Principles of Ultrasound
Christopher J. Gallagher and John C. Sciarra
Nature of Ultrasound: Compression and Rarefaction
Ultrasound is sound waves propagated through a medium at a frequency above that which we can hear. Imaging depends on displaying the time required for an ultrasound pulse to go to a cardiac structure and return. We acoustically challenged humans only hear from 20 cycles/second to 20 000 cycles/second, or 20 kilohertz (named after the famous physicist and car-rental magnate).
Keep in mind that sound, or ultrasound, must get propagated through a medium.
Frequency, Wavelength, and Tissue Propagation Velocity
Note that frequency is the number of complete cycles per second, and wavelength is the distance from one corresponding area to the next (usually peak to peak). Propagation velocity is the wavelength ∞ frequency.

Ultrasound–Tissue Interactions
Reflection
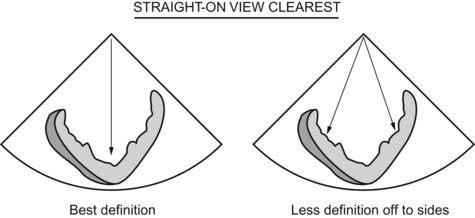
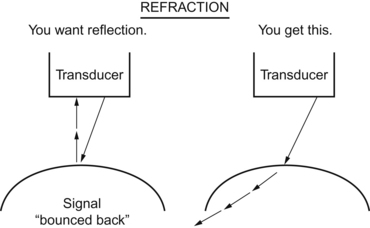
Since reflection is the key to the kingdom, and you prefer a “straight on” bounce coming back to your transducer, it makes sense that your best view is straight on, at 180 degrees to the transducer. At any angle other than 90 degrees, some of the signal will bounce “away” from the transducer.
Tissue Characterization
The meaty tissues are denser, absorb more ultrasound, and look gray. Blood is less dense, and looks black. (Adjust the gain until you get gray for the tissue, black for the blood.) Calcified areas eat up all the ultrasound waves and look white. If dense enough, they don’t allow ultrasound to go any further and thus throw a shadow distal to them, leading to artifacts. Calcified things can also cause reflections that “fake out” the transducer and produce artifacts.