48 Procedures for Vascular Access
VASCULAR CANNULATION is an important procedure in the anesthetic and perioperative management of children. Its routine use was introduced in the 1950s.1 The indications are to provide routes for fluid, drug, and blood product administration, monitoring of cardiopulmonary function, and provision of access for blood sampling. Although the technique of insertion may be extremely difficult, especially in the very young or small child, no child should be denied an indicated procedure because of an operator’s inexperience; appropriate consultation should be sought, if necessary. Regardless of the procedure, gloves should be worn to maintain clean or sterile technique and to protect health care professionals from exposure to blood.2–6 An update from the Pediatric Perioperative Cardiac Arrest Registry suggests that lack of good vascular access may contribute to the underestimation of fluid or blood loss and inadequate replacement of fluid or blood in anesthetized children, emphasizing the importance of appropriate and adequate vascular access and monitoring.7,8
Venous Cannulation
Peripheral Intravenous Cannulation
Indications
Percutaneous intravenous cannulation should be used in almost all anesthetized children for the following purposes9,10:
 Provision of a route for postoperative pain relief
Provision of a route for postoperative pain relief
 Administration of drugs, fluids and electrolytes, glucose, and blood products, including resuscitation medications
Administration of drugs, fluids and electrolytes, glucose, and blood products, including resuscitation medications
 Indirect central venous pressure measurement; the accuracy of this method for central venous pressure measurement does not appear to vary by location of the catheter11 but does depend on ensuring direct continuity between the central and peripheral circulation.12,13 This can be assessed by providing a large, sustained inspiration or occluding the venous return of the extremity, which both cause an increase in the peripheral pressure.14–16 Hypothermia may impair the accuracy of such measurement.17
Indirect central venous pressure measurement; the accuracy of this method for central venous pressure measurement does not appear to vary by location of the catheter11 but does depend on ensuring direct continuity between the central and peripheral circulation.12,13 This can be assessed by providing a large, sustained inspiration or occluding the venous return of the extremity, which both cause an increase in the peripheral pressure.14–16 Hypothermia may impair the accuracy of such measurement.17
Equipment
 Alcohol pads or chlorhexidine swabs
Alcohol pads or chlorhexidine swabs
 Clear plastic dressing (Tegaderm, 3M Medical-Surgical Division, St. Paul, Minn., or OpSite, Smith + Nephew, Inc., Largo, Fla.)
Clear plastic dressing (Tegaderm, 3M Medical-Surgical Division, St. Paul, Minn., or OpSite, Smith + Nephew, Inc., Largo, Fla.)
Consider the possible need for latex-free equipment. In cases of difficult access, the availability of a transillumination light source (Karl Storz, 485 B Type, Tutlingen, Germany) may improve the success rate of catheter placement.18 Ultrasonography also may be used for obtaining peripheral venous access at the basilic, cephalic, or brachial veins.19,20 Finally, new near-infrared and infrared technology is available to aid in the identification of peripheral veins (AccuVein, Accuvein, Huntington, N.Y.; VeinViewer, Christie Digital Systems, Cypress, Calif.).21
Practical Suggestions
1. Awake intravenous line placement can be facilitated by any combination of good patient rapport, EMLA cream (lidocaine 2.5% and prilocaine 2.5%), lidocaine and tetracaine patch, lidocaine by iontophoresis, lidocaine by topical cream, topical tetracaine (Ametop), ethyl chloride spray, and/or pre-medication.22–31
2. Prefilling the cannula with saline may reduce menisci tension and allow a more rapid blood flash back.
3. A butterfly needle can be inserted for induction, followed by an appropriate-size catheter after anesthesia.
4. A T-connector (Abbott Hospitals, Inc., Chicago) may be used to minimize the fluids necessary to flush drugs administered through the intravenous line; this is particularly important for infants.32
5. A calibrated burette should be used to limit the total infusion and provide a means to titrate fluids accurately in infants and young children.
6. A flow-limiting infusion pump may be used for preterm and full-term neonates.
7. Flow rates may be significantly changed by catheter brand, tubing type, and addition of extensions and stopcocks.33
8. One-way valves in the intravenous tubing are useful in preventing back-flow of drugs or infusions.
9. Air filters also may be useful for children at risk for paradoxical gas embolization.
Complications
Hematoma from a failed vascular cannulation is usually of no serious consequence. Infection or thrombosis may be limited by aseptic technique.34–36 One study of 642 Teflon catheters in 525 patients showed that the risk of catheter complications in children was extremely small and would not be reduced significantly by routine replacement of the catheters.37 Catheter life span has been found to be unrelated to insertion site, cannula size, or brand in infants younger than 12 months of age.38,39
Skin sloughing is usually caused by subcutaneous infiltration of calcium, potassium, or hypertonic solutions; it may be avoided by frequent inspection of the intravenous line before injecting medications.40 The risk of subcutaneous infiltration increases with the administration of medications versus no medications and with parenteral nutrition solutions compared with 5% or 10% dextrose solutions, but the risk of infiltration is no different with solutions that contain potassium (≤20 mEq/L vs. >20 mEq/L). In addition, there is no difference between gravity-controlled versus infusion delivery devices.41
There are insufficient data to support the routine use of heparin to prolong the patency of peripheral intravenous catheters in neonates and children.42
Central Venous Pressure Measurement
Some studies in children and adults describe a reasonable correlation between peripheral intravenous catheters and central venous catheters, even in critically ill children. Hypothermia (peripheral vasoconstriction) decreases the accuracy of such measurements, but it is useful to understand that transducing the pressure of a peripheral vein may provide valuable information regarding right-sided cardiac filling pressures.9,10,43–46
Establishing a Large Intravenous Catheter in Small Patients
Indications
1. Prepare and drape the appropriate area using standard sterile techniques.
2. Perform a standard intravenous cannulation of an antecubital, saphenous, or external jugular vein with a small (22-gauge) intravenous catheter.
3. Pass a small, flexible guidewire (0.018 inch) through the intravenous catheter, remove the catheter, and with a number 11 blade make a small incision at the entry point of the wire at the skin.
4. Pass the next larger size intravenous catheter over the wire to dilate the vein and leave in place; stiff intravenous catheters are more effective. An alternative is to use a small dilator from a pulmonary artery catheter introducer and leave the sheath in place. The wire is removed, and the next larger size wire is inserted (0.025 inch). The catheter (or sheath) is removed, leaving this larger wire within the vein. This process may be repeated with larger catheters and wires until the desired size cannula or sheath is reached. An alternative is to leave progressively larger pulmonary artery introducer sheaths in the vein; both techniques provide a reasonably rapid method of establishing a large-bore intravenous infusion site.
Rapid Infusion Catheters and Introducer Sheaths
Special rapid volume catheters (6F and larger, Arrow International, Reading, Pa.) allow venipuncture with a needle or small intravenous catheter, passage of a guidewire, and then introduction of a dilator and sheath, with fewer steps required (see E-Fig. 10-1).
Intravenous Cutdown
Indications
 Percutaneous cannulation is unsuccessful.
Percutaneous cannulation is unsuccessful.
 Percutaneous cannulation is tenuous.
Percutaneous cannulation is tenuous.
 The catheter in place is inadequate for the planned surgical procedure.
The catheter in place is inadequate for the planned surgical procedure.
The most common sites for insertion are the saphenous vein at the medial malleolus and the brachiocephalic vein at the antecubital fossa. This procedure may require considerable time to perform and has limited utility for emergent access.47
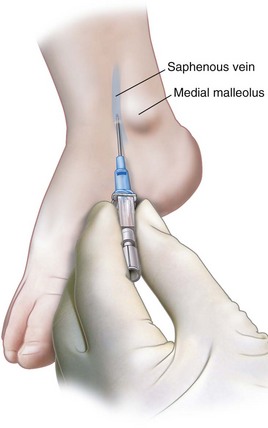
Saphenous Vein Cannulation
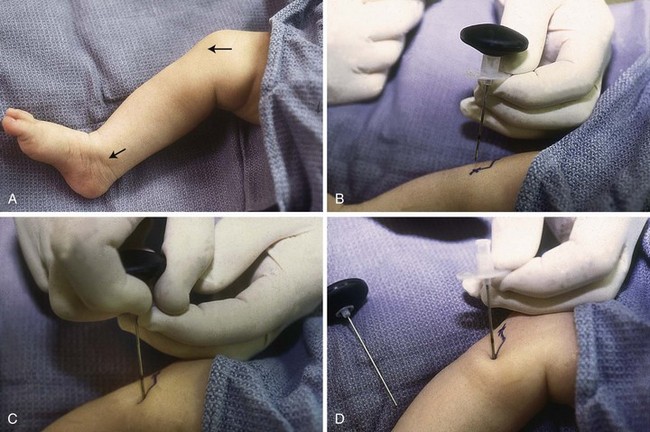
The saphenous vein is often a reliable point for intravenous access in infants and children that may be directly visualized or cannulated with a “blind” technique (Fig. 48-1). It is consistently found lateral to the medial malleolus of the ankle one-half to one finger breadth over the anterior quadrant.
1. Cleanse the area in the standard fashion after a tourniquet is applied to the lower extremity below the knee.
2. The saphenous vein may or may not be palpated, and visualization may not be possible.
3. Enter the skin at a 30-degree angle at the expected site of the saphenous vein at the level of the medial malleolus, with the tip of the needle directed toward the upper two thirds of the calf. If no evidence of venipuncture is seen on insertion, slowly withdraw the needle because the flash of blood may occur while exiting the vein.
4. If unsuccessful on the first attempt, fan medially and then laterally from the same insertion point, slowly advancing and withdrawing the catheter until blood return is obtained.
5. Once a flashback is seen, gently advance the entire unit 2 to 3 mm into the lumen before advancing the catheter off the needle.
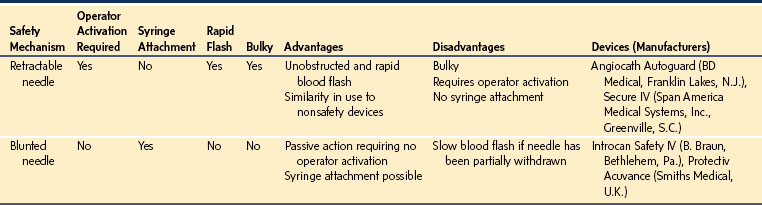
Safety Intravenous Catheters
In the United States, federal law requires that retractable or sheathed needles designed to reduce the potential for needlestick injury are available for use by health care personnel (see Table 48-1).48 A study that compared traditional intravenous catheters to safety devices found that a larger proportion of children younger than 3 years of age required more than one catheter to successfully gain intravenous access. The retractable intravenous catheter was associated with a nearly fourfold greater incidence of splattering and spilling of blood compared with traditional catheters.49 Retractable needles require activation of a button to trigger the safety device; therefore sheathed catheters are regarded as inherently safer because they require no action on the part of the operator to protect the needle tip. Note that the U.S. federal legislation requires that these devices be available but the ultimate decision to use them rests with the physician. Therefore the type of catheter should not be dictated by the hospital but rather by the individuals who place the catheters.
Central Venous Catheterization
Indications
 Provision of a secure means for administration of fluid and blood when major shifts in intravascular volume are anticipated (e.g., multiple trauma, intestinal obstruction, burns)
Provision of a secure means for administration of fluid and blood when major shifts in intravascular volume are anticipated (e.g., multiple trauma, intestinal obstruction, burns)
 Monitoring of cardiac filling pressures
Monitoring of cardiac filling pressures
 Infusion of drugs and fluids that are sclerosing to peripheral veins (e.g., antibiotics, vasopressors, and hyperalimentation fluids)
Infusion of drugs and fluids that are sclerosing to peripheral veins (e.g., antibiotics, vasopressors, and hyperalimentation fluids)
 Measurement of mixed venous acid-base balance, estimation of cardiac output (Fick principle) or measurement of cardiac output (dye dilution)
Measurement of mixed venous acid-base balance, estimation of cardiac output (Fick principle) or measurement of cardiac output (dye dilution)
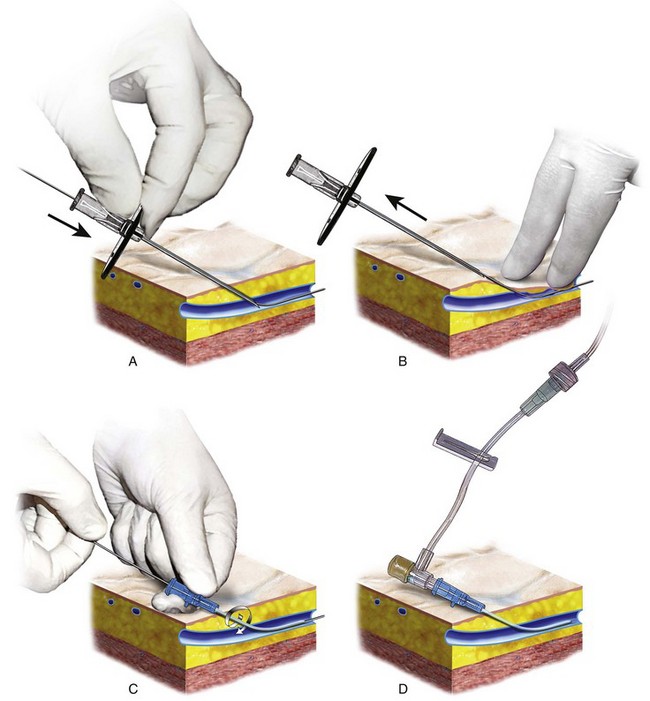
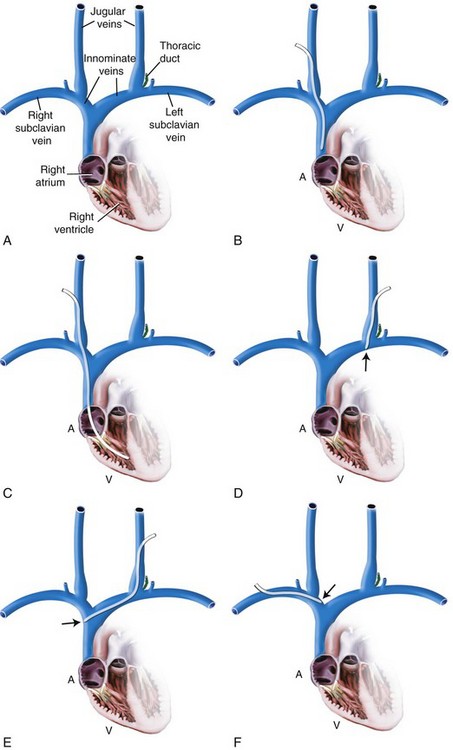
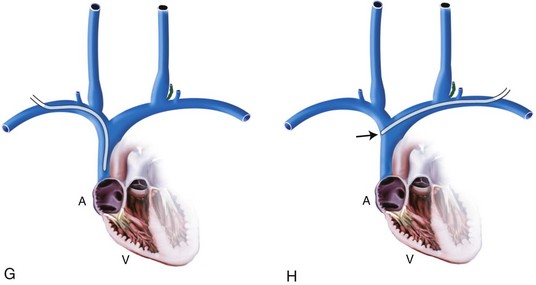
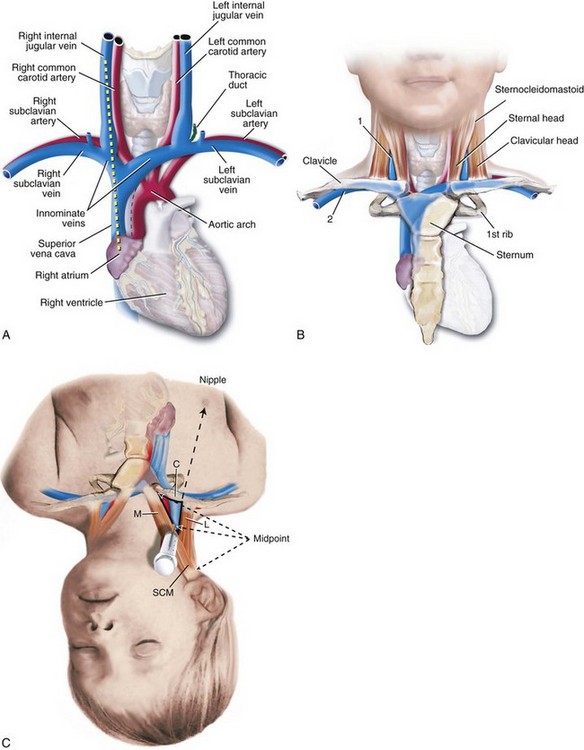
The common sites for central venous cannulation are the external and internal jugular veins, the subclavian and brachiocephalic veins, the femoral vein in infants and children, and the umbilical vein in neonates. Approaches such as the internal jugular and subclavian veins should be used with extreme caution in the presence of a bleeding diathesis as stopping bleeding may be difficult. The percutaneous approach to central venous cannulation is often successful using a modified Seldinger technique (Fig. 48-2).50,51 The advantages of this technique are that it avoids the need for a cutdown, only one venipuncture is made with a thin-walled small-gauge needle, a guidewire directs the catheter within the blood vessel, introducing a large catheter through the small venipuncture site minimizes the chances of significant hematoma formation even after systemic heparinization, and the procedure often can be accomplished when access is required emergently. Whenever a central line is inserted into the heart from above, care must be taken to ensure that the catheter tip is positioned at the junction of the superior vena cava and the right atrium, because positions within the heart have been associated with perforation of large vessels and the myocardium (Fig. 48-3) with triggering of ventricular arrhythmias.52
Ultrasound guidance, pressure waveform analysis, or electrocardiographic guidance may help prevent complications related to central catheter placement.53,54 Ultrasound-guided access assists successful cannulation of the internal jugular vein,53 the infraclavicular axillary vein,54 and the subclavian vein.55,56 A meta-analysis of 18 trials with 1646 participants, including infants, children, and adults, showed a benefit from the use of two-dimensional ultrasound guidance compared with the landmark method. The greatest benefit was for internal jugular vein cannulation rather than subclavian or femoral veins.57 See Chapter 42 and Video 48-1![]() for ultrasound-guided techniques.
for ultrasound-guided techniques.
Complications
Pneumothorax, arrhythmia, hematoma, bleeding, infection, thrombosis, inadvertent arterial puncture, cardiac tamponade, air embolus, thoracic duct injury, and malposition are all possible complications associated with central venous cannulation. Data in adults suggest that the smallest catheter and placement from the left subclavian approach may have the least complication rate; similar studies have not been conducted in children.58 The infection rate reported after 1056 central venous catheters were inserted into 289 children with burn injury varied from 2.0% to 7.3% for catheters in place for 11 or fewer days, but that the rate increased dramatically to 15.8% to 37.5% for catheters left in place for 12 to 14 days.59
Aseptic Technique
Contamination of catheters during insertion may result in catheter colonization or bacterial infection. Evidence suggests that the use of maximum barrier precautions during placement, including the use of sterile gloves, long-sleeved gowns, full-size drape, and a nonsterile mask and cap, decrease the risk of catheter-related infection.34,36,60,61 The efficacy of chlorhexidine versus povidone-iodine for preventing bacteremia remains unclear, and the safety of chlorhexidine in infants and children has not been fully established.62 For older infants and children, chlorhexidine may be safe and effective, but it can cause severe local contact dermatitis in low-birth-weight infants.63,64 In a case-controlled, prospective, active surveillance study in a pediatric intensive care unit (ICU), independent risk factors for central line-associated bloodstream infection were the duration of central venous catheterization in the ICU, nonoperative cardiovascular disease, gastrostomy tube, parenteral nutrition, central line placement in the ICU, and red blood cell transfusion.65
External Jugular Vein Catheterization
1. Place the child in the Trendelenburg position with the head turned 45 degrees away from the side of cannulation.
2. Place a pillow or rolled sheet under the shoulders to extend the head and allow complete access to the neck.
3. Under aseptic conditions, venipuncture and catheter insertion are completed according to the techniques shown in Figure 48-2. A J-wire is usually more useful to circumvent the plexus of veins at the clavicle.66,67
4. Suture or tape appropriately and cover with an occlusive dressing. Many catheters will not pass beyond the clavicle or will pass into the axillary vein; success is generally more often attained on the right side.68,69 If a shorter catheter is used, infusion and pressure monitoring are very dependent on the position of the head.70 Continuous free-flowing infusion is best maintained when the head is turned away from the side of catheter insertion. This vein is particularly valuable in children with difficult peripheral venous access and in an emergent situation that suddenly develops intraoperatively that requires establishment of additional intravenous access.
Internal Jugular Vein Catheterization
Numerous approaches and techniques are used for internal jugular vein cannulation.71–74 A high approach using the apex of a triangle formed by the two bellies of the sternocleidomastoid muscle and the clavicle may be used as a landmark for insertion (Fig. 48-4). With the use of the Seldinger technique, the success rate, even in neonates, approaches 75% on the first attempt and 90% to 95% on the second attempt.50 Cannulation of the right side virtually ensures a central location because the internal jugular vein, the superior vena cava, and the right atrium are in a straight line (see Fig. 48-4). Left-sided cannulation risks injury to the thoracic duct and possible pneumothorax because the apex of the lung is more cephalad on the left. In addition, if the catheter inserted on the left is too short, it is not unusual for the tip to rest against the wall of the superior vena cava, be position dependent, and possibly erode through the wall of the vessel. Figure 48-3 illustrates less desirable sites for catheter tips that may result in perforation. The principal advantage of the high approach is that the most common complication (arterial puncture, approximately 10%) is easily recognized and usually treated uneventfully. In one study, the effect individually and in combination of the simulated Valsalva maneuver (positive inspiratory pressure of 25 mm Hg for 10 seconds), liver compression, and Trendelenburg position to increase the cross-sectional area of the right internal jugular vein was investigated.75 A maximal mean increase in cross-sectional area of the right internal jugular vein was 17.4 ± 16.1% from baseline when all three maneuvers were combined. This effect was most pronounced in children 1 to 6 years of age and was clinically negligible in infants younger than 12 months of age. The effect on ease of catheter placement was not investigated.75 For neonates, a study using skin traction in infants less than 5 kg showed that a technique using tape for skin traction combined with ultrasound guidance increased internal jugular cross-sectional area and decreased the time for catheter placement.76–78
Technique
1. Position the child as for external jugular vein cannulation but with a rolled towel under the center of the back to allow the head to be slightly extended (see Fig. 48-3 and Video 48-1![]() for positioning and the use of ultrasound to guide insertion). The head is turned slightly away from the side of insertion; turning the head too far to the side may result in compression of the vein and moving the vein in closer proximity to the carotid artery.
for positioning and the use of ultrasound to guide insertion). The head is turned slightly away from the side of insertion; turning the head too far to the side may result in compression of the vein and moving the vein in closer proximity to the carotid artery.
2. Locate the apex of a triangle formed by the two bellies of the sternocleidomastoid muscle. This point is usually where the external jugular vein crosses the sternocleidomastoid muscle or the midpoint between the mastoid process and the sternal notch.
3. Palpate the carotid artery. Introduce the needle just lateral to this artery at an angle of 30 degrees to the skin surface. If the internal jugular vein is superficial, a less acute angle may be indicated. While continuously aspirating, advance the needle toward the ipsilateral nipple a distance of no more than 2.5 cm. If no blood is freely obtained, slowly withdraw the needle while maintaining aspiration. The needle can compress the vessel on entry, and it straightens during withdrawal, allowing free aspiration of blood.
4. Once venipuncture is accomplished, carefully remove the syringe and occlude the end of the needle (to prevent entraining air if the child is breathing spontaneously) until a flexible guidewire is inserted (see Fig. 48-2).51 The wire should advance easily. However, if the wire cannot be advanced, the needle has passed out of the vessel lumen or its tip rests against the vessel wall. In this situation, the wire and needle should be withdrawn simultaneously to avoid shearing the wire. If the wire passes without difficulty, then cannulation proceeds as demonstrated in Figures 48-2 and 48-4. Catheter tip location should be confirmed with a radiologic study and repositioned as necessary (see Fig. 48-3).
5. Suture the catheter in place, and protect the area with an occlusive dressing.
Contraindications
 A bleeding diathesis (relative contraindication); in life-threatening emergencies, the benefit may outweigh the risk.
A bleeding diathesis (relative contraindication); in life-threatening emergencies, the benefit may outweigh the risk.
 Raised intracranial pressure (Trendelenburg position and venous occlusion by the catheter may increase intracranial pressure); this is a relative contraindication and ultrasound-guided insertion may provide a great advantage because Trendelenburg position may not be required.
Raised intracranial pressure (Trendelenburg position and venous occlusion by the catheter may increase intracranial pressure); this is a relative contraindication and ultrasound-guided insertion may provide a great advantage because Trendelenburg position may not be required.
Subclavian Vein Catheterization
The subclavian vein is a site frequently used for central vein cannulation.79,80 Success rates of over 80% have been reported even in infants younger than 4 weeks of age.81–83 The advantages include fixed landmarks, ease of securing the line to children for long-term management, and patient comfort. Disadvantages include pneumothorax and hemothorax.84,85 If this site is chosen, we suggest obtaining a chest radiograph after the catheter is inserted and before surgery begins to preclude an unrecognized intraoperative tension pneumothorax. The use of the Seldinger technique (our preference) may reduce the incidence of damage to intrathoracic structures compared with other techniques. As with left-sided internal jugular vein cannulation, if a left subclavian catheter tip rests against the wall of the superior vena cava, it can erode through, resulting in hemothorax or hydrothorax (see Fig. 48-3, H). In a comparison of neutral versus lowered shoulder position in 361 adult patients, neutral position significantly reduced the incidence of misplacement of the catheter tip (ipsilateral internal jugular or brachiocephalic vein) with no difference in the rate of arterial puncture or pneumothorax.86 This maneuver remains to be tested in children.
Technique
1. Prepare and position the child as previously described for external jugular vein puncture.
2. Insert a needle immediately inferior to the clavicle at a point one-half to two-thirds its length from the sternoclavicular junction; while “hugging” the undersurface of the clavicle, the needle is directed toward the suprasternal notch while continuously aspirating.
3. As soon as free blood flow is obtained, proceed as in Figure 48-2. If the Seldinger technique is not used, then first locating the subclavian vein with a small-gauge finder needle is recommended.
4. Suture the catheter in place, and apply an occlusive dressing.
If the child’s ventilation is controlled, the risk of pneumothorax may be decreased by momentarily ceasing ventilation so that the apex of the lung is away from the needle tip. While probing for the subclavian vein, once successful venipuncture has been achieved, maintaining positive end-expiratory pressure reduces the possibility of air embolism. Optimal depths for right subclavian catheterization have been studied in infants 2 to 5 kg using transesophageal echocardiography and found to be 40 to 55 mm for catheter tip placement at the junction of the superior vena cava and the right atrium.87 Contraindications are the same as for internal jugular vein catheterization (see Video 48-1![]() for illustration of technique).
for illustration of technique).
Brachiocephalic Vein Catheterization
The brachiocephalic vein offers the advantage of being far removed from the intrathoracic structures.88 The main disadvantage is that a significant number of catheters introduced at this site do not pass centrally, that is, they are caught in the axilla or pass up the jugular vein (internal or external).89–91 Other disadvantages include significant catheter migration with movement of the arm and possibly an increased incidence of infection. This approach is commonly used by radiologists and pediatric nurses for placement of peripherally inserted central catheters (PICCs), which can be used on a long-term basis.92–94 These catheters often markedly improve patient care and the quality of life for the child because of the reduced need for peripheral venous access and the reduced number of venipunctures for blood testing. The routine use of heparin to prevent catheter thrombosis and occlusion is not supported by published studies, but the data are inadequate to reach a conclusion one way or the other.95
Technique
1. Prepare and drape the arm with aseptic technique.
2. Cannulate the brachiocephalic vein either by using the modified Seldinger technique (special long catheters and wires for this purpose) or by passing a catheter through a needle (Intra Cath, New Delhi, India). If the catheter cannot be threaded once the vein is entered, initiating rapid intravenous fluid administration, cephalad positioning of the arm, and anterior displacement of the shoulder may assist advancement. If percutaneous techniques are not possible, direct venous cutdown may be performed.
Femoral Vein Catheterization
The femoral vein may also be used for access to the central circulation.96 The catheter must pass into the thorax to provide accurate cardiac filling pressure measurements, although there seems to be a reasonable correlation with central filling pressures even when the catheter tip is within the abdomen.97 One advantage of this route is that the vein is large and presents easy access distant from the vital intrathoracic structures (Fig. 48-5). Disadvantages include difficulty in securing the catheter to the child, kinking of the catheter with leg flexion, and problems in maintaining insertion site sterility. Short-term catheterization can provide large-bore venous access for the duration of a procedure with expected large and rapid blood loss if other veins are not accessible. Surprisingly, this site is not associated with a greater incidence of catheter-related sepsis compared with other insertion sites.59,98 This site is not appropriate if disruption of inferior vena cava blood flow is possible (e.g., Wilms tumor resection with invasion of the inferior vena cava, abdominal trauma). The tip of the catheter should be located either low in the atrium or inferior to the level of the diaphragm but superior to the level of the renal veins to reduce the potential for renal vein thrombosis. Use of this technique also has been reported to be safe in infants weighing less than 1000 g with the caution of careful catheter advancement to avoid cardiac perforation.99
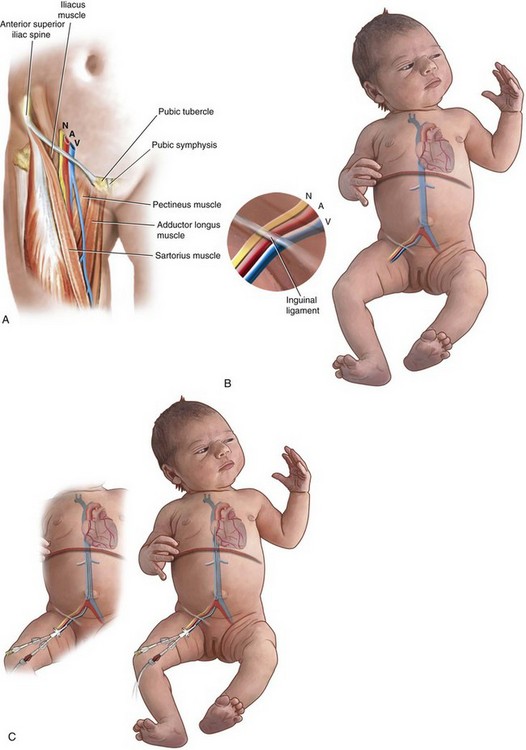
FIGURE 48-5 Insertion of a central venous catheter from the femoral approach. A, The easiest method to remember the anatomy is the mnemonic NAVEL—Nerve, Artery, Vein, Empty space, Leg—such that the vein is always located medial to the artery, and the femoral nerve is located lateral to the artery. B, The femoral artery is palpated just below the inguinal ligament, and a needle is passed just medial to the arterial pulsations. C, The Seldinger technique is utilized (see Fig. 48-2) and the catheter tip is advanced to the desired location (into the low right atrium or below the level of the diaphragm but above the level of the renal veins).
Technique
1. Prepare and drape the groin using an aseptic technique with the legs at 90-degree angles (“frog-leg position”) (see Fig. 48-5, B) A roll under the hips also may provide optimal conditions by slightly elevating the hips.
2. Palpate the femoral artery at a point midway between the pubic tubercle and the anterior superior iliac spine (see Fig. 48-5, A).
3. Using the Seldinger technique, enter the vein at a point just medial to the femoral artery and 1 to 2 cm below the inguinal ligament. A catheter is inserted as in Figure 48-2. As for the brachiocephalic vein, special long catheters and wires are needed to achieve a central location (see Video 48-1![]() ). As with many vascular access methods, ultrasound guidance can be quite useful.100–102
). As with many vascular access methods, ultrasound guidance can be quite useful.100–102
4. Protect the catheter insertion site as previously described (see discussion of internal jugular vein catheterization). If an alternative technique is used (e.g., catheter through the needle), maintain compression of the cannulation site until hemostasis is ensured. The saphenous vein may be cannulated by direct venous cutdown at its junction with the femoral vein if percutaneous techniques are unsuccessful.
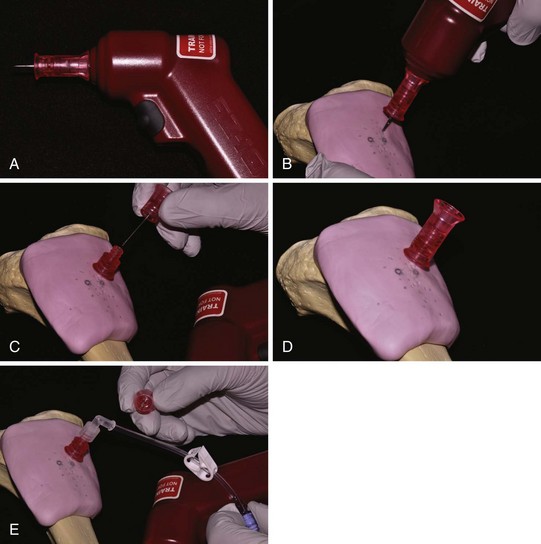
Intraosseous Infusion
The administration of intravenous fluid into the medullary cavity of long bones is a proven method for volume resuscitation in a hypovolemic child and even in teenagers.103–109 This method can effectively deliver drugs to the central circulation as quickly as using peripheral intravenous infusion sites.110 It is a particularly valuable emergency route of drug administration, even in the hands of emergency medical technicians111–113 and as part of emergency department resuscitation of pediatric trauma patients.107 Complications such as cellulitis, abscess, fractures, and osteomyelitis have been reported in less than 1% of cases, and this technique does not appear to affect later growth of the tibia with proper insertion technique.114–116 These complications relate in part to duration of infusion, underlying medical conditions, and aseptic technique. The major difficulties with this technique are due to failure to adhere to proper landmarks117 and bending and clotting of the needle. This technique is used in an emergency situation if several attempts at peripheral or central venous cannulation have failed (suggested “if you cannot achieve reliable access quickly,” which generally means after three attempts or 90 seconds).118,119 Sites for insertion include the upper medial tibia just below the tibial tuberosity, the lower medial tibia just superior to the medial malleolus (to avoid growth plates), the lower femur and the anterior iliac crest. Intraosseous infusions are discontinued once an alternative intravenous infusion site has been secured. This technique has been successfully used for resuscitation of burn victims.120,121 Intraosseous devices should not be used in a fractured leg. For the most recent, complete information, please refer to a review directed to the anesthesiologist caring for pediatric patients.122
Technique
1. Palpate the tibial tuberosity.
2. Locate a point on the medial surface of the tibia at least 1 to 2 cm below and medial to the tibial tuberosity for the site of needle puncture, because the mantle of the tibia is thin at this location (Fig. 48-6, A).
3. Use a special short needle with a stylet to puncture the mantle of the tibia at a 75-degree angle directed toward the feet to avoid the epiphyseal plate (see Fig. 48-6, B and C). A styleted spinal needle also may be used.
4. The appropriate position is readily achieved with the loss of resistance; take care to avoid advancing the needle too far (i.e., out the opposite side or against the opposite mantle of the tibia). The needle is usually quite stable if properly positioned.
5. Attach standard intravenous infusion equipment. Fluid should flow freely without extravasation (see Fig. 48-6, D). A new device for intraosseous access is the EZ-IO (VidaCare, San Antonio, Tex.), which is a handheld battery-powered device that works much like an electric drill (E-Fig. 48-1). This device should be immediately available in all operating rooms and prenatal intensive care units because this is the simplest and easiest means for establishing emergent intraosseous access even in out of hospital venues.123–127
Umbilical Vein Catheterization
Indications
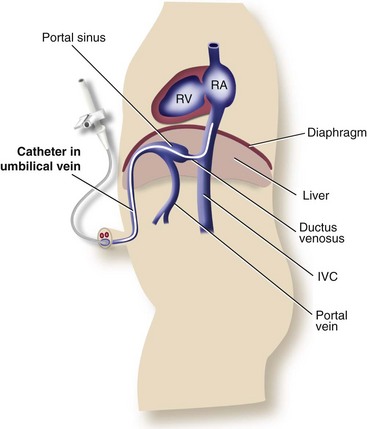
The umbilical vein provides convenient access to the central circulation of a neonate for restoration of blood volume and for administration of glucose and drugs. This procedure is often carried out blindly with later radiographic confirmation of correct position. A large fraction of catheters are initially malpositioned, which if unrecognized, can lead to life-threatening complications.128–132 A change in the configuration of the electrocardiogram (ECG) suggests that a small QRS complex reflects catheter position below the diaphragm; a normal-sized QRS complex with a small P wave was associated with location within the inferior vena cava at the thoracic level; and the appearance of a tall P wave indicated positioning within the right atrium.128 Umbilical vein catheterization also provides a route for the procedure of exchange transfusion and for measuring central venous pressure.
Equipment
 Umbilical artery catheter sizes 3.5 and 5F
Umbilical artery catheter sizes 3.5 and 5F
 Sutures with needle (3-0 silk)
Sutures with needle (3-0 silk)
 Antiseptic solutions (povidone-iodine and alcohol)
Antiseptic solutions (povidone-iodine and alcohol)
 Infusion solution of 10% dextrose in water, with 1 to 2 units of heparin per milliliter at 1 mL/hour
Infusion solution of 10% dextrose in water, with 1 to 2 units of heparin per milliliter at 1 mL/hour
 Calibrated transducer/monitoring system if used for central venous pressure measurement
Calibrated transducer/monitoring system if used for central venous pressure measurement
Technique
1. Prepare and drape the umbilicus with sterile technique; cut the cord approximately 1 cm above the umbilicus. The umbilical vein orifice is more patulous and thin walled than the two umbilical arteries (Fig. 48-7).
2. Holding the catheter filled with heparinized solution 2 cm from the tip, gently introduce it into the vein. In some situations, forceps can aid in directing the catheter. Traction of the umbilical stump caudad may facilitate the catheter’s advancement (see Fig. 48-7). The catheter is passed a distance that approximates the length between the umbilical stump and the right atrium. Blood should freely aspirate into a syringe. Inability to withdraw blood may occur if the tip of the catheter is resting against a vessel wall or if a clot is present within the catheter lumen. It is important that the tip of the catheter be placed in the proper position, that is, at the junction of the inferior vena cava and right atrium. A radiograph confirms proper catheter position. Monitoring changes in the configuration of the ECG during insertion may allow for a more accurate placement within the right atrium but is limited to neonates with a normal tracing.128 At times, the catheter may fail to traverse the ductus venosus and become wedged in the liver. This position is potentially dangerous because portal necrosis and subsequent cirrhosis may result should hyperosmolar or sclerosing solutions be injected (calcium, sodium bicarbonate, 25% to 50% glucose).132,133 A low position might be acceptable for short-term use if it is not possible to pass the catheter centrally, but the distance of insertion should be no more than 3 to 4 cm or just until blood is freely aspirated.
3. Suture the catheter in place, cover the insertion site with antibiotic ointment, and tape it to the abdominal wall. The catheter is then connected to a constant-infusion system and should be removed as soon as the indications for its insertion have passed. Complications appear to relate in part to the duration of insertion.130,132,134
Arterial Cannulation
Umbilical Artery
The umbilical artery in a neonate is a convenient site for monitoring arterial blood pressure, blood gases, and pH. It provides emergency access to an infant’s circulation for restoration of blood volume and administration of glucose and drugs.141–144 Continuous monitoring of arterial O2 saturation is also possible.145
Equipment
The materials used for cannulation are identical to those described for umbilical venous catheterization. Equipment is required for continuous monitoring of blood pressure. End-hole rather than side-hole catheters may have a lower incidence of thrombosis or associated ischemic events.146
Technique
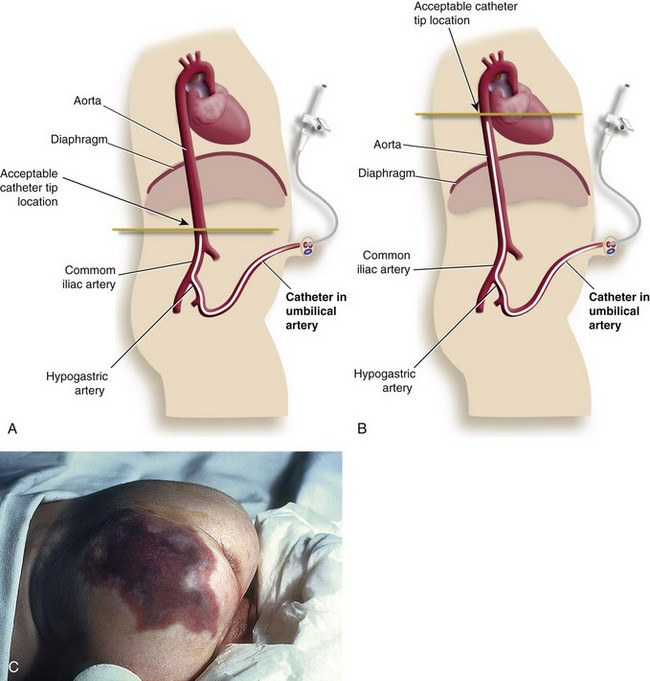
1. Prepare and drape the area with sterile technique; cut the umbilical cord approximately 1 cm above the umbilicus. The two umbilical arteries are identified (Fig. 48-8). The cut vessel ends have thicker walls, are smaller than the vein, and are usually in spasm. The artery is entered in the manner described for umbilical vein catheterization, except that cephalad traction is applied to the umbilical stump (see Fig. 48-6, A) to encourage caudal direction of the catheter. The catheter should course through the umbilical artery into the iliohypogastric artery and then into the descending aorta. Proper positioning of the catheter tip is crucial. If the catheter is advanced too far up the aorta, it may pass through the ductus arteriosus and into the pulmonary artery. If this situation is not recognized, blood pressure and blood gas measurements may be misleading. Care should be taken to ensure the placement of the catheter tip in the descending aorta (at T7 to T9). Early reports suggested that a cephalad position, at or above the level of the diaphragm, is easier to maintain but predisposes infants to increased risk of embolization to renal or mesenteric vessels (see Fig. 48-8, B).147–150 However, positioning just above the bifurcation of the descending aorta, that is, at L3 to L5 (see Fig. 48-8, A) (below the origin of the renal arteries and visceral branches of the aorta) has not been supported by a Cochrane review; a cephalad position is recommended.151 The caudad position is difficult to maintain, and the catheter tip may slip into one of the iliac arteries, resulting in tissue ischemia (see Fig. 48-8, C).
2. Confirm the position radiographically. Once the catheter is properly positioned, the system is connected to a constant-infusion pump and heparinized fluids (10% dextrose in water or normal saline) are infused. Suture and tape the catheter and apply antibiotic ointment as for umbilical vein catheters. A Cochrane review of the use of heparin suggested that low-dose heparinization of the infusate (0.25 unit/mL) has been shown to reduce the likelihood of catheter occlusion compared with intermittent flushing with heparinized solutions.152
Complications
Using the umbilical artery as a source for blood pressure monitoring and blood gas analysis only and reserving alternative sites for glucose and drug administration may minimize complications. Changes in cerebral blood flow are associated with intraventricular hemorrhage and have been documented to occur with umbilical artery blood sampling; fewer changes in cerebral blood flow occur with low-positioned catheters.153 The incidence of documented intraventricular hemorrhage appears to have a stronger relation with age than with catheter position and is not associated with the use of low-dose heparin.152,154 Other complications are as follows:
 Accidental disconnection of stopcocks and catheters can lead to potentially dangerous exsanguination.
Accidental disconnection of stopcocks and catheters can lead to potentially dangerous exsanguination.
 Blood clots may embolize retrograde or, more likely, distally, leading to ischemia or infarction of the infant’s gut, kidneys, or lower limbs (see Fig. 48-8, C ).155
Blood clots may embolize retrograde or, more likely, distally, leading to ischemia or infarction of the infant’s gut, kidneys, or lower limbs (see Fig. 48-8, C ).155
 Vascular spasm is usually transitory and may be resolved by withdrawal of the catheter. Several cases of flaccid paraplegia have been reported resulting from spasm or embolic phenomena.156
Vascular spasm is usually transitory and may be resolved by withdrawal of the catheter. Several cases of flaccid paraplegia have been reported resulting from spasm or embolic phenomena.156
 The infant is always at risk for sepsis; therefore clear indications for the insertion of this catheter are mandatory. The catheter should be removed at the earliest possible time. A Cochrane review failed to establish a role for prophylactic antibiotics in reducing catheter-related infections.157
The infant is always at risk for sepsis; therefore clear indications for the insertion of this catheter are mandatory. The catheter should be removed at the earliest possible time. A Cochrane review failed to establish a role for prophylactic antibiotics in reducing catheter-related infections.157
 Hypertension as a result of renal artery emboli may cause ischemia and infarction of the kidney.150,158
Hypertension as a result of renal artery emboli may cause ischemia and infarction of the kidney.150,158
Radial Artery
Radial artery cannulation is a reasonable alternative to umbilical artery cannulation in a neonate and is the primary site of arterial cannulation in infants and children in most pediatric institutions. Percutaneous radial artery cannulation is widely practiced, with minimal morbidity.130,159–164 Failure to cannulate the artery percutaneously may be followed successfully by direct arterial cutdown. Of children with Down syndrome (trisomy 21), 16% to 19% have abnormal radial vessels (both size and location), which can make arterial cannulation particularly difficult; some children with Down syndrome have a single median artery.166,167 The ulnar artery also has been used as an alternative site for arterial catheterization when attempts at insertion in other locations have been unsuccessful; to ensure adequate perfusion of the hand, this site should not be used if previous attempts at cannulation of the ipsilateral radial artery had been attempted.165
Technique
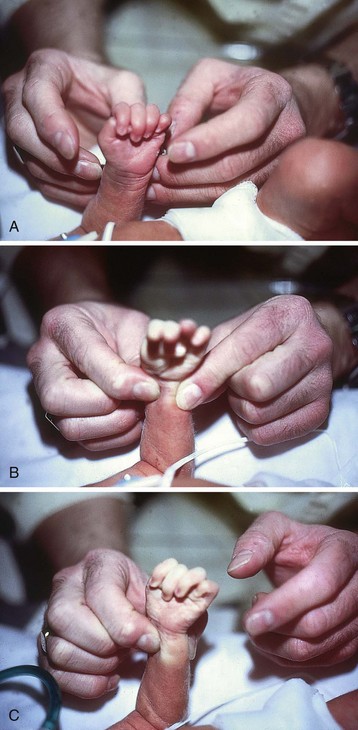
1. Confirm the adequacy of ulnar artery collateral flow by the modified Allen test (Fig. 48-9, A). The color of the hand is noted. The hand is passively clenched, and the radial and ulnar arteries are simultaneously compressed at the wrist (see Fig. 48-9, B). The ulnar artery is then released, and flushing (reperfusion) of the blanched hand is noted (see Fig. 48-9, C ). If the entire hand is well perfused while the radial artery remains occluded, indicating adequate collateral flow, catheterization of the radial artery is performed. Note that the sensitivity of the Allen test is approximately 73%, with a specificity of 97%.168
2. Secure the hand using an arm board with slight extension of the wrist to avoid excessive median nerve stretching. The fingertips should be left exposed when the hand is taped down so that any peripheral ischemic changes from spasm, clot, or air can be observed.
3. Observe the course of the radial artery in a neonate with the aid of a fiberoptic light source directed toward the lateral side or dorsal aspect of the wrist. Use of a Doppler device may also be of great value.169,170
4. Use a 20-gauge needle to make a small skin puncture over the maximal pulsation of the radial artery, usually at the second proximal wrist crease. This step eases passage of the cannula by reducing resistance offered by the skin and prevents a burr from forming on the catheter tip as it passes through the dermis. A method to avoid accidental puncture of the artery is to pull the overlying skin laterally to make the skin nick.
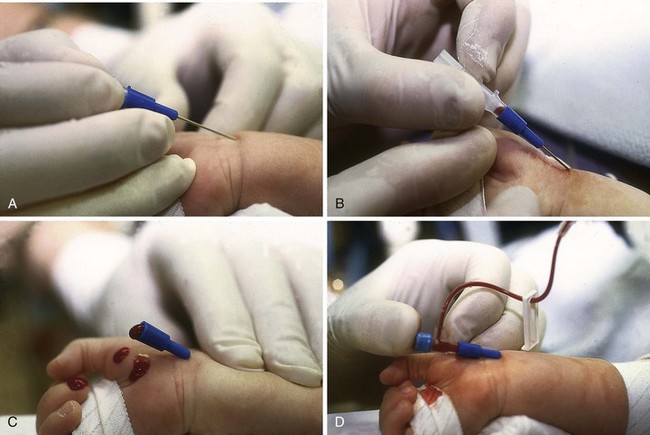
5. Perform cannulation with a 24- or 22-gauge catheter either on direct entry of the artery at an angle of 15 to 20 degrees or on withdrawing the cannula after transfixion of the artery (Fig. 48-10, A to C ). A wire (0.018 inch) may be used as an aid to advance 22-gauge and nontapered 24-gauge catheters.
6. Attach the catheter firmly to a T-connector to permit continuous infusion of isotonic saline (1 unit/mL) at the rate of 1 to 2 mL/hr via a constant-infusion pump (see Fig. 48-10, D). The catheter is securely taped in place. A pressure transducer is connected to allow continuous arterial pressure monitoring. To ensure accurate blood pressure measurement, it is essential that the transducer be calibrated to the neonate’s or child’s heart level, that all air bubbles be removed from the system, and that no more than 3 feet of tubing be used between the neonate or child and the transducer to minimize artifacts caused by the monitoring tubing.171
7. Obtain blood samples by clamping off the distal end of the T-connector, cleaning the injection port of the T-connector with povidone-iodine, introducing a 22-gauge needle, and withdrawing 1 mL of blood. A sample of blood is obtained by heparinized syringe, with minimal blood loss and minimal manipulation of the system.159,172 An alternative is the use of a 3-mL syringe on a three-way stopcock: aspirate 2 to 3 mL, clamp the system, and then take the sample of blood from the T-connector as just described. After sampling, the clamp is released, the aspirated blood is readministered, and continuous infusion is resumed or flush is run into the 3-mL syringe and then the system is gently manually flushed intermittently with the syringe but the flush syringe is changed just once per 24 hours. This method of sampling maintains a closed system with reduced potential for sources of infection. Bolus flushes are avoided, which is an important consideration because bolus flushing has been associated with retrograde blood flow to the brain. Disastrous results may occur if an air bubble or blood clot should accompany a bolus flush.173–177 All arterial lines must be clearly identified (red tape) to avoid accidental infusion of hypertonic solutions and sclerosing medications.
Complications
 Infection at the site of the catheter insertion, with possible septicemia.
Infection at the site of the catheter insertion, with possible septicemia.
 Arterial thrombus formation. This depends on the size of catheter inserted, the material of which it is constructed, the technique of insertion, and the duration of cannulation.
Arterial thrombus formation. This depends on the size of catheter inserted, the material of which it is constructed, the technique of insertion, and the duration of cannulation.
 Emboli. A blood clot or air may embolize to the digits, resulting in arteriolar spasm or more serious ischemic necrosis.
Emboli. A blood clot or air may embolize to the digits, resulting in arteriolar spasm or more serious ischemic necrosis.
 Disconnection of the catheter from the infusion system. Blood loss may be life-threatening, especially in an infant.
Disconnection of the catheter from the infusion system. Blood loss may be life-threatening, especially in an infant.
 Ischemia. The radial artery cannula should be withdrawn if ischemic changes develop.
Ischemia. The radial artery cannula should be withdrawn if ischemic changes develop.
 Vasospasm. Usually transient but requires careful observation.
Vasospasm. Usually transient but requires careful observation.
The method just described is the traditional percutaneous radial artery cannulation at the ventral aspect of the wrist. The radial artery on the dorsal aspect of the wrist within the anatomic snuff box may be used as an alternative site.178 Once an attempt at cannulation of the radial artery is made, the ipsilateral ulnar artery should not be instrumented to ensure adequate perfusion of the entire hand. Strict indications for inserting radial artery catheters are necessary, and their removal must be considered at the earliest possible time.147–150
Temporal Artery
When the radial artery has been previously cannulated or is inaccessible, the temporal artery may be used.179 Cerebral infarction has been described as a complication of this technique. It appears to be related to retrograde embolization of air or a blood clot.180
Femoral Artery
Femoral catheterization in infants and children includes a greater risk of vascular injury or thrombosis resulting in ischemia181 and is not recommended if other peripheral sites are available. In situations in which peripheral arterial cannulation is impossible (e.g., in burned patients or children with poor peripheral perfusion), the femoral artery should be used rather than not having any invasive arterial monitoring; the remote possibility of a complication must be balanced versus a greater likelihood of life-threatening complications owing to less than ideal monitoring.182
Technique
1. Locate the femoral artery by palpation at the groin; this can be confirmed with ultrasonic guidance. Anatomically, it is situated midway between the anterior superior iliac spine and the pubic tubercle.
2. After sterile preparation of the skin, insert a catheter of appropriate size into the femoral artery using the Seldinger technique. The artery is entered at the point of maximal pulsation, approximately 1 cm below the line joining the anterior superior iliac spine and the pubic tubercle.
3. After cannulation, connect the catheter to a continuous-flow system and pressure transducer. The catheter is sutured in place, the insertion site is covered, and an occlusive dressing is applied. The likelihood of fecal and urinary contamination makes this last step particularly important.
Complications
 Emboli of clot and air, leading to ischemic necrosis of the lower limb
Emboli of clot and air, leading to ischemic necrosis of the lower limb
 Poor arterial puncture technique, leading to osteoarthritis of the hip joint; severe trauma to the femoral artery has resulted in gangrene of the lower limb, retroperitoneal hemorrhage, and arteriovenous fistula formation.183–185 A late complication can be partial arrest of bone growth likely as a result of thrombus formation.186
Poor arterial puncture technique, leading to osteoarthritis of the hip joint; severe trauma to the femoral artery has resulted in gangrene of the lower limb, retroperitoneal hemorrhage, and arteriovenous fistula formation.183–185 A late complication can be partial arrest of bone growth likely as a result of thrombus formation.186
 Vasospasm. Usually transient but requires careful observation.
Vasospasm. Usually transient but requires careful observation.
1 Smith DW, Sappenfield RS, Fink WJ. Use of the plastic intravenous catheter for multiple and massive transfusions and prolonged intravenous fluid therapy. Surg Gynecol Obstet. 1952;95:775–777.
2 Anonymous, Policy and guidelines for prevention and management of human immunodeficiency virus and hepatitis B virus infection in the nursing education community. American Association of Colleges of Nursing. J Prof Nurs. 1997;13:325–328.
3 Moore S, Goodwin H, Grossberg R, Toltzis P. Compliance with universal precautions among pediatric residents. Arch Pediatr Adolesc Med. 1998;152:554–557.
4 Tait AR, Tuttle DB. Preventing perioperative transmission of infection: a survey of anesthesiology practice. Anesth Analg. 1995;80:764–769.
5 Chalmers C, Straub M. Standard principles for preventing and controlling infection. Nurs Stand. 2006;20:57–65.
6 Beekmann SE, Henderson DK. Protection of healthcare workers from bloodborne pathogens. Curr Opin Infect Dis. 2005;18:331–336.
7 Morray JP. Anesthesia-related cardiac arrest in children: an update. Anesthesiol Clin North Am. 2002;20:1–28.
8 Mason LJ. An update on the etiology and prevention of anesthesia-related cardiac arrest in children. Paediatr Anaesth. 2004;14:412–416.
9 Tobias JD, Johnson JO. Measurement of central venous pressure from a peripheral vein in infants and children. Pediatr Emerg Care. 2003;19:428–430.
10 Cox P, Johnson JO, Tobias JD. Measurement of central venous pressure from a peripheral intravenous catheter in the lower extremity. South Med J. 2005;98:698–702.
11 Tobias JD. Measurement of central venous pressure from a peripheral intravenous catheter in the prone position during spinal surgery. South Med J. 2009;102:256–259.
12 Tobias JD, Johnson JO. Measurement of central venous pressure from a peripheral vein in infants and children. Pediatr Emerg Care. 2003;19:428–430.
13 Anter AM, Bondok RS. Peripheral venous pressure is an alternative to central venous pressure in paediatric surgery patients. Acta Anaesthesiol Scand. 2004;48:1101–1104.
14 Tobias JD. Measurement of central venous pressure from a peripheral intravenous catheter in the prone position during spinal surgery. South Med J. 2009;102:256–259.
15 Baty L, Russo P, Tobias JD. Measurement of central venous pressure from a peripheral intravenous catheter following cardiopulmonary bypass in infants and children with congenital heart disease. J Intensive Care Med. 2008;23:136–142.
16 Amoozgar H, Behniafard N, Borzoee M, Ajami GH. Correlation between peripheral and central venous pressures in children with congenital heart disease. Pediatr Cardiol. 2008;29:281–284.
17 Sahin A, Salman MA, Salman AE, Aypar U. Effect of body temperature on peripheral venous pressure measurements and its agreement with central venous pressure in neurosurgical patients. J Neurosurg Anesthesiol. 2005;17:91–96.
18 Atalay H, Erbay H, Tomatir E, Serin S, Oner O. The use of transillumination for peripheral venous access in paediatric anaesthesia. Eur J Anaesthesiol. 2005;22:317–318.
19 Sandhu NP, Sidhu DS. Mid-arm approach to basilic and cephalic vein cannulation using ultrasound guidance. Br J Anaesth. 2004;93:292–294.
20 Keyes LE, Frazee BW, Snoey ER, Simon BC, Christy D. Ultrasound-guided brachial and basilic vein cannulation in emergency department patients with difficult intravenous access. Ann Emerg Med. 1999;34:711–714.
21 Perry AM, Caviness AC, Hsu DC. Efficacy of a near-infrared light device in pediatric intravenous cannulation: a randomized controlled trial. Pediatr Emerg Care. 2011;27:5–10.
22 Rogers TL, Ostrow CL. The use of EMLA cream to decrease venipuncture pain in children. J Pediatr Nurs. 2004;19:33–39.
23 Sethna NF, Verghese ST, Hannallah RS, et al. A randomized controlled trial to evaluate S-Caine patch for reducing pain associated with vascular access in children. Anesthesiology. 2005;102:403–408.
24 Schultz AA, Strout TD, Jordan P, Worthing B. Safety, tolerability, and efficacy of iontophoresis with lidocaine for dermal anesthesia in ED pediatric patients. J Emerg Nurs. 2002;28:289–296.
25 Kim MK, Kini NM, Troshynski TJ, Hennes HM. A randomized clinical trial of dermal anesthesia by iontophoresis for peripheral intravenous catheter placement in children. Ann Emerg Med. 1999;33:395–399.
26 Koh JL, Harrison D, Myers R, et al. A randomized, double-blind comparison study of EMLA and ELA-Max for topical anesthesia in children undergoing intravenous insertion. Paediatr Anaesth. 2004;14:977–982.
27 Luhmann J, Hurt S, Shootman M, Kennedy R. A comparison of buffered lidocaine versus ELA-Max before peripheral intravenous catheter insertions in children. Pediatrics. 2004;113:e217–e220.
28 Eichenfield LF, Funk A, Fallon-Friedlander S, Cunningham BB. A clinical study to evaluate the efficacy of ELA-Max (4% liposomal lidocaine) as compared with eutectic mixture of local anesthetics cream for pain reduction of venipuncture in children. Pediatrics. 2002;109:1093–1099.
29 O’Brien L, Taddio A, Lyszkiewicz DA, Koren G. A critical review of the topical local anesthetic amethocaine (Ametop) for pediatric pain. Paediatr Drugs. 2005;7:41–54.
30 Ballantyne M, McNair C, Ung E, Gibbins S, Stevens B. A randomized controlled trial evaluating the efficacy of tetracaine gel for pain relief from peripherally inserted central catheters in infants. Adv Neonatal Care. 2003;3:297–307.
31 Arrowsmith J, Campbell C. A comparison of local anaesthetics for venepuncture. Arch Dis Child. 2000;82:309–310.
32 Lovich MA, Doles J, Peterfreund RA. The impact of carrier flow rate and infusion set dead-volume on the dynamics of intravenous drug delivery. Anesth Analg. 2005;100:1048–1055.
33 Rosen KR, Rosen DA. Comparative flow rates for small bore peripheral intravenous catheters. Pediatr Emerg Care. 1986;2:153–156.
34 Kline AM. Pediatric catheter-related bloodstream infections: latest strategies to decrease risk. AACN Clin Issues. 2005;16:185–198.
35 Couzigou C, Lamory J, Salmon-Ceron D, Figard J, Vidal-Trecan GM. Short peripheral venous catheters: effect of evidence-based guidelines on insertion, maintenance and outcomes in a university hospital. J Hosp Infect. 2005;59:197–204.
36 O’Grady NP, Alexander M, Dellinger EP, et al. Guidelines for the prevention of intravascular catheter-related infections. Infect Control Hosp Epidemiol. 2002;23:759–769.
37 Shimandle RB, Johnson D, Baker M, et al. Safety of peripheral intravenous catheters in children. Infect Control Hosp Epidemiol. 1999;20:736–740.
38 Smith AB, Wilkinson-Faulk D. Factors affecting the life span of peripheral intravenous lines in hospitalized infants. Pediatr Nurs. 1994;20:543–547.
39 Rickard CM, McCann D, Munnings J, McGrail MR. Routine resite of peripheral intravenous devices every 3 days did not reduce complications compared with clinically indicated resite: a randomised controlled trial. BMC Med. 2010;8:53.
40 Yosowitz P, Ekland DA, Shaw RC, Parsons RW. Peripheral intravenous infiltration necrosis. Ann Surg. 1975;182:553–556.
41 Phelps SJ, Helms RA. Risk factors affecting infiltration of peripheral venous lines in infants. J Pediatr. 1987;111:384–389.
42 Shah PS, Ng E, Sinha AK. Heparin for prolonging peripheral intravenous catheter use in neonates. Cochrane Database Syst Rev. 2002. CD002774
43 Hadimioglu N, Ertug Z, Yegin A, et al. Correlation of peripheral venous pressure and central venous pressure in kidney recipients. Transplant Proc. 2006;38:440–442.
44 Sahin A, Salman MA, Salman AE, Aypar U. Effect of catheter site on the agreement of peripheral and central venous pressure measurements in neurosurgical patients. J Clin Anesth. 2005;17:348–352.
45 Sahin A, Salman MA, Salman AE, Aypar U. Effect of body temperature on peripheral venous pressure measurements and its agreement with central venous pressure in neurosurgical patients. J Neurosurg Anesthesiol. 2005;17:91–96.
46 Charalambous C, Barker TA, Zipitis CS, et al. Comparison of peripheral and central venous pressures in critically Ill patients. Anaesth Intensive Care. 2003;31:34–39.
47 Iserson KV, Criss EA. Pediatric venous cutdowns: utility in emergency situations. Pediatr Emerg Care. 1986;2:231–234.
48 Occupational exposure to bloodborne pathogens; needlestick and other sharps injuries: final rule. Fed Reg. 2002;66:5317–5325. 29 CFR Part 1910, Docket H370A
49 Coté CJ, Roth AG, Wheeler M, et al. Traditional versus new needle retractable i.v. catheters in children: are they really safer, and whom are they protecting? Anesth Analg. 2003;96:387–391.
50 Coté CJ, Jobes DR, Schwartz AJ, Ellison N. Two approaches to cannulation of a child’s internal jugular vein. Anesthesiology. 1979;50:371–373.
51 Seldinger SI. Catheter replacement of the needle in percutaneous arteriography. Acta Radiol. 1953;39:368–376.
52 Jay AW, Kehler CH. Heart perforation by central venous catheters. Can J Anaesth. 1987;34:333–335.
53 Liberman L, Hordof AJ, Hsu DT, Pass RH. Ultrasound-assisted cannulation of the right internal jugular vein during electrophysiologic studies in children. J Interv Card Electrophysiol. 2001;5:177–179.
54 Sharma A, Bodenham AR, Mallick A. Ultrasound-guided infraclavicular axillary vein cannulation for central venous access. Br J Anaesth. 2004;93:188–192.
55 Rhondali O, Attof R, Combet S, Chassard D, de Queiroz SM. Ultrasound-guided subclavian vein cannulation in infants: supraclavicular approach. Paediatr Anaesth. 2011.
56 Breschan C, Platzer M, Jost R, et al. Consecutive, prospective case series of a new method for ultrasound-guided supraclavicular approach to the brachiocephalic vein in children. Br J Anaesth. 2011;106:732–737.
57 Hind D, Calvert N, McWilliams R, et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ. 2003;327:361.
58 Onders RP, Shenk RR, Stellato TA. Long-term central venous catheters: size and location do matter. Am J Surg. 2006;191:396–399.
59 Sheridan RL, Weber JM. Mechanical and infectious complications of central venous cannulation in children: lessons learned from a 10-year experience placing over 1000 catheters. J Burn Care Res. 2006;27:713–718.
60 Raad II, Hohn DC, Gilbreath BJ, et al. Prevention of central venous catheter-related infections by using maximal sterile barrier precautions during insertion. Infect Control Hosp Epidemiol. 1994;15:231–238.
61 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control. 2011;39:640–646.
62 Carson SM. Chlorhexidine versus povidone-iodine for central venous catheter site care in children. J Pediatr Nurs. 2004;19:74–80.
63 Garland JS, Alex CP, Mueller CD, et al. A randomized trial comparing povidone-iodine to a chlorhexidine gluconate-impregnated dressing for prevention of central venous catheter infections in neonates. Pediatrics. 2001;107:1431–1436.
64 Garland JS, Buck RK, Maloney P, et al. Comparison of 10% povidone-iodine and 0.5% chlorhexidine gluconate for the prevention of peripheral intravenous catheter colonization in neonates: a prospective trial. Pediatr Infect Dis J. 1995;14:510–516.
65 Wylie MC, Graham DA, Potter-Bynoe G, et al. Risk factors for central line-associated bloodstream infection in pediatric intensive care units. Infect Control Hosp Epidemiol. 2010;31:1049–1056.
66 Blitt CD, Wright WA, Petty WC, Webster TA. Central venous catheterization via the external jugular vein: a technique employing the J-WIRE. JAMA. 1974;229:817–818.
67 Schwartz AJ, Jobes DR, Levy WJ, Palermo L, Ellison N. Intrathoracic vascular catheterization via the external jugular vein. Anesthesiology. 1982;56:400–402.
68 Belani KG, Buckley JJ, Gordon JR, Castaneda W. Percutaneous cervical central venous line placement: a comparison of the internal and external jugular vein routes. Anesth Analg. 1980;59:40–44.
69 Blitt CD, Carlson GL, Wright WA, Otto CW. J-wire versus straight wire for central venous system cannulation via the external jugular vein. Anesth Analg. 1982;61:536–537.
70 Stoelting RK. Evaluation of external jugular venous pressure as a reflection of right atrial pressure. Anesthesiology. 1973;38:291–294.
71 Boulanger M, Delva E, Mailleet, Paiement B. [A new way of access into the internal jugular vein]. [French]. Can Anaesth Soc J. 1976;23:609–615.
72 Civetta JM, Gabel JC, Gemer M. Internal-jugular-vein puncture with a margin of safety. Anesthesiology. 1972;36:622–623.
73 Hayashi Y, Maruyama K, Takaki O, et al. Optimal placement of CVP catheter in paediatric cardiac patients. Can J Anaesth. 1995;42:479–482.
74 Rao TL, Wong AY, Salem MR. A new approach to percutaneous catheterization of the internal jugular vein. Anesthesiology. 1977;46:362–364.
75 Verghese ST, Nath A, Zenger D, et al. The effects of the simulated Valsalva maneuver, liver compression, and/or Trendelenburg position on the cross-sectional area of the internal jugular vein in infants and young children. Anesth Analg. 2002;94:250–254.
76 Morita M, Sasano H, Azami T, et al. A novel skin-traction method is effective for real-time ultrasound-guided internal jugular vein catheterization in infants and neonates weighing less than 5 kilograms. Anesth Analg. 2009;109:754–759.
77 Morita M, Sasano H, Azami T, Sasano N, Katsuya H. The skin-traction method increases the cross-sectional area of the internal jugular vein by increasing its anteroposterior diameter. J Anesth. 2007;21:467–471.
78 Sasano H, Morita M, Azami T, et al. Skin-traction method prevents the collapse of the internal jugular vein caused by an ultrasound probe in real-time ultrasound-assisted guidance. J Anesth. 2009;23:41–45.
79 Casado-Flores J, Valdivielso-Serna A, Perez-Jurado L, et al. Subclavian vein catheterization in critically ill children: analysis of 322 cannulations. Intensive Care Med. 1991;17:350–354.
80 Cogliati AA, Dell’Utri D, Picardi A, et al. Central venous catheterization in pediatric patients affected by hematological malignancies. Haematologica. 1995;80:448–450.
81 Kron IL, Rheuban K, Miller ED, Lake CL, Nolan SP. Subclavian vein catheterization for central line placement in children under 2 years of age. Am Surg. 1985;51:272–273.
82 Yao ML, Chiu PC, Hsieh KS, et al. Subclavian central venous catheterization in infants with body weight less than 10 kg. Acta Paediatr Taiwan. 2004;45:324–327.
83 Finck C, Smith S, Jackson R, Wagner C. Percutaneous subclavian central venous catheterization in children younger than one year of age. Am Surg. 2002;68:401–404.
84 Citak A, Karabocuoglu M, Ucsel R, Uzel N. Central venous catheters in pediatric patients: subclavian venous approach as the first choice. Pediatr Int. 2002;44:83–86.
85 Johnson EM, Saltzman DA, Suh G, Dahms RA, Leonard AS. Complications and risks of central venous catheter placement in children. Surgery. 1998;124:911–916.
86 Kang M, Ryu HG, Son IS, Bahk JH. Influence of shoulder position on central venous catheter tip location during infraclavicular subclavian approach. Br J Anaesth. 2011;106:344–347.
87 Kim JH, Kim CS, Bahk JH, et al. The optimal depth of central venous catheter for infants less than 5 kg. Anesth Analg. 2005;101:1301–1303.
88 Klein MD, Rudd M. Successful central venous catheter placement from peripheral subcutaneous veins in children. Anesthesiology. 1980;52:447–448.
89 Kuramoto T, Sakabe T. Comparison of success in jugular versus basilic vein technics for central venous pressure catheter positioning. Anesth Analg. 1975;54:696–697.
90 Webre DR, Arens JF. Use of cephalic and basilic veins for introduction of central venous catheters. Anesthesiology. 1973;38:389–392.
91 Chaturvedi A, Bithal PK, Dash H, Chauhan RS, Mohanty B. Catheter malplacement during central venous cannulation through arm veins in pediatric patients. J Neurosurg Anesthesiol. 2003;15:170–175.
92 Donaldson JS, Morello FP, Junewick JJ, O’Donovan JC, Lim-Dunham J. Peripherally inserted central venous catheters: US-guided vascular access in pediatric patients. Radiology. 1995;197:542–544.
93 Stovroff MC, Totten M, Glick PL. PIC lines save money and hasten discharge in the care of children with ruptured appendicitis. J Pediatr Surg. 1994;29:245–247.
94 Crowley JJ. Vascular access. Tech Vasc Interv Radiol. 2003;6:176–181.
95 Shah P, Shah V. Continuous heparin infusion to prevent thrombosis and catheter occlusion in neonates with peripherally placed percutaneous central venous catheters. Cochrane Database Syst Rev. 2005. CD002772
96 Celermajer DS, Robinson JT, Taylor JF. Vascular access in previously catheterized children and adolescents: a prospective study of 131 consecutive cases. Br Heart J. 1993;70:554–557.
97 Fernandez EG, Green TP, Sweeney M. Low inferior vena caval catheters for hemodynamic and pulmonary function monitoring in pediatric critical care patients. Pediatr Crit Care Med. 2004;5:14–18.
98 Casado-Flores J, Barja J, Martino R, Serrano A, Valdivielso A. Complications of central venous catheterization in critically ill children. Pediatr Crit Care Med. 2001;2:57–62.
99 Chen KB. Clinical experience of percutaneous femoral venous catheterization in critically ill preterm infants less than 1,000 grams. Anesthesiology. 2001;95:637–639.
100 Suk EH, Lee KY, Kweon TD, Jang YH, Bai SJ. Ultrasonographic evaluation of the femoral vein in anaesthetised infants and young children. Anaesthesia. 2010;65:895–898.
101 Pirotte T. Ultrasound-guided vascular access in adults and children: beyond the internal jugular vein puncture. Acta Anaesthesiol Belg. 2008;59:157–166.
102 Aouad MT, Kanazi GE, Abdallah FW, et al. Femoral vein cannulation performed by residents: a comparison between ultrasound-guided and landmark technique in infants and children undergoing cardiac surgery. Anesth Analg. 2010;111:724–728.
103 Cilley RE. Intraosseous infusion in infants and children. Semin Pediatr Surg. 1992;1:202–207.
104 Driggers DA, Johnson R, Steiner JF, et al. Emergency resuscitation in children: the role of intraosseous infusion. Postgrad Med. 1991;89:129–132.
105 Evans RJ, McCabe M, Thomas R. Intraosseous infusion. Br J Hosp Med. 1994;51:161–164.
106 Guy J, Haley K, Zuspan SJ. Use of intraosseous infusion in the pediatric trauma patient. J Pediatr Surg. 1993;28:158–161.
107 Smith R, Davis N, Bouamra O, Lecky F. The utilisation of intraosseous infusion in the resuscitation of paediatric major trauma patients. Injury. 2005;36:1034–1038.
108 Haas NA. Clinical review: vascular access for fluid infusion in children. Crit Care. 2004;8:478–484.
109 DeBoer S, Seaver M, Morissette C. Intraosseous infusion: not just for kids anymore. Emerg Med Serv. 2005;34:54. 56-4, 63
110 Bilello JF, O’Hair KC, Kirby WC, Moore JW. Intraosseous infusion of dobutamine and isoproterenol. Am J Dis Child. 1991;145:165–167.
111 Glaeser PW, Hellmich TR, Szewczuga D, Losek JD, Smith DS. Five-year experience in prehospital intraosseous infusions in children and adults. Ann Emerg Med. 1993;22:1119–1124.
112 Losek JD, Szewczuga D, Glaeser PW. Improved prehospital pediatric ALS care after an EMT-paramedic clinical training course. Am J Emerg Med. 1994;12:429–432.
113 Seigler RS, Tecklenburg FW, Shealy R. Prehospital intraosseous infusion by emergency medical services personnel: a prospective study. Pediatrics. 1989;84:173–177.
114 Fiser RT, Walker WM, Seibert JJ, McCarthy R, Fiser DH. Tibial length following intraosseous infusion: a prospective, radiographic analysis. Pediatr Emerg Care. 1997;13:186–188.
115 Claudet I, Baunin C, Laporte-Turpin E, et al. Long-term effects on tibial growth after intraosseous infusion: a prospective, radiographic analysis. Pediatr Emerg Care. 2003;19:397–401.
116 Bowley DM, Loveland J, Pitcher GJ. Tibial fracture as a complication of intraosseous infusion during pediatric resuscitation. J Trauma. 2003;55:786–787.
117 Boon JM, Gorry DL, Meiring JH. Finding an ideal site for intraosseous infusion of the tibia: an anatomical study. Clin Anat. 2003;16:15–18.
118 Anonymous. Guidelines for cardiopulmonary resuscitation and emergency cardiac care. Emergency Cardiac Care Committee and Subcommittees, American Heart Association. Part VI. Pediatric advanced life support. JAMA. 1992;268:2262–2275.
119 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: pediatric advanced life support. Pediatrics. 2006;117:e1005–e1028.
120 Goldstein B, Doody D, Briggs S. Emergency intraosseous infusion in severely burned children. Pediatr Emerg Care. 1990;6:195–197.
121 Hurren JS, Dunn KW. Intraosseous infusion for burns resuscitation. Burns. 1995;21:285–287.
122 Tobias JD, Ross AK. Intraosseous infusions: a review for the anesthesiologist with a focus on pediatric use. Anesth Analg. 2010;110:391–401.
123 Gazin N, Auger H, Jabre P, et al. Efficacy and safety of the EZ-IO intraosseous device: out-of-hospital implementation of a management algorithm for difficult vascular access. Resuscitation. 2011;82:126–129.
124 Sunde GA, Heradstveit BE, Vikenes BH, Heltne JK. Emergency intraosseous access in a helicopter emergency medical service: a retrospective study. Scand J Trauma Resusc Emerg Med. 2010;18:52.
125 Levitan RM, Bortle CD, Snyder TA, et al. Use of a battery-operated needle driver for intraosseous access by novice users: skill acquisition with cadavers. Ann Emerg Med. 2009;54:692–694.
126 Frascone RJ, Jensen J, Wewerka SS, Salzman JG. Use of the pediatric EZ-IO needle by emergency medical services providers. Pediatr Emerg Care. 2009;25:329–332.
127 Horton MA, Beamer C. Powered intraosseous insertion provides safe and effective vascular access for pediatric emergency patients. Pediatr Emerg Care. 2008;24:347–350.
128 Tsui BC, Richards GJ, Van Aerde J. Umbilical vein catheterization under electrocardiogram guidance. Paediatr Anaesth. 2005;15:297–300.
129 Cohen M, Sprigg A, Roberts I, Bustani P. Subcapsular haematoma and multifocal necrosis as fatal liver complications following umbilical vein catheterisation in a premature baby. Eur J Pediatr Surg. 2006;16:55–57.
130 Hermansen MC, Hermansen MG. Intravascular catheter complications in the neonatal intensive care unit. Clin Perinatol. 2005;32:141–156. vii
131 Liao CH, Sy LB, Tsou KI. Umbilical vein catheter malposition: report of one case. Acta Paediatr Taiwan. 2003;44:38–40.
132 Kim JH, Lee YS, Kim SH, et al. Does umbilical vein catheterization lead to portal venous thrombosis? Prospective US evaluation in 100 neonates. Radiology. 2001;219:645–650.
133 Beluffi G, Vivarelli M, Mongini ME, Chiara A. Hepatic calcification following umbilical vein catheterization in a premature baby. Eur Radiol. 2004;14:1320–1321.
134 Guimaraes H, Castelo L, Guimaraes J, et al. Does umbilical vein catheterization to exchange transfusion lead to portal vein thrombosis? Eur J Pediatr. 1998;157:461–463.
135 Rehan VK, Cronin CM, Bowman JM. Neonatal portal vein thrombosis successfully treated by regional streptokinase infusion. Eur J Pediatr. 1994;153:456–459.
136 Brans YW, Ceballos R, Cassady G. Umbilical catheters and hepatic abscesses. Pediatrics. 1974;53:264–266.
137 Fey D, Perrotta L. Peritoneal perforation resulting from umbilical vein catheterization: an unusual pattern. J Pediatr. 1973;83:501.
138 Orloff MJ, Orloff MS, Rambotti M. Treatment of bleeding esophagogastric varices due to extrahepatic portal hypertension: results of portal-systemic shunts during 35 years. J Pediatr Surg. 1994;29:142–151.
139 Vos LJ, Potocky V, Broker FH, et al. Splenic vein thrombosis with oesophageal varices: a late complication of umbilical vein catheterization. Ann Surg. 1974;180:152–156.
140 Van Niekerk M, Kalis NN, Van der Merwe PL. Cardiac tamponade following umbilical vein catheterization in a neonate. S Afr Med J. 1998;88:C87–C90.
141 Cole AF, Rolbin SH. A technique for rapid catheterization of the umbilical artery. Anesthesiology. 1980;53:254–255.
142 Kanarek KS, Kuznicki MB, Blair RC. Infusion of total parenteral nutrition via the umbilical artery. JPEN J Parenter Enteral Nutr. 1991;15:71–74.
143 Sherman NJ. Umbilical artery cutdown. J Pediatr Surg. 1977;12:723–724.
144 Coleman MM, Spear ML, Finkelstein M, et al. Short-term use of umbilical artery catheters may not be associated with increased risk for thrombosis. Pediatrics. 2004;113:770–774.
145 Cohen RS, Ramachandran P, Kim EH, Glasscock GF. Retrospective analysis of risks associated with an umbilical artery catheter system for continuous monitoring of arterial oxygen tension. J Perinatol. 1995;15:195–198.
146 Barrington KJ. Umbilical artery catheters in the newborn: effects of catheter design (end vs side hole). Cochrane Database Syst Rev. 2000. CD000508
147 Adelman RD, Karlowicz MG. What is the appropriate workup and treatment for an infant with an umbilical artery catheter-related thrombosis? Semin Nephrol. 1998;18:362–364.
148 Fletcher MA, Brown DR, Landers S, Seguin J. Umbilical arterial catheter use: report of an audit conducted by the Study Group for Complications of Perinatal Care. Am J Perinatol. 1994;11:94–99.
149 Ford KT, Teplick SK, Clark RE. Renal artery embolism causing neonatal hypertension: a complication of umbilical artery catheterization. Radiology. 1974;113:169–170.
150 Plumer LB, Kaplan GW, Mendoza SA. Hypertension in infants: a complication of umbilical arterial catheterization. J Pediatr. 1976;89:802–805.
151 Barrington KJ. Umbilical artery catheters in the newborn: effects of position of the catheter tip. Cochrane Database Syst Rev. 2000. CD000505
152 Barrington KJ. Umbilical artery catheters in the newborn: effects of heparin. Cochrane Database Syst Rev. 2000. CD000507
153 Lott JW, Conner GK, Phillips JB. Umbilical artery catheter blood sampling alters cerebral blood flow velocity in preterm infants. J Perinatol. 1996;16:341–345.
154 Anonymous.Relationship of intraventricular hemorrhage or death with the level of umbilical artery catheter placement: a multicenter randomized clinical trial. Umbilical Artery Catheter Trial Study Group. Pediatrics. 1992;90:881–887.
155 Rudolph N, Wang HH, Dragutsky D. Gangrene of the buttock: a complication of umbilical artery catheterization. Pediatrics. 1974;53:106–109.
156 Munoz ME, Roche C, Escriba R, Martinez-Bermejo A, Pascual-Castroviejo I. Flaccid paraplegia as complication of umbilical artery catheterization. Pediatr Neurol. 1993;9:401–403.
157 Inglis GD, Davies MW. Prophylactic antibiotics to reduce morbidity and mortality in neonates with umbilical artery catheters. Cochrane Database Syst Rev. 2004. CD004697
158 Bauer SB, Feldman SM, Gellis SS, Retik AB. Neonatal hypertension: a complication of umbilical-artery catheterization. N Engl J Med. 1975;293:1032–1033.
159 Todres ID, Rogers MC, Shannon DC, Moylan FM, Ryan JF. Percutaneous catheterization of the radial artery in the critically ill neonate. J Pediatr. 1975;87:273–275.
160 Cole FS, Todres ID, Shannon DC. Technique for percutaneous cannulation of the radial artery in the newborn infant. J Pediatr. 1978;92:105–107.
161 Ducharme FM, Gauthier M, Lacroix J, Lafleur L. Incidence of infection related to arterial catheterization in children: a prospective study. Crit Care Med. 1988;16:272–276.
162 Furfaro S, Gauthier M, Lacroix J, et al. Arterial catheter-related infections in children: a 1-year cohort analysis. Am J Dis Child. 1991;145:1037–1043.
163 Sellden H, Nilsson K, Larsson LE, Ekstrom-Jodal B. Radial arterial catheters in children and neonates: a prospective study. Crit Care Med. 1987;15:1106–1109.
164 Scheer B, Perel A, Pfeiffer UJ. Clinical review: complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care. 2002;6:199–204.
165 Kahler AC, Mirza F. Alternative arterial catheterization site using the ulnar artery in critically ill pediatric patients. Pediatr Crit Care Med. 2002;3:370–374.
166 Lo NS, Leung PM, Lau KC, Yeung CY. Congenital cardiovascular malformations in Chinese children with Down’s syndrome. Chin Med J (Engl.). 1989;102:382–386.
167 Lo RN, Leung MP, Lau KC, Yeung CY. Abnormal radial artery in Down’s syndrome. Arch Dis Child. 1986;61:885–890.
168 Kohonen M, Teerenhovi O, Terho T, Laurikka J, Tarkka M. Is the Allen test reliable enough? Eur J Cardiothorac Surg. 2007;32:902–905.
169 Buakham C, Kim JM. Cannulation of a nonpalpable artery with the aid of a Doppler monitor. Anesth Analg. 1977;56:125–126.
170 Morray JP, Brandford HG, Barnes LF, Oh SM, Furman EB. Doppler-assisted radial artery cannulation in infants and children. Anesth Analg. 1984;63:346–348.
171 Shinozaki T, Deane RS, Mazuzan JE. The dynamic responses of liquid-filled catheter systems for direct measurements of blood pressure. Anesthesiology. 1980;53:498–504.
172 Galvis AG, Donahoo JS, White JJ. An improved technique for prolonged arterial catheterization in infants and children. Crit Care Med. 1976;4:166–169.
173 Lowenstein E, Little JW, Lo HH. Prevention of cerebral embolization from flushing radial-artery cannulas. N Engl J Med. 1971;285:1414–1415.
174 Bedford RF. Radial arterial function following percutaneous cannulation with 18- and 20-gauge catheters. Anesthesiology. 1977;47:37–39.
175 Hager DL, Wilson JN. Gangrene of the hand following intra-arterial injection. Arch Surg. 1967;94:86–89.
176 Katz AM, Birnbaum M, Moylan J, Pellett J. Gangrene of the hand and forearm: a complication of radial artery cannulation. Crit Care Med. 1974;2:270–272.
177 Miyasaka K, Edmonds JF, Conn AW. Complications of radial artery lines in the paediatric patient. Can Anaesth Soc J. 1976;23:9–14.
178 Amato JJ, Solod E, Cleveland RJ. A “second” radial artery for monitoring the perioperative pediatric cardiac patient. J Pediatr Surg. 1977;12:715–717.
179 Gauderer M, Holgersen LO. Peripheral arterial line insertion in neonates and infants: a simplified method of temporal artery cannulation. J Pediatr Surg. 1974;9:875–877.
180 Prian GW, Wright GB, Rumack CM, O’Meara OP. Apparent cerebral embolization after temporal artery catheterization. J Pediatr. 1978;93:115–118.
181 Cilley RE. Arterial access in infants and children. Semin Pediatr Surg. 1992;1:174–180.
182 Park MK, Guntheroth WG. Direct blood pressure measurements in brachial and femoral arteries in children. Circulation. 1970;41:231–237.
183 Bogart DB, Bogart MA, Miller JT, et al. Femoral artery catheterization complications: a study of 503 consecutive patients. Cathet Cardiovasc Diagn. 1995;34:8–13.
184 Riker AI, Gamelli RL. Vascular complications after femoral artery catheterization in burn patients. J Trauma. 1996;41:904–905.
185 Taylor LMJ, Troutman R, Feliciano P, et al. Late complications after femoral artery catheterization in children less than five years of age. J Vasc Surg. 1990;11:297–304.
186 Macnicol MF, Anagnostopoulos J. Arrest of the growth plate after arterial cannulation in infancy. J Bone Joint Surg Br. 2000;82:172–175.