epithelial tissue
Introduction to primary issues
This classification is still in wide use and is the basis for all studies aimed at understanding the structure and function of normal and abnormal cells, tissues and organs of the body.
Epithelial tissues in general lie on surfaces (epi = on or upon) and many carry out secretory and other highly specialised functions. Cells from some epithelia migrate from surfaces during development in utero and form glands within the body (e.g. the pancreas) and produce and secrete various molecules. The names of the other primary tissues (connective, muscle and nerve) indicate the prime functions of the components of these tissues in their titles, respectively the connection of structures, contraction of muscles and conduction of nerve impulses.
Epithelial tissue
Epithelial tissue consists mainly of epithelial cells which form layers (epithelia) covering the body and structures in the body such as organs. Epithelial tissues also form the linings of hollow structures in the body and form the outer layer(s) of some membranes. Epithelial cells are the major cell type forming the parenchyma of some solid organs and glands and are involved in synthesising and secreting many substances. In addition to secretion, epithelia are involved in a variety of functions, including transport of substances, absorption of molecules, modulation of permeability and protection, and in detecting some sensations. Although epithelia exhibit a variety of forms and functions they all consist of epithelial cells which are tightly bound to each other by specialised junctions (Chapter 2). The importance of epithelia to body function is apparent when it is realised that every molecule or organism that enters (or leaves) the body has to pass through an epithelium.
Epithelia lining and covering structures
Epithelia are categorised as:
■ simple epithelia, which consist of a single layer of epithelial cells
■ compound (stratified) epithelia, which display several layers of cells.
In each of these categories there are sub-categories, classified according to the shape of the epithelial cells.
Simple epithelia
In simple epithelia, each epithelial cell is attached to a basement membrane (sometimes called a basal lamina). The basement membrane is a concentration of extracellular material, including glycoproteins and connective tissue fibres (mainly collagen) (Chapter 4).
Simple epithelia comprise four main types:
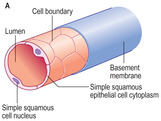
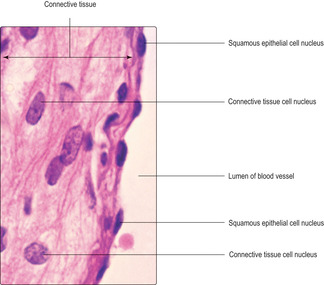
Simple squamous epithelia
Squamous epithelial cells are irregularly shaped, flattened (pavement like) and fit intimately together. The nuclei in squamous cells often occupy a central position, and, given that the cytoplasm of the cells is generally flattened, a bulge may be apparent in the region of the nucleus (Fig. 3.1A). An important function of simple, squamous epithelial cells is that they facilitate the transport of gases and/or other substances across the epithelium. Examples of the location of squamous epithelia include the linings of blood vessels (Fig. 3.2), which are known as endothelia, and the walls of lung alveoli, i.e. regions where the move-ment of oxygen and carbon dioxide is important.
Simple cuboidal epithelia
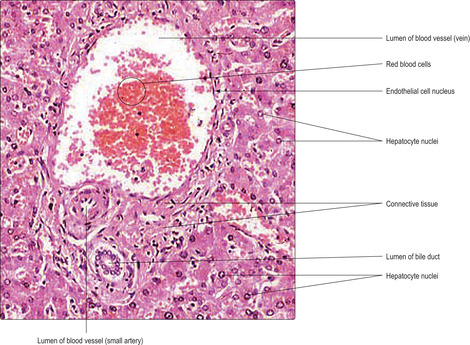
Epithelial cells in cuboidal epithelia are shaped like boxes, with fairly square profiles, and each cell has a roughly centrally placed nucleus. Unlike squamous cells, their nuclei do not bulge as there is ample cytoplasm around them (Fig. 3.1B). Examples of where this cell type may be found include the lining of the walls of ducts in the liver (Fig. 3.3) and the walls of ducts draining glands, e.g. sweat glands. Their function varies with their location and may involve synthesis and secretion, or excretion, or absorption of molecules.
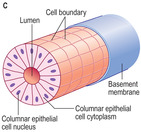
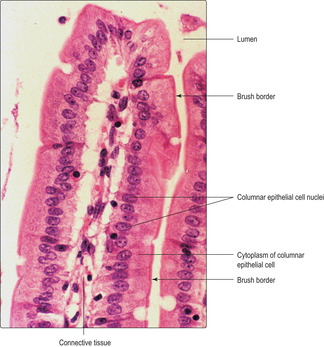
Simple columnar epithelia
Columnar epithelial cells have the shape of columns with their longest dimension at right angles to the basement membrane. Their nuclei typically lie near the basement membrane (Fig. 3.1C) or about half-way along their length. Columnar epithelial cells are present in the lining of the wall of the gastrointestinal tract (Fig. 3.4), the gall bladder and some tubules in the kidney, for example. In many locations, they are associated with the function of absorption of substances into the cells across their apical (luminal) surface and then out of the cells via the basal surface and then across their basement membrane. The apical surfaces of many absorptive columnar epithelial cells display a ‘brush border’ appearance (Fig. 3.4) when examined by light microscopy and this is due to the presence of microvilli (Chapter 2). The microvilli increase the surface area of the luminal membrane of absorptive cells and thus increase the efficiency of the transport of molecules.
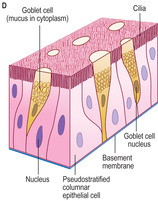
Pseudostratified columnar epithelia
This type of epithelium is called ‘pseudostratified’ because it appears as though it is composed of several layers but each cell actually has an attachment to the basement membrane (Fig. 3.1D). The appearance of stratification is because the nuclei in the various cells in the epithelium are located at different levels in relation to the basement membrane and a single section through the cells does not usually display the whole extent of their cytoplasm. This type of epithelium lines much of the respiratory tract (Fig. 3.5). Specialised epithelial cells are present in this ‘respiratory’ epithelium; some produce mucus (unicellular glands known as goblet cells) and others have cytoplasmic projections on their luminal surface known as cilia (Chapter 2). Together, cilia and mucus entrap solid particles, e.g. dust and bacteria. The cilia move in a synchronised beat, a bit like a whiplash, and this moves the mucus and its contents. The general direction of flow of the mucus is away from the lungs and towards the pharynx where most is swallowed.
Compound (stratified) epithelia
Compound (stratified) epithelia are composed of several layers of cells. Only cells in the deepest layer are attached to the basement membrane. Sub-categories are classified according to the shape of the surface epithelial cells:
■ stratified squamous
■ stratified cuboidal
■ stratified columnar
■ transitional.
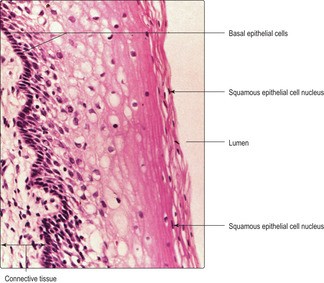
Stratified squamous epithelia
Stratified squamous epithelia have layers of cells of cuboidal or columnar shape but the surface cells are squamous (flattened and pavement like). Typical regions of the body where stratified squamous epithelia are present include the linings of the oesophagus, vagina (Fig. 3.6) and anal canal where the epithelia provide some physical protection from abrasion. The squamous surface cells are shed, especially when abrasion occurs, but they are replaced by deeper cells which become flattened as they move to the surface layer. Cells located at the base of the epithelium are the progenitor (stem) cells for the rest of the epithelial cells. Mitosis of these stem cells ensures that the layers of cells are constantly replaced as some new cells migrate to the surface. Importantly, some cells remain in the basal layer and continue to function as stem cells.
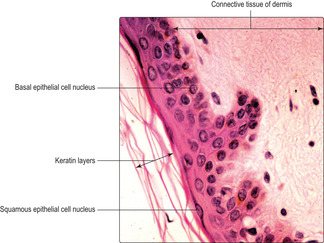
The cells in a specialised type of stratified squamous epithelium produce the protein keratin. The epithelium of the skin, known as the epidermis, is the main region of the body where this type of epithelium is present and it is categorised as a keratinised, stratified, squamous epithelium (Fig. 3.7). The keratin produced by the epithelial cells (keratinocytes) fills the cells in the upper layers of the epidermis and these cells become flattened and they die. Keratin from the dead cells forms the surface layers of the skin and it gradually flakes off (desquamates). Keratin makes the skin waterproof, reduces water loss by evaporation, provides protection from abrasion, and resists the penetration of the skin by many molecules and microorganisms.
Stratified cuboidal epithelia
The surface cells of stratified cuboidal epithelia are cuboidal in shape and usually only two layers are present. This type of epithelium lines ducts draining some glands, e.g. salivary glands.
Stratified columnar epithelia
This type of epithelium is present in only a few locations in the body, e.g. some large ducts and portions of the male urethra. Its deepest layer is typically low cuboidal and the surface cells are columnar in shape.
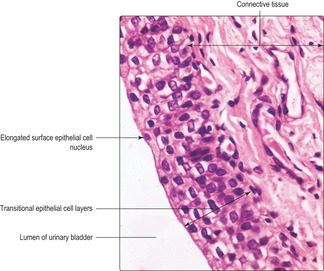
Transitional epithelium
This type of epithelium is a highly specialised stratified epithelium present only in the regions of the body in contact with urine. Transitional epithelium lines parts of the kidney, the ureters, the urinary bladder (Fig. 3.8) and parts of the urethra (Chapter 13). A key function of transitional epithelium is its ability to act as a permeability barrier between hypertonic urine and isotonic tissue fluid and blood. In addition, the transitional epithelium lining the bladder is able to stretch as the bladder distends and stores urine. The appearance of transitional epithelium depends on the amount it is stretched. In an empty bladder, numerous epithelial cell layers are apparent. As the volume of urine in the bladder increases, the surface epithelial cells become flattened and the number of layers of cells reduced, but, importantly, they continue to function as a permeability barrier.
Epithelial glands and membranes
Glands
There are two main functional types of gland in the body:
■ exocrine glands that secrete their products onto epithelial surfaces via ducts
■ endocrine glands that secrete their products (hormones) directly into blood vessels.
Other secretory gland cells are present in the body. Some, known as paracrine glands, secrete factors into adjacent regions, and unicellular glands such as goblet cells secrete mucus onto the surfaces of the gastrointestinal and the respiratory tract (Fig. 3.5), for example.
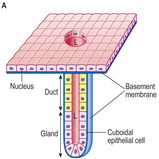
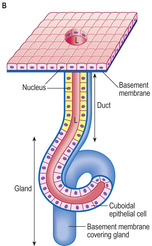
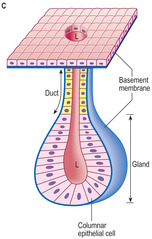
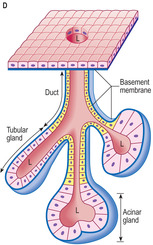
Structurally, exocrine glands are of two types: simple or compound. Simple glands are drained by a single, unbranched duct and the secretory cells forming the gland may be arranged as straight or coiled tubules or in a spherical arrangement described as ‘acinar’ (Fig. 3.9A,B,C, respectively). Compound glands have a branching duct system that carries the secretion from gland cells arranged as tubules or acini or a combination of the two (Fig. 3.9D).
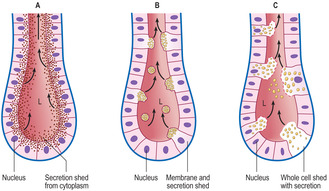
Exocrine glands synthesise their secretory products and may store them in membrane-bound structures. Secretions are released from the cells by three mechanisms:
■ merocrine secretion (Fig. 3.10A) involves exocytosis (Chapter 2) of the product, which is typically protein based, and constitutes the commonest arrangement; the pancreas secretes pancreatic enzymes by this method
■ apocrine secretion (Fig. 3.10B) involves the release of membrane-bound vesicles of secretory product from the apex of the cell; this arrangement is associated, mainly, with lipid-based products as secreted by some sweat glands and the modified sweat glands that form the mammary glands
■ holocrine secretion (Fig. 3.10C) involves the breakdown and release of the contents of the whole cell; sebaceous glands of skin utilise this mode of secretion (Chapter 7).
Release of secretion from exocrine glands may be enhanced by nervous or hormonal stimuli acting on specialised cells known as myoepithelial cells. These specialised epithelial cells surround the secretory units (e.g. acini) and they contain contractile proteins similar to those in muscle cells. Under nervous or hormonal stimulation, the contractile proteins in myoepithelial cells contract and this applies pressure to the secretory units and helps to expel their secretions.
Recognising epithelia, other primary tissues and organs
If cells are lining or covering a surface it will give the first clue as to whether these are epithelial cells forming an epithelium. To categorise the type of epithelium, the number of layers of cells and the shape of the cells must be determined and this is easier at higher magnifications at which it is usually possible to identify individual cell nuclei and their cytoplasm.
Connective tissue connects the basement membranes of epithelia to other structures and is thus readily recognised if an epithelium has been identified.
■ In skin, the epithelium (epidermis) is adjacent to the connective tissue of the dermis (Fig. 3.7).
■ In many tubes, e.g. of the digestive (Fig. 3.4), respiratory (Fig. 3.5), reproductive (Fig. 3.6) and urinary (Fig. 3.8) systems, the epithelia and basement membranes are adjacent to connective tissue (known as the lamina propria). The epithelium, basement membrane and connective tissue lamina propria together are described as a mucous membrane (a mucosa). The epithelial surfaces of such structures are kept moist by glandular secretions which are usually mucus or, in the case of the urinary tract, by urine. In addition, smooth muscle (the muscularis mucosae) lies deep to the mucosa of some of these tubes.
■ In blood vessels, the squamous epithelium (endothelium) is adjacent to connective tissue (Fig. 3.2) and, in some vessels, smooth muscle cells are also in close proximity.
Connective tissue occurs in regions other than adjacent to epithelia; further details which aid recognising primary tissues, other than epithelia, are given in Chapter 4, Chapter 5 and Chapter 6.
Recognising organs relies on determining the primary tissues present and their arrangement. The liver is a multifunctional organ in which epithelial gland cells (hepatocytes) make up the majority of the organ, the parenchyma (Figs 3.3 and 3.11). Connective tissue (known as stroma) is also present and it provides support for, and connects, the hepatocytes, blood vessels and ducts in the gland. Knowing the normal arrangement of the cells and tissues in an organ is essential before being able to decide whether abnormalities are present.
Tumours Many tumours in humans arise from epithelial cells undergoing abnormally high levels of cell proliferation when new cells produced by mitosis exceed the rate at which cells are lost. If the new growth of epithelial cells remains localised, it forms a benign tumour; if the new epithelial cells penetrate the basement membrane, the growth is malignant and known as a carcinoma. It is only after this invasion through the basement membrane has occurred that cancerous cells can spread to distant sites in the process known as metastasis. The extent to which cancerous epithelial cells have penetrated their basement membrane and have changed their appearance is used to judge the invasiveness of the tumour.
Epithelial tissue consists of epithelial cells attached to each other:
■ A simple epithelium has a single layer of epithelial cells and each is attached to the basement membrane.
■ A compound (stratified) epithelium has several layers of epithelial cells and only those in the basal layer are attached to the basement membrane.
■ Epithelial cells line or cover structures in the body, form some membranes and form glands which secrete a variety of molecules:
■ exocrine glands discharge their secretions onto surfaces
■ endocrine glands discharge their secretions into blood vessels
■ paracrine and unicellular glands discharge their secretions in their local area.
Epithelial tissue has a variety of functions, reflected in its structure:
■ secretion
■ absorption
■ modulation of permeability to molecules
■ physical protection
■ detection of some sensations.