10 PRINCIPLES OF JOINT AND PERIARTICULAR ASPIRATIONS AND INJECTIONS
Indications for Aspiration and Injection of Joints and Periarticular Lesions
Aspiration and injection of joints and periarticular synovium-lined cavities (bursae and tendon sheaths) and injection of soft-tissue lesions (entheses, tendinitis, compression neuropathies, epidural sac) are indicated in the diagnosis and treatment of various musculoskeletal disorders. These are summarized in Table 10-1.
TABLE 10-1 INDICATIONS FOR ASPIRATION AND INJECTION OF JOINTS AND PERIARTICULAR LESIONS
| Diagnosis |
| Diagnostic synovial fluid analysisSeptic arthritis, hemarthrosis, crystal arthritis, differentiation of inflammatory from noninflammatory arthritis |
| Diagnostic studies |
IA, intraarticular; OA, osteoarthritis
(From Silva M, Luck JV Jr, Siegel ME. 32P chromic phosphate radiosynovectomy for chronic haemophilic synovitis. Haemophilia 2001;7 Suppl 2:40–49.)
Contraindications for Aspiration and Injection of Joints and Periarticular Lesions
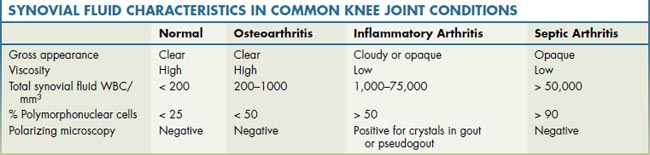
The relative contraindications to intraarticular (IA) and periarticular injections of corticosteroids are summarized in Table 10–2. If infection is suspected in the joint, bursa, or tenosynovium, it should be aspirated and the synovial fluid examined for cell count, differential, and culture. In the setting of an inflamed joint, if the clinical diagnosis is unclear, or the aspirated fluid suggests possible infection, the aspirated fluid should be sent for cell count, differential, culture, and polarizing microscopy for crystals (Table 10-3). Intrasynovial corticosteroid injections may exacerbate an infection and are not recommended if there is suspicion of infection. Joint injection is also best avoided if there is bacteremia or infection of the overlying skin or subcutaneous tissue or in the presence of overlying skin lesions, such as extensive psoriatic plaques.
TABLE 10-2 RELATIVE CONTRAINDICATIONS TO INTRAARTICULAR AND PERIARTICULAR CORTICOSTEROID INJECTIONS
| Suspected joint infection |
| Overlying cellulitis or other skin infection |
| Systemic bacteremia |
| Thrombocytopenia, bleeding disorders |
| Prosthetic joints |
| Osteonecrosis, IA fracture or severely destroyed or unstable joint |
| Tendon tears and steroid injections near the Achilles tendon |
| Multiple or high-dose IA steroid injections in patients with uncontrolled diabetes mellitus, hypertension, congestive heart failure, or psychosis |
| Skin surface area covered by psoriatic plaques |
| Hypersensitivity to local anesthetic (steroid alone may be used) |
| Reluctant patient |
IA, intraarticular
Complications of Intrasynovial and Periarticular Corticosteroid Injections
The potential complications of IA and intralesional corticosteroid injections are summarized in Table 10-4. The risk of infection after intrasynovial corticosteroid injections is very low; among practicing rheumatologists, one study documented the rate at less than 1 per 75,000 procedures, while a study of primary care practitioners in Britain prospectively documented no infections following 1147 steroid injections. Infection rates can be minimized by observing stringent aseptic “no-touch” techniques and by using sterile disposable needles and syringes and single-dose vials of corticosteroid and lidocaine. Local aspirations and injections can occasionally result in minor hemorrhage in the joint (hemarthrosis) or periarticular tissues (ecchymosis).
TABLE 10-4 COMPLICATIONS OF INTRAARTICULAR AND INTRALESIONAL CORTICOSTEROID INJECTIONS
| Introduction of infection |
| IA or periarticular hemorrhage |
| Postinjection flare |
| Destructive arthritis (“steroid arthropathy”) from multiple IA injections into weight-bearing, partially damaged joints |
| Systemic Effects |
| Transient facial flush, warmth, and diaphoresis |
| Worsening of diabetic control, hypertension, heart failure, or psychosis |
| Suppression of HPA axis |
| Iatrogenic Cushing syndrome |
| Local Effects |
| Leakage of steroid along needle tract |
| Atrophy of subcutaneous fat, depigmentation, telangiectasia, and periarticular calcifications |
| Misplaced injections |
| Tendon rupture, nerve damage, cartilage injury, subcutaneous fat granuloma, and sterile abscess formation |
| Rare Reactions |
| Pancreatitis, hypersensitivity reactions, uterine bleeding, central serous chorioretinopathy, posterior subcapsular cataract, osteonecrosis |
HPA, hypothalamic–pituitary–adrenal; IA, intraarticular
Technique of Joint Aspiration and Injection
EQUIPMENT
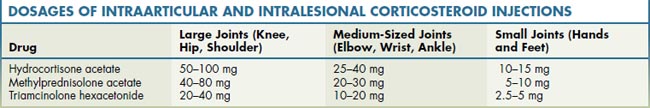
Aspiration or injection of joints and soft tissues is an outpatient procedure that does not require specialized equipment. The equipment used includes povidone iodine or chlorhexidine, alcohol swabs, gauze pads, 1% or 2% lidocaine, ethyl chloride spray, disposable needles and syringes of various sizes, gloves, a corticosteroid preparation (Table 10-5), prepared small-patch dressing (e.g., Band-Aid), specimen bottles, and forceps.
PREPARATIONS OF INTRAARTICULAR AND PERIARTICULAR CORTICOSTEROID INJECTIONS
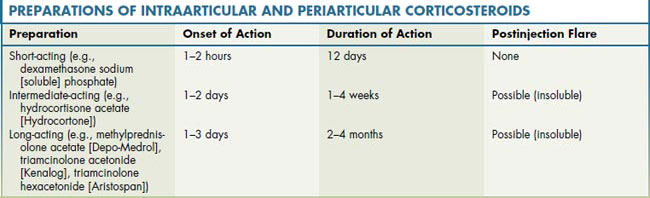
Corticosteroid preparations are divided into three categories based on potency and approximate duration of action of the drug (Table 10-6; see Table 10-5 also). Hydrocortisone, which can be synthesized, is the natural corticosteroid preparation. Prednisolone is less soluble, and the addition of methyl and acetate groups further reduces its solubility and prolongs its duration of action. The introduction of a fluorine atom to form triamcinolone enhances potency, and the addition of acetonide prolongs the duration of action. Therefore, the ranking order of potency is hydrocortisone, prednisolone salts, and then triamcinolone. Although triamcinolone is a highly effective preparation with a longer duration of action, it causes greater subcutaneous fat atrophy when leaked or injected extraarticularly compared to other steroid preparations. For this reason, use of prednisolone is preferred for periarticular injections.
Berger R.G., Yount N.J. Immediate “steroid flare” from intra-articular triamcinolone hexacetonide injection: Case report and review of the literature. Arthritis Rheum.. 1990;33:1284-1286.
Bernstein R.M. Injections and surgical therapy in chronic pain. Clin. J. Pain. 2001;17:S94-S104.
Bird H.A. Intra-articular and intralesional therapy. In: Hochberg M.C., Silman A.J., Smolen J.S., et al, editors. Rheumatology. third ed. Edinburgh: Mosby; 2003:393-397.
Canoso J.J. Aspiration and injection of joints and periarticular tissues. In: Hochberg M.C., Silman A.J., Smolen J.S., et al, editors. Rheumatology. third ed. Edinburgh: Mosby; 2003:233-244.
Dieppe P.A., Klippel J.H. Aspiration and injection of joints and periarticular tissues. In: Klippel J.H., Dieppe P.A., editors. Practical Rheumatology. first ed. London: Mosby; 1995:111-113.
Fam A.G. The ankle and foot. In: Klippel J.H., Dieppe P.A., editors. Practical Rheumatology. first ed. London: Mosby; 1995:120.
Grassi W., Farina A., Fillippucci E., Cervini C. Sonographically guided procedures in rheumatology. Semin. Arthritis Rheum.. 2001;30:347-353.
Gray R.C., Gottlieb N.L. Intra-articular corticosteroids: An updated assessment. Clin. Orthop.. 1983;177:235-263.
Jones A., Regan M., Ledingham J., et al. Importance of placement of intra-articular steroid injection. Br. Med. J.. 1993;307:1329-1330.
Kumar N., Newman R.J. Complications of intra- and peri-articular steroid injections. Br. J. Gen. Prac. 1999;49:465-466.
Pfenninger J.L. Injections of joints and soft tissues. Part I: General guidelines. Am. Fam. Physician. 1991;44:1196-1202.
Seror P., Pluvinage P., d’Andre F.L., et al. Frequency of sepsis after local corticosteroid injection (an inquiry on 1,160,000 injections in rheumatological private practice in France). Rheumatology (Oxford). 1999;38:1272-1274.
Speed C.A. Corticosteroid injections in tendon lesions. Br. Med. J.. 2001;323:382-386.