cordell, WH. Emergency department workplace interruptions: Are emergency physicians “interrupt-driven” and “multitasking”? Acad Emerg Med. 2000;7:1239.
12. Fordyce, J, et al. Errors in a busy emergency department. Ann Emerg Med. 2003;42:324.
13. Coiera, EW, et al. Communication loads on clinical staff in the emergency department. Med J Aust. 2002;176:415.
14. Morey, JC, et al. Error reduction and performance improvement in the emergency department through teamwork training: Evaluation results of the MedTeams project. Health Serv Res. 2002;37:1553.
15. Perry, SJ, Wears, RL, Cook, RI. The role of automation in complex system failures. J Patient Saf. 2005;1:56.
16. Perry SJ, et al: Ironies of improvement: Organizational factors undermining resilient performance in healthcare. Paper presented at IEEE International Conference on Systems, Cybernetics and Man; October 7-11, 2007; Montreal, Canada.
17. Wears, RL, Perry, SJ. Human factors and ergonomics in the emergency department. Ann Emerg Med. 2002;40:206.
18. Hall, KK, Kyriacou, DN, Handler, JA, Adams, JG. Impact of emergency department built environment on timelines of physician assessment of patients with chest pain. Environ Behav. 2008;40:233.
19. Croskerry, P. Achieving quality in clinical decision making: Cognitive strategies and detection of bias. Acad Emerg Med. 2002;9:1184.
20. Beach, C, Croskerry, P, Shapiro, M. Profiles in patient safety: Emergency care transitions. Acad Emerg Med. 2003;10:364.
21. Chisholm, CD, Pencek, AM, Cordell, WH, Nelson, DR. Interruptions and task performance in emergency departments compared with primary care offices. Acad Emerg Med. 1998;5:470.
22. Croskerry, PG, Wears, RL. Safety in emergency medicine. In: Markovchick V, Pons P, eds. Emergency Medicine Secrets. 3rd ed. Philadelphia: Hanley & Belfus; 2003:1023–1028.
23. Gaba, DM, Howard, SK. Patient safety: Fatigue among clinicians and the safety of patients. N Engl J Med. 2002;347:1249.
24. Derlet, R, Richards, J, Kravitz, R. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med. 2001;8:151.
25. Stiell, A, Forster, AJ, Stiell, IG, van Walraven, C. Prevalence of information gaps in the emergency department and the effect on patient outcomes. CMAJ. 2003;169:1023.
26. Croskerry, P. The feedback sanction. Acad Emerg Med. 2000;7:1232.
27. Gosbee, J. Human factors engineering and patient safety. Qual Saf Health Care. 2002;11:352.
28. Perry, SJ, Hall, KK. Emergency department design and patient safety: Tracking the trade-offs. In: Croskerry P, Cosby IC, Schenkel S, Wears RL, eds. Patient Safety in Emergency Medicine. Philadelphia: Lippincott Williams & Wilkins; 2008:106–111.
29. Wears, RL. More on computer glitches and laboratory test reporting. http://catless.ncl.ac.uk/Risks/23.64.html#subj4, 2004.
30. Y2K Flaw blamed for Down’s syndrome test errors. http://catless.ncl.ac.uk/Risks/21.67.html#subj14.
31. Koppel, R, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293:1197.
32. Fairbanks, RJ, Caplan, S. Poor interface design and lack of usability testing facilitate medical error. In: Gosbee JW, Gosbee L, eds. Using Human Factors Engineering to Improve Patient Safety. Oakbrook Terrace, Ill: Joint Commission Resources; 2005:105–113.
33. Nemeth, C, et al. Getting to the point: Developing IT for the sharp end of healthcare. J Biomed Inform. 2005;38:18.
34. Richardson, LD, Asplin, BR, Lowe, RA. Emergency department crowding as a health policy issue: Past development, future directions. Ann Emerg Med. 2002;40:388.
35. Wears RL, Perry SJ, Nasca L: “Free Fall”—Highly Decentralized, Resilient Adaptation to Demand-Capacity Mismatches in an Emergency Department. Paper presented at the eighth International Naturalistic Decision-Making Conference; June 4-6, 2007; Pacific Grove, Calif.
36. Huang, DT. Clinical review: Impact of emergency department care on intensive care unit costs. Crit Care. 2004;8:498.
37. Sprivulis, PC, et al. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006;184:208.
38. Gilligan, P, et al. The Boarders in the Emergency Department (BED) study. Emerg Med J. 2008;25:265.
39. Burgess, DJ. Are providers more likely to contribute to healthcare disparities under high levels of cognitive load? How features of the healthcare setting may lead to biases in medical decision making. Med Decis Making. 2010;30:246–257.
40. Stiell, IG, et al. The Canadian CT head rule for patients with minor head injury. Lancet. 2001;357:1391.
41. Cook, RI, Render, M, Woods, DD. Gaps in the continuity of care and progress on patient safety. BMJ. 2000;320:791.
42. Croskerry, P. The cognitive imperative: Thinking about how we think. Acad Emerg Med. 2000;7:1223.
43. Reason, J. Managing the Risks of Organizational Accidents. Aldershot, UK: Ashgate; 1997.
44. Vaughan, D. The Challenger Launch Decision: Risky Technology, Culture and Deviance at NASA. Chicago: University of Chicago Press; 1996.
45. Pearson, SD, et al. Triage decisions for emergency department patients with chest pain: Do physicians’ risk attitudes make the difference? J Gen Intern Med. 1995;10:557.
46. Helmreich, RL, Merritt, AC. Culture at Work in Aviation and Medicine. Aldershot, UK: Ashgate; 1998.
47. Risser, DT, et al. The potential for improved teamwork to reduce medical errors in the emergency department. The MedTeams Research Consortium. Ann Emerg Med. 1999;34:373.
48. Grabowski, M, Roberts, K. Risk mitigation in large-scale systems: Lessons from high reliability organizations. Calif Manage Rev. 1997;39:152.
49. Small, SD, et al. Demonstration of high-fidelity simulation team training for emergency medicine. Acad Emerg Med. 1999;6:312.
50. Vincent, C. Hemivulvectomy: The wrong side removed. www.webmm.ahrq.gov/case.aspx?caseID=33, 2003.
51. Chisholm, CD, Croskerry, P. A case study in medical error: The use of the portfolio entry. Acad Emerg Med. 2004;11:388.
52. Campbell, SG, Croskerry, P, Bond, WF. Profiles in patient safety: A “perfect storm” in the emergency department. Acad Emerg Med. 2007;14:743.
53. Croskerry, P. Commentary: The affective imperative: Coming to terms with our emotions. Acad Emerg Med. 2007;14:184.
54. Croskerry, P. Cognitive and affective dispositions to respond. In: Croskerry P, Cosby KS, Schenkel S, Wears R, eds. Patient Safety in Emergency Medicine. Philadelphia: Lippincott, Williams & Wilkins; 2008:219–227.
55. Croskerry, P. Cognitive forcing strategies in clinical decision making. Ann Emerg Med. 2003;41:110.
56. Graber, M, Gordon, R, Franklin, N. Reducing diagnostic errors in medicine: What’s the goal? Acad Med. 2002;77:981.
57. Henriksen, K, Kaplan, H. Hindsight bias, outcome knowledge and adaptive learning. Qual Saf Health Care. 2003;12:46ii.
58. Croskerry, P, Abbass, A, Wu, A. Emotional issues in patient safety. J Patient Saf. 2010;6:1–7.
59. Miller, DP, Swain, AD. Human error and human reliability. In: Salvendy G, ed. Handbook of Human Factors. New York: Wiley; 1986:219.
60. Rollinson, DC, et al. The effects of consecutive night shifts on neuropsychological performance of interns in the emergency department: A pilot study. Ann Emerg Med. 2003;41:400.
61. Dodge, R. Circadian rhythms and fatigue: A discrimination of their effects on performance. Aviat Space Environ Med. 1982;53:1131.
62. Croskerry, P. Shiftwork, fatigue, and safety in emergency medicine. In: Croskerry P, Cosby KS, Schenkel S, Wears R, eds. Patient Safety in Emergency Medicine. Philadelphia: Lippincott Williams & Wilkins; 2008:259–268.
63. Bonnet, MH. Sleep deprivation. In: Kryger M, Roth T, Dement WC, eds. Principles and Practice of Sleep Medicine. Philadelphia: WB Saunders; 2000:53–71.
64. Howard, SK. Sleep deprivation and fatigue: Are we sleepy people keeping people asleep? CSA Bull. 2000:49.
65. Reid, K, Dawson, D. Comparing performance on a simulated 12 hour shift rotation in young and older subjects. Occup Environ Med. 2001;58:58.
66. Jha, AK, Duncan, BW, Bates, DW, Fatigue, sleepiness, and medical errors, Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Agency for Healthcare Research and Quality: Rockville, Md, 2001. www.ahcpr.gov/clinic/ptsafety/chap46a.htm.
67. Thomas, H, Jr., Schwartz, E, Whitehead, DC. Eight- versus 12-hour shifts: Implications for emergency physicians. Ann Emerg Med. 1994;23:1096.
68. Okamoto, H, et al. An occupational health study of emergency physicians in Japan: Health assessment by immune variables (CD4, CD8, CD56, and NK cell activity) at the beginning of work. J Occup Health. 2008;50:136.
69. Gaba DM: Physician work hours: The “sore thumb” of organizational safety in tertiary health care. Proceedings of the Second Annenberg Conference on Enhancing Patient Safety and Reducing Errors in Health Care. Rancho Mirage, Calif: National Patient Safety Foundation; 1998:142.
70. Tanabe, P, Gimbel, R, Yarnold, PR, Adams, JG. The Emergency Severity Index (version 3) 5-level triage system scores predict ED resource consumption. J Emerg Nurs. 2004;30:22.
71. Maningas, PA, Hime, DA, Parker, DE. The use of the Soterion Rapid Triage System in children presenting to the emergency department. J Emerg Med. 2006;31:353.
72. Jha, AK, Duncan, BW, Bates, DW, Simulator-based training and patient safety, Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Agency for Healthcare Research and Quality: Rockville, Md, 2001. www.ahcpr.gov/clinic/ptsafety/chap45.htm.
73. Boone, DJ, et al. Transfusion medicine monitoring practices: A study of the College of American Pathologists/Centers for Disease Control and Prevention Outcomes Working Group. Arch Pathol Lab Med. 1995;119:999.
74. Carraro, P, Plebani, M. Errors in a stat laboratory: Types and frequencies 10 years later. Clin Chem. 2007;53:1338.
75. Bonini, P, Plebani, M, Ceriotti, F, Rubboli, F. Errors in laboratory medicine. Clin Chem. 2002;48:691.
76. Kripalani, S, Williams, MV, Rask, K, Reducing errors in the interpretation of plain radiographs and computed tomography scans, Making Health Care Safer: A Critical Analysis of Patient Safety Practices. Agency for Healthcare Research and Quality: Rockville, Md, 2001. www.ahcpr.gov/clinic/ptsafety/chap35.htm.
77. Fairbanks, RJ, Perry, SJ, Venturino, M, Zwemer, FL. Radiology in the emergency department: Patient safety issues with digital imaging. In: Croskerry P, Cosby IC, Schenkel S, Wears RL, eds. Patient Safety in Emergency Medicine. Philadelphia: Lippincott Williams & Wilkins; 2008:133–138.
78. Espinosa, JA, Nolan, TW. Reducing errors made by emergency physicians in interpreting radiographs: Longitudinal study. BMJ. 2000;320:737.
79. Wears, RL, et al. Shift changes among emergency physicians: Best of times, worst of times. Denver, Colo: Human Factors and Ergonomics Society; 2003.
80. Falvo, T, et al. The opportunity loss of boarding admitted patients in the emergency department. Acad Emerg Med. 2007;14:332.
81. Croskerry, P, et al. Profiles in patient safety: Medication errors in the emergency department. Acad Emerg Med. 2004;11:289.
82. Selbst, SM, Fein, JA, Osterhoudt, K, Ho, W. Medication errors in a pediatric emergency department. Pediatr Emerg Care. 1999;15:1.
83. Kaushal, R, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285:2114.
84. American Society of Health-Systems Pharmacists. Top-priority actions for preventing adverse drug events in hospitals. Recommendations of an expert panel. Am J Health Syst Pharm. 1996;53:747.
85. Ash, JS, Berg, M, Coiera, E. Some unintended consequences of information technology in health care: The nature of patient care information system–related errors. J Am Med Inform Assoc. 2004;11:104.
86. Koppel, R, et al. Workarounds to barcode medication administration systems: Their occurrences, causes, and threats to patient safety. J Am Med Inform Assoc. 2008;15:408.
87. Abbreviations to avoid. ISMP Medication Safety Alert. 2001;6:1.