7 Problems of the female genital tract
Benign conditions of the vulva
Vulvodynia
Carcinoma of the vulva
FIGO staging
• Stage 0 – carcinoma in situ (preinvasive)
• Stage 1 – tumour confined to vulva or vulva and perineum < 2 cm in diameter with no nodal involvement
• Stage 2 – tumour > 2 cm in diameter with no nodal involvement
• Stage 3 – spread of tumour to urethra, vagina or anus or unilateral involvement of nodes. This stage has been subdivided into A, B or C according to number and nature of lymph node metastases. These changes reflect the fact that the number of nodes involved is a more significant prognostic factor than fully resected local disease
• Stage 4 – tumour within rectum, bladder, bone or distant metastases and bilateral nodal involvement.
Benign conditions of the cervix
Cervical neoplasia
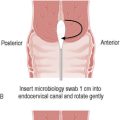
Cervical cytology
Definitions:
• Inflammatory – this means that there are increased polymorphs and this may occur during the premenstrual or menstrual phases of the cycle.
• Mild squamous changes – mainly due to inflammation or an artefact of poor fixation, which will require a repeat smear in 6 months.
• Hyperkeratosis – may be due to HPV or uterovaginal prolapse, but CIN may be present in less than 5%.
• Dyskaryosis – this is the term used for cells that come from a dysplastic or neoplastic lesion.
• Transformation zone – this is the area between the original and existing squamocolumnar junction and is where the columnar epithelium undergoes metaplasia. This zone may extend up the cervical canal, especially in the postmenopausal patient.
Carcinoma of the cervix
Investigations
• Stage 1: carcinoma confined to the cervix
• Stage 2: carcinoma extending beyond the cervix but not to pelvic side walls. The carcinoma involves the vagina but not the lower third of vagina
• Stage 3: carcinoma spread to pelvic side wall or lower third of vagina. Would include all cases of hydronephrosis or renal failure secondary to ureteric obstruction
• Stage 4: carcinoma extending beyond the true pelvis or involving the mucosa of bladder or rectum.
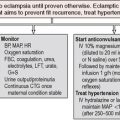
Management
Surgery
Preoperative assessment:
Technique:
Radical hysterectomy involves the following:
• Vertical midline or Cherney/Maylard incision. Minimal-access surgery is now an option, either laparoscopically or robot-assisted
• Assess for ascites, assess liver, spleen, undersurface of diaphragm, kidneys, ureters, omentum, appendix
• Removal of uterus, cervix, plus or minus ovaries and tubes, parametria, upper third of vagina and pelvic nodes.
Early-stage cervical cancer
Benign tumours of the uterus
Uterine fibroids
Endometrial carcinoma
FIGO staging of endometrial cancer (updated 2009)
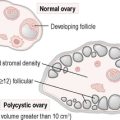
Tumours of the ovary
Epithelial tumours
1. Serous cystadenoma or adenocarcinoma – this is the commonest form of ovarian carcinoma, accounting for 50% of ovarian malignancy, but both benign and malignant varieties exist.
2. Mucinous cystadenoma or adenocarcinoma – these are less commonly malignant, accounting for 10% of ovarian carcinomas. They are usually large ovarian cysts.
3. Endometrioid carcinoma – this malignant variety of ovarian carcinoma accounts for 25% of ovarian carcinomas and is associated with endometrial malignancy in 20% of cases.
4. Clear-cell carcinoma – this is a malignant tumour that accounts for 10% of ovarian carcinoma and carries a particularly poor prognosis.
Brenner’s tumour is a rare form of ovarian neoplasm that is usually small and benign.
Germ cell tumours
1. Teratoma (dermoid cyst) – this is a common benign cyst in young women that may contain tissue from all the cell lines derived from the primordial germ cells of the ovary, including hair and teeth. They are usually small, bilateral and asymptomatic, but can cause pain if the ovary torts or the cyst ruptures. They can, rarely, undergo malignant change to solid teratomas.
2. Dysgerminoma – this is a rare tumour of the ovary overall, but is the commonest type of ovarian malignancy in the younger age group.
Sex cord tumours
This type of ovarian tumour is derived from the ovarian stroma and there are three varieties:
1. Granulosa cell tumours – these are slow-growing malignant tumours of the ovary, which are usually malignant. They are rare and secrete oestrogen, and so may cause postmenopausal bleeding or endometrial hyperplasia or carcinoma in this group of women.
2. Thecomas – these are similar to the granulosa cell tumours, secreting oestrogen and, therefore, causing similar effects, but are rare and usually benign, e.g. Sertoli–Leydig tumours.
3. Fibromas – these are benign tumours that are uncommon and are often associated with ascites and pleural effusions as part of Meigs’ syndrome.
Ovarian carcinoma
Management
Gynaecological cancer in pregnancy
Carcinoma of the cervix
Management
1. Low-grade abnormality on smear – followed up with a further smear test in 12 months.
2. High-grade abnormality on smear – mandatory colposcopy, avoid biopsy if possible (but this will be unavoidable if invasive carcinoma is suspected), but repeat colposcopy at 24–28 weeks’ gestation to exclude progression of disease. Follow up postpartum for biopsy if necessary.
3. Suspected microinvasion – may indicate need for cold-knife cone biopsy during pregnancy. This procedure carries a significant risk of morbidity for both mother and fetus.
4. Invasive carcinoma – adequate staging is essential. Management will depend on extent of stage, gestation at diagnosis and patient’s wishes for continuing pregnancy. Generally, definitive treatment can be deferred if the carcinoma is diagnosed in the third trimester. If the carcinoma is at a stage that responds to surgery, most gynaecologists would advise elective caesarean section followed by a radical hysterectomy.
Summary
• Cervical smears are an effective screening technique for cervical carcinoma.
• Cervical carcinoma is the second commonest female cancer after breast carcinoma, followed by ovarian and then endometrial.
• Uterine fibroids are the commonest benign tumours of the female genital tract.
• Ovarian cysts are common and management has been improved with the development of ultrasound and tumour markers.
• Ovarian carcinoma usually presents late and is therefore the main cause of mortality from gynaecological cancer.