connective tissue
Blood may be categorised as a connective tissue since its cells arise from mesoderm, but the extracellular matrix (plasma) is fluid (Chapter 8). Bone and cartilage are classified as connective tissues and they have an extracellular matrix that is relatively solid. In the case of bone, the matrix is mineralised with calcium salts which confer rigidity to the bone and the ability to resist deforming forces (Chapter 9).
Cell types in connective tissue (excluding blood, bone and cartilage)
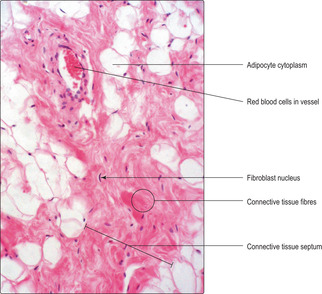
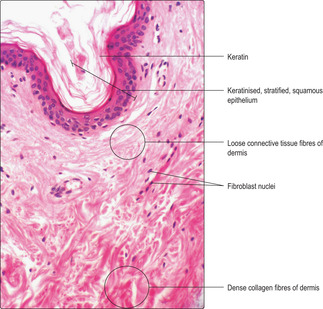
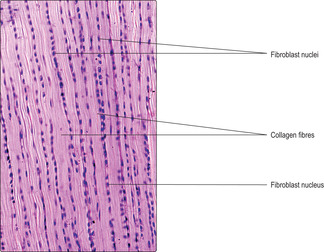
The major cell type found in many connective tissues is the fibroblast. In many instances, fibroblasts are identified by their densely stained, elongated nuclei which do not appear to be associated with much cytoplasm (Figs 4.1 and 4.2). Fibroblasts secrete long, fibre-like protein molecules (e.g. collagen and elastin) and many of the other large molecules in the extracellular matrix.
If connective tissue is damaged, it may be repaired by the ability of fibroblasts to undergo mitosis and to synthesise new matrix. If fibroblasts are actively secreting matrix proteins, their appearance is changed: their nuclei are larger and relatively palely stained and nucleoli are apparent (Chapter 3, see Fig. 3.2). This appearance is a result of the activity of the DNA (and nucleolus) in the synthetic processes which produce new molecules for the extracellular matrix. (Conventionally, a cell with the suffix ‘blast’ indicates a rapidly dividing cell. However, in the case of the fibroblast, the term is usually reserved for the differentiated non-dividing cell, which might more appropriately be known as a fibrocyte.)
Several other types of cell occur in connective tissues; some are restricted to a particular type of connective tissue and others to the functional state of the tissue.
They are:
■ mast cells, which store granules containing specific molecules (e.g. histamine). When released from mast cells these molecules modify the permeability of blood vessels as part of an inflammatory reaction (Chapter 8)
■ macrophages, which are able to phagocytose and digest bacteria and cell debris. They are also able to phagocytose, but not digest, inert substances, e.g. carbon particles. In addition, they aid the immune response to antigens (Chapter 8)
■ white blood cells and plasma cells, which may be in transit through the connective tissue or responding locally as part of an immune response (Chapter 8)
■ adipocytes, which store fats (lipids) in their cytoplasm (Fig. 4.1). The fats may be metabolised and provide energy and various metabolites when needed. Adipocytes also provide insulation, give shape to the body and act as physical protection, e.g. around the kidney.
Extracellular matrix of connective tissue
Ground substance
Ground substance is a complex mixture of large molecules containing carbohydrates and protein, and tissue fluid containing water, salts, other small, soluble molecules and dissolved gases. The tissue fluid component ensures gases and nutrients move readily between blood vessels and connective tissue cells and other cells in the region. The large molecules (glycoproteins, proteoglycans and glycosoaminoglycans) bind the components of the extracellular matrix together altering the viscosity of the gel-like matrix and conferring on it different properties. In addition, the matrix molecules act as adhesion sites for various transient cell types which may be involved in immune responses.
Protein fibres
The protein fibres that are present in extracellular matrix of connective tissues are of two main types: collagen and elastin. Collagen is characterised by tensile strength and elastin by elasticity.
Collagen
Collagen is synthesised by fibroblasts and about 20 types have been identified but only a few are common. Different types of collagen are found in specific locations:
■ types I and II collagen are in bone and skin (Fig. 4.2) and provide strength
■ type II is in cartilage and provides strength and allows some distortion and recoil
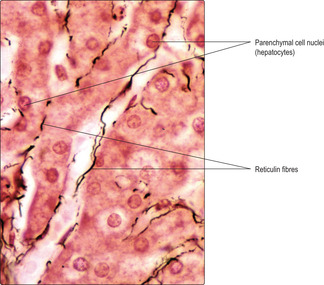
■ type III (known as reticulin) provides fine supporting fibres, e.g. for liver cells (Fig. 4.3)
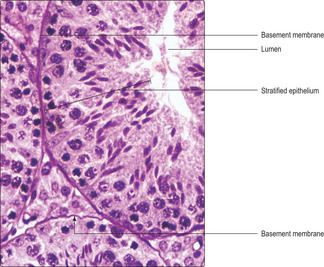
■ type IV is in basement membranes and provides firm attachments for epithelial cells (Fig. 4.4).
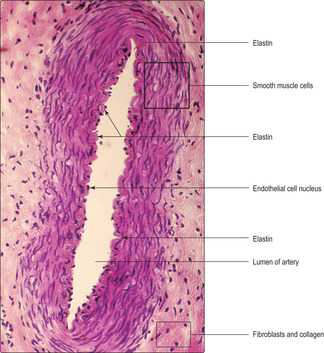
Elastin
Elastin molecules are also made and secreted by fibroblasts. The molecules may be formed into sheets (laminae) or distributed irregularly as fibres. Elastin molecules are predominantly in parts of the body where deformation and reformation occurs. Elastin is present in skin and in the walls of arteries (Fig. 4.5). Some arteries are distended as blood is pumped into them and then they recoil (owing to the elastin fibres recoiling), thus ensuring the blood continues to flow (Chapter 10).
Connective tissue types
Connective tissues may be divided into three major types (excluding bone, cartilage and blood):
■ connective tissue ‘proper’ is also described as generalised connective tissue and is subdivided into loose (areolar) or dense categories depending on the arrangement of the protein fibres
■ reticular connective tissue has fine fibres of reticulin which form a fine supporting meshwork
■ adipose connective tissue in which adipocytes (fat) cells are predominant.
Vitamin C deficiency Vitamin C is essential for the synthesis of normal collagen. Normally, collagen molecules are replaced several months after they are formed by new collagen. If vitamin C is absent from the diet for prolonged periods the condition known as scurvy develops and the new collagen that replaces the old is abnormal. Collagen attaches teeth to the sockets in jaw bones; in extremely severe cases of scurvy, the teeth drop out of the sockets because the new collagen is defective.
Marfan syndrome In this condition a genetic mutation results in the abnormal function of elastin fibres in the body. Many regions are affected but, in particular, the loss of the normal elastin component in the wall of the aorta (the main blood vessel from the heart supplying the body) can be serious as the wall may rupture; this is usually fatal.
Connective tissue proper
Loose areolar connective tissue
Loose areolar connective tissue occupies spaces that no other organs or tissues occupy: it is packing material. It underlies the skin (the hypodermis), surrounds delicate organs and skeletal muscles, and acts as filler around blood vessels and nerves. Loose connective tissue physically connects many parts of the body, e.g. it binds together the constituents of the walls of the gastrointestinal, respiratory, urinary and reproductive tracts. It is also present in the delicate membranes attaching organs or tubes to other structures, e.g. the membranes of the gut (Fig. 4.6). In addition to its ‘connective’ role, areolar tissue also acts as a medium for the transport of gases and other molecules between blood vessels and surrounding cells and is a region where various cell types such as the cells of the immune system (Chapter 8) can interact. Transient cell types such as white blood cells may also be present in areolar tissue. Loose connective tissue may respond to trauma or infection by becoming oedematous and infiltrated by increased numbers of white blood cells and other immune-related cells (signs of inflammation).
Loose connective tissue is characterised by abundant amounts of ground substance, and by fibroblasts which are usually widely spaced and may appear to have little or no cytoplasm. In histological sections ground substance may appear as empty spaces since many components may have been extracted during the processing of the tissue. Also present in loose connective tissue are varying proportions of collagen and elastin which appear as pink strands in routine H&E preparations (Figs 4.1 and 4.2). Some components of connective tissue can be more readily revealed by various special staining techniques (Figs 4.6 and 4.7).
Dense connective tissue
Dense connective tissue may be classified as regular or irregular with regard to the arrangement of the fibres. The former is arranged as bundles of similarly oriented, densely packed collagen fibres which resist tensile forces, such as those applied to tendons (Fig. 4.8) and ligaments. The predominant cell type is the fibroblast. However, given the tight packing of the collagen fibres, there is relatively little space for extracellular matrix or transient cells. Dense, irregular connective tissue also has densely packed collagen fibres, but they are arranged irregularly and resist tensile forces from many directions. Again, the predominant cell type is the fibroblast and there is little space for extracellular material or transient cells. A typical site for this type of connective tissue is the deep region of the dermis of the skin (Fig. 4.2).
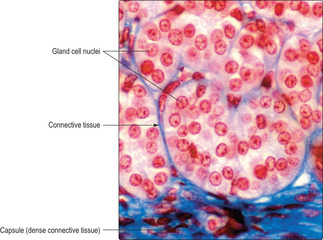
Reticular connective tissue
The fine collagen fibres of reticulin act as a delicate framework for the parenchymal cells of several organs, e.g. the liver (Fig. 4.3) and endocrine glands (Fig. 4.7), where minimal impedance to the transport of large molecules is important. Reticulin also provides a support network for immune cells in the spleen, bone marrow and lymph nodes (Chapter 8).
Adipose connective tissue
There are two types of adipose tissue: white adipose and brown adipose tissue. White adipose tissue is the most prominent type in adults. It is also known as unilocular fat as each cell contains one fat droplet which occupies most of the cell. In brown fat, known as multilocular fat, the constituent cells store the fat as multiple droplets. Both types of adipose tissue have many blood vessels. White adipose tissue contains connective tissue fibres forming septa that break the tissue up into lobules (Fig. 4.1). This type of adipose tissue is found under the skin (subcutaneously), and it may be extensive in particular regions of the body. Brown fat is a reddish brown colour in life and its cells contain abundant mitochondria. The latter are related to its principal function, which is to release energy from the fat its cells contain. Much of this energy is heat and it aids temperature regulation in neonates. Brown fat is found in particular locations in the body; it is most evident in infants, although it is also found in the neck region of adults.
Connective tissue:
Cells in connective tissue include:
■ fibroblasts which synthesise the protein fibres and other large molecules in the ECM
■ mast cells which synthesise, store and secrete molecules that affect the permeability of blood vessels
■ macrophages which phagocytose and digest cell debris and microorganisms, and aid immune responses
■ white blood cells which migrate through the ECM and may remain localised as part of the immune response
■ adipocytes which store lipids.
Extracellular matrix consists of:
■ ground substance containing
■ water, salts, dissolved gases and small molecules
■ large molecules, e.g. glycoproteins, proteoglycans and glycosoaminoglycans which affect the viscosity and function of the ECM
■ molecules to which cells involved in immune responses adhere
■ protein fibres
■ collagen types I and II provide strength, e.g. in skin
■ collagen type III (also known as reticulin) provides delicate meshworks which support other cells, e.g. in the liver
■ collagen type IV forms basement membranes which support many epithelial cells
■ elastin fibres which are able to stretch and recoil.
Categories of connective tissues (other than bone, cartilage and blood) are:
■ proper connective tissue
■ loose connective tissue connects structures
■ dense connective tissue has little ECM
■ reticulin connective tissue
■ adipose connective tissue.