Primary Mandibular Deficiency Growth Patterns with or without Maxillary Arch Constriction
• Treatment Indications and Objectives
• The Role of Growth Modification in the Preadolescent Child
• Orthodontic Camouflage Approach
• Postsurgical Orthodontic Maintenance and Detailing
• Complications, Informed Consent, and Patient Education
• Temporomandibular Disorders: The Effects of Orthodontics and Orthognathic Surgery
The surgical correction of the underdeveloped mandible was first reported in the American literature by Vilray P. Blair in the Journal of the American Medical Association in July 1909.7 Dr. Blair presented two cases of retrognathia in which a horizontal ramus osteotomy was performed on each side of the mandible. The operative technique was carried out through a preauricular stab incision; an aneurysm needle was introduced posteriorly to the neck of the condyle and directed medially around to the ascending ramus, where it then exited through the cheek in front of the anterior border of the ramus. A Gigli saw was then put in place and blindly used to complete an osteotomy. The same procedure was completed on the opposite side of the jaw, and then the mandible was advanced into the desired occlusion. Intermaxillary fixation was applied until a callus formed. As a result of the limited bone contact across the osteotomy sites, a strong relapse tendency required persistent counterforces with continued intermaxillary elastics. Extrusion of the incisors with periodontal sequelae and recurrent malocclusion was a frequent observation.
Mandibular deficiency is the most prevalent form of dentofacial deformity.2,30,32,39,43 It is more common among Caucasians than Africans or Asians, which suggests that a hereditary component is a predominant part of the etiology. During the mid 1970s, the public health service of the U.S. Department of Health, Education, and Welfare conducted an assessment of the occlusions of children who were 6 to 11 years old and 12 to 17 years old. These collected data indicated that approximately 20% of the sample populations had an Angle Class II malocclusion. Unfortunately, no other means of evaluation were performed to separate those children with a Class II jaw disharmony from those with a more straightforward dental Class II malocclusion. According to a National Health and Nutrition Examination Survey, severe mandibular deficiency (defined as >7 mm of positive overjet) in the U.S. Caucasian population has a prevalence of approximately 10%.43 This pattern of Class II excess overjet is less frequent among African-American and Mexican-American groups. It can be assumed that more than 7 mm of overjet indicates a jaw discrepancy of such magnitude that orthognathic surgery would be the preferred way to manage the problem. The majority of these patients will have dentofacial deformities that fall into the categories of a long face growth pattern, maxillomandibular deficiency, or primary mandibular deficiency with or without arch-width discrepancy.
Functional Aspects
• Articulation errors during speech and swallowing difficulties that result from the Class II malocclusion are expected (see Chapter 8).
• Difficulties with chewing and with lateral and protrusive mandibular movements as a result of the Class II malocclusion are also expected.
• Upper airway obstruction during sleep often exists as a result of the retropositioned tongue. Obstructive sleep apnea should be ruled out (see Chapter 26).
• Detrimental long-term effects on the dentition and the periodontium as a result of the crowding of the mandibular teeth in limited alveolar housing or from previous camouflage orthodontic treatments are often seen (see Chapters 5 and 6).
• A higher incidence of temporomandibular disorders that result from mandibular deficiency Class II malocclusion have been reported (see Chapters 9 and 36).
Clinical Characteristics
• The lower lip is curled and everted, and it is often wedged behind the incisors with an accentuated labiomental fold. The shorter the lower anterior facial height, the greater the tendency for an accentuated labiomental fold.
• The gonial angles of the mandible tend to be relatively square. The shorter the face and the deeper the bite, the more acute the angles.
• There is a retruded and weak chin with a convex profile.
• There is a deficient mandible with the illusion of a large nose.
• There is a short chin-to-neck length and an obtuse angle, often with a double chin (even in a thin individual).
Dental Findings
• There are varied degrees of increased overjet with a Class II molar and canine relationship.
• The crowding of the teeth within the lower arch (i.e., the smaller the mandible, the greater the crowding) needs to be evaluated, and so does lower incisor flaring. Mandibular dental compensations often mask the true skeletal discrepancy.
• There are varied degrees of dental compensation in the upper jaw with either procumbency (i.e., “buck teeth”) or maxillary incisors that are retroclined.
• The anterior deep bite (i.e., excessive overbite) may involve impingement of the anterior maxillary palatal tissues by the mandibular incisors.
• There is an excessive curve of Spee in the mandible (i.e., the deeper the anterior bite, the greater the excess curve).
• A reduced or negative curve of Spee is found in the maxillary arch.
• Dental crowding may also be seen in the maxilla (i.e., the more constricted the maxilla, the greater the crowding).
• Excessive wear facets, cusp fractures, and significant restorations in the posterior dentition are frequent findings in adults.
• Accelerated loss of the periodontium associated with the maxillary incisors (due to traumatic occlusion or previous orthodontics); the maxillary molars (due to arch constriction or previous orthodontics); and the mandibular incisors (due to supraeruption and anterior flaring from previous orthodontics) may be seen in adults.
Radiographic Findings
• Horizontal retrusion is measurable at the B-point of the mandible.
• The A-point–nasion–B-point angle is generally increased as a result of the retrusive lower jaw.
• Excessive procumbency of the mandibular incisors is frequently measurable.
• A vertically short and retrusive chin is generally measurable.
• The maxillary incisors are often procumbent, but they may be retropositioned as a result of previous extractions and camouflage orthodontics.
Treatment Indications and Objectives
The individual’s immediate aesthetic concerns often center on 1) unfavorable lower-lip contours (e.g., a curled and everted lower lip with an accentuated labiomental fold) 2) a lack of prominence of the chin (e.g., a weak profile) and 3) an unattractive neck (e.g., a soft-tissue double-chin tendency).27,38,39,42,48,47,50,59 Functional issues are also to be expected. For example, when the anterior bite is “deep,” it will cause irritation of the gingival tissues of the palate just behind the maxillary incisors. Partial obstruction of the upper airway as a result of a retropositioned tongue is also common (i.e., heavy snoring, restless sleep, daytime fatigue, and documented or undiagnosed sleep apnea; see Chapter 26).11,62 Complaints of an uncomfortable “dual” bite, chewing difficulties, masticatory muscle discomfort, and audible speech articulation errors are frequent. The individual with a Class II deep bite may have a greater tendency toward clicking (i.e., anterior disc displacement) in each temporomandibular joint.25,51 Interestingly, there is little scientific evidence to support the notion that the signs of clicking will into more significant temporomandibular joint pathology (see Chapter 9).
The Role of Growth Modification in the Preadolescent Child
When the preadolescent child with mandibular deficiency is identified, a growth modification approach to treatment is frequently considered by the evaluating orthodontist.13,33,32 Cozza and colleagues completed a systematic review of the literature to assess the efficacy of functional appliance use for enhancing mandibular growth in subjects with Class II malocclusions.14 With the use of the Medline database, the survey covered the period from January 1966 to January 2005. A review of 704 articles confirmed only 22 that qualified for the final analysis. Of these 22 articles, only four randomized clinical trials were retrieved and found to be worthy of inclusion. Interestingly, none of these four trials reported a clinically significant change in mandibular length to be induced by functional appliances in the patients with Class II deformities. According to Proffit, the only concrete indications for the treatment of the preadolescent mixed dentition child with a mandibular deficiency who presents without an anterior open bite are the following44:
• Significant trauma to the palatal tissue (i.e., the lower incisors are injuring the palatal mucosa) or other indications of potential irreversible tissue damage
• Special concerns about the effects of the condition on the child’s psychological well-being and the strong belief that the recommended treatment will alter this in a positive way
• Skeletal maturation that is well ahead of dental development so that the adolescent growth spurt occurs before the mixed dentition ends
1. The alignment of the upper incisors (i.e., the correction of lingual tipping with a Class II, Division 2 malocclusion) to prevent any interference with the forward movement of the mandible.
2. Attempts to impede the biologic programmed forward growth of the maxilla and to facilitate the forward growth of the mandible. Extraoral (posterior vectored) compressive forces are typically applied to the maxilla through a headgear device.
3. Attempts to stimulate the mandibular posterior teeth to hypererupt while preventing the incisors from doing so. During this process, it is hoped that the deep overbite will improve. An intra-oral functional appliance is often designed to facilitate these events.
Orthodontic Camouflage Approach
When the orthodontist proceeds with growth modification maneuvers and a less than favorable biologic response is realized, it is apparently tempting to proceed with a camouflage (dental compensation) approach (Figs. 19-1 through 19-5).34,35,37,36,42 This would be carried out to “neutralize” the occlusion rather than to position the teeth solidly into the alveolar process in combination with orthognathic surgery. Current evidence-based medical standards recommend that the treating orthodontist have a “timeout” (i.e., a sit-down discussion and reassessment with the parents and the patient) that includes a review of the records (e.g., photos, models, radiographs) and a discussion of the biologic effects on the airway, the facial aesthetics, the occlusal stability, and the periodontium that may result from the various treatment options. A referral to an experienced orthognathic surgeon for the discussion of possible future surgical aspects is highly recommended.


Figure 19-1 A 20-year-old man with a primary mandibular deficiency growth pattern requested a surgical consultation for a weak chin. During his early teenage years, the patient underwent growth modification in an attempt to stimulate the forward projection of the mandible. This was followed by an orthodontic camouflage approach that included maxillary first bicuspid extractions to retract the anterior teeth. In addition, the mandibular anterior dentition was flared forward. His history was significant for heavy snoring, restless sleeping, and a degree of daytime fatigue, all of which are suggestive of obstructive sleep apnea. Examination confirmed a retrognathic mandible with a molar Class II deep-bite malocclusion. The mandibular incisors were crowded and procumbent. The family had hoped that a chin implant would be effective to manage the aesthetic effects. A sleep study was recommended, and an orthognathic approach with redo orthodontic treatment including lower bicuspid extractions was suggested as the preferred method to improve the airway, to achieve long-term dental health, and to enhance facial aesthetics. A, Frontal facial and occlusal views. B, Profile facial view and lateral cephalometric radiograph.


Figure 19-2 A 21-year-old woman with a primary mandibular deficiency growth pattern requested a surgical consultation for a weak chin. During her early teenage years, the patient underwent growth modification in an attempt to stimulate the forward projection of the mandible. This was followed by an orthodontic camouflage approach. The mandibular anterior dentition was flared forward. Her history was significant for restless sleeping and a degree of daytime fatigue, which are suggestive of obstructive sleep apnea. Examination confirmed a retrognathic mandible with a Class II malocclusion. The mandibular incisors were crowded and procumbent. The family had hoped that a chin implant would be effective to manage the aesthetic effects. A sleep study confirmed obstructive sleep apnea (respiratory disturbance index = 18/hour). An orthognathic approach with redo orthodontic treatment including lower bicuspid extractions was recommended as the preferred method to improve the airway, to achieve long-term dental health, and to enhance facial aesthetics. A, Frontal facial and occlusal views. B, Profile facial view and lateral cephalometric radiograph.
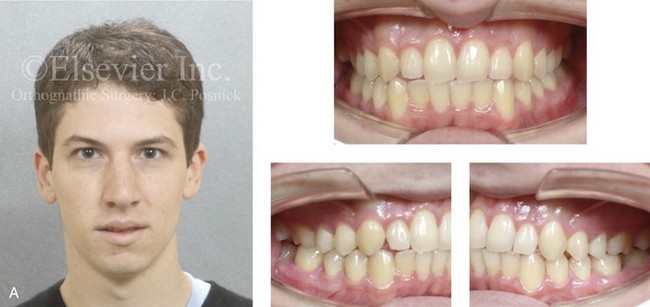

Figure 19-3 A 20-year-old man with a primary mandibular deficiency growth pattern requested a surgical consultation for a weak chin. During his the early teenage years, the patient underwent growth modification in an attempt to stimulate the forward projection of the mandible. This was followed by an orthodontic camouflage approach. The mandibular anterior dentition was flared forward. The patient’s history was significant for heavy snoring, restless sleeping, and a degree of daytime fatigue, all of which are suggestive of obstructive sleep apnea. Examination confirmed a retrognathic mandible with clockwise rotation of the maxillomandibular complex. The mandibular incisors were crowded and procumbent. He had hoped that a chin implant would be effective to manage the aesthetic effects. An orthognathic approach with redo orthodontic treatment including lower bicuspid extractions was recommended as the preferred method to improve the airway, to achieve long-term dental health, and to enhance facial aesthetics. A, Frontal facial and occlusal views. B, Profile facial view and lateral cephalometric radiograph.

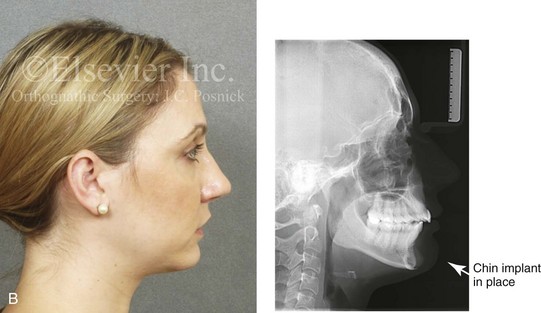
Figure 19-4 A 29-year-old women arrived to discuss chin aesthetics. During the mixed dentition, she was recognized as having mandibular deficiency and a constricted maxillary arch width. At that time, she underwent growth modification techniques that included headgear. She also underwent rapid palatal expansion followed by compensatory orthodontic mechanics to neutralize the occlusion, but this also involved proclination of the incisors. A retrusive profile and a dual bite remained. The patient had recently undergone the placement of a chin implant without fixation. Aesthetic modification of the anterior maxillary dentition was also completed. The patient was displeased with the cosmetic results of a deepened labiomental fold, a mobile chin implant, and a “button” appearance during lip closure. There is a dual bite with Class II malocclusion when the teeth are in centric relation. A, Oblique and frontal facial views. B, Profile facial view and lateral cephalometric radiograph 6 months after chin implant placement.


Figure 19-5 A 43-year-old woman arrived to discuss the aesthetics of her weak chin and premature facial aging. During her late mixed dentition, she was recognized as having mandibular deficiency with a Class II malocclusion. At that time, she underwent growth modification techniques followed by compensatory orthodontic mechanics. This included upper first bicuspid extractions, the retraction of the anterior maxillary teeth, and the proclination of the mandibular incisors, all in an attempt to neutralize the occlusion. A retrusive profile and a dual bite remained. The weak profile of her adolescence had progressed into premature facial aging. She also had a lifelong history of obstructed nasal breathing, restless sleeping, and excessive daytime fatigue, all of which are suggestive of obstructive sleep apnea. An orthognathic approach with redo orthodontic treatment including lower bicuspid extractions was recommended as the preferred method to improve the airway, to achieve long-term dental health, and to enhance facial aesthetics. A, Frontal facial and occlusal views. B, Profile facial view and lateral cephalometric radiograph.
An orthodontic camouflage approach for the individual with mandibular deficiency may take the form of maxillary premolar extractions so that the upper incisors can be retracted. This is generally combined with the flaring of the mandibular incisors. When this is carried out in the individual with a mandibular deficiency, the short-term objective of a neutralized occlusion may be achieved, but the following are potential sequelae: 1) unfavorable long-term facial aging 2) the risk for obstructive sleep apnea later in life 3) long-term periodontal deterioration 4) lower anterior crowding with recurrent malocclusion and 5) an inconsistent occlusion (i.e., a dual bite) (see Figs. 19-1 through 19-5). The orthodontist may feel favorable toward a camouflage approach on the basis of the belief that the patient can always have a “chin implant” to improve his or her facial aesthetics. Unfortunately, this approach will rarely achieve a pleasing aesthetic outcome. A chin implant tends to result in 1) an accentuated labiomental fold 2) an overly prominent pogonion and 3) a residual obtuse neck–jaw angle (Fig. 19-4). Furthermore, it does nothing for any baseline masticatory and airway dysfunction (see Chapter 37).
Definitive Reconstruction
Timing of Orthognathic Surgery
Stahl and colleagues carried out a longitudinal study to compare the biologic jaw growth changes of untreated subjects with Class II, Division 1 malocclusions as compared with those subjects with a normal Class I occlusion.55 Each subject was followed from the prepubertal stage through the postpubertal stage of development. The study provides evidence of a similar growth pattern in both Class II and Class I subjects. The absolute amount of mandibular lengthening at the pubertal peak was significantly smaller in the Class II subjects than in those with normal occlusion. A significant deficiency was measured in overall mandibular length (i.e., Condyle-Gonion [Co-Gn]) in the Class II malocclusion subjects at the completion of growth. Interestingly, the authors’ findings show that a Class II dentofacial disharmony does not have a tendency to self-correct with growth.
There are numerous reports in the literature of surgeons carrying out successful orthognathic corrections in patients with mandibular deficiencies who are between the ages of 13 and 15 years. This is before the age at which growth maturity is typically considered to be complete. Interestingly, after the patient with a mandibular deficiency has undergone successful surgical correction, there are no reports late mandibular catch up growth.5,20,23,29,45,52,61
A review of available research data and clinical reports indicated that, when orthognathic surgery was undertaken in the patient with a mandibular deficiency as early as the completion of the adolescent growth spurt, further significant forward growth of the mandible almost never occurred.31,55 Further horizontal growth of the maxilla at this age is also not expected. In theory, limited vertical growth of both the mandible and maxilla may continue; however, if it does, it tends to be proportionate. Proceeding with definitive orthognathic surgery in the patient with a mandibular deficiency as early as the age of 13 or 14 years—but only after the eruption and orthodontic alignment of the teeth—is generally safe from a growth perspective.
Periodontal Considerations before Orthodontic Treatment
The position of the mandibular incisors in the alveolar housing has important periodontal consequences (see Chapter 6). In the retrognathic patient, the more the mandibular incisors are orthodontically tipped forward, the greater the chance of labial bone loss and gingival recession. There should be a healthy band of attached gingiva at the beginning of treatment and flaring of the incisors is to be avoided. This is a frequent concern in borderline crowding cases, when the final decision is made to not extract and then further labial tipping of the incisors occurs.
Even after successful gingival grafting, if further incisor flaring is allowed to occur in the presence of deficient labial bone, negative periodontal sequelae are to be expected. For patients with borderline crowding, if the incisor crowns are morphologically large, the judicious use of interproximal reduction may create the needed space to uncrowd the arch and to simultaneously upright the teeth (see Chapter 17).
Orthodontic Preparation for Orthognathic Surgery
When the deficient mandible is surgically advanced and vertically lengthened to achieve a more ideal overbite and overjet, the relative widening of the mandibular arch in the molar region occurs. Maxillary arch expansion may then be required to correct posterior crossbites. If more than several millimeters is required, then simultaneous surgical arch expansion of the maxilla through segmental Le Fort I osteotomy is the preferred approach (see Chapter 17).
• Recognizing the need for extractions in the mandible and incorporating this information into the treatment plan from the beginning
• Recognizing the need for the surgical expansion of the upper arch (consider incorporating Le Fort I segmental osteotomies to widen the arch into the treatment plan from the beginning; see Chapter 17)
• Aligning the teeth independently within each arch with the objective of a compatible postsurgical occlusion
• Establishing the preferred sagittal and vertical positions of the incisors in the alveolar bone so that the jaw reconstruction that follows will result in enhanced facial aesthetics and improved head and neck function.
• To manage an excessive curve of Spee in the lower arch, a majority of the leveling will be done after jaw surgery via the extrusion of the premolars.
• If the mandibular arch is fully leveled before surgery, then the bicuspid extraction spaces should also be closed before surgery.
• If a degree of lower arch leveling is to be accomplished after jaw surgery, then it is desirable to leave some of the bicuspid extraction space to be closed postoperatively.
• Passive surgical arch wires to be used for stabilization during surgery should be full-dimensional and rectangular.
• With effective plate and screw fixation at each osteotomy site, continuous intermaxillary fixation after surgery is not warranted. Nevertheless, the orthodontic placement of stable hooks throughout the arch wires is useful both at the time of surgery and to accomplish supportive vectored elastics postoperatively.
Immediate Presurgical Planning
First, broad-stroke decisions are made regarding preferred vector changes for each jaw; only then are the precise millimeter distances and angular changes that are required in each jaw to achieve the desired result determined (see Chapter 12).3,4,17,42 Analytic model planning is carried out on the articulated dental casts with use of the Erickson Model Table. Splints are constructed to assist with the achievement of the precise occlusion and the preferred facial aesthetics in the operating room (see Chapter 13).
During surgical planning for the individual with a primary mandibular deficiency growth pattern, it is known that bilateral sagittal split ramus osteotomies with advancement into a corrected overbite and overjet position will be required (Figs. 19-6 through 19-9).6,21 An important consideration is whether or not surgical repositioning of the upper jaw (i.e., Le Fort I osteotomy) will also be useful to correct arch-width discrepancies; to further adjust the horizontal and vertical position of the maxilla; and to alter the maxillary plane (i.e., pitch orientation) and cant (i.e., roll orientation) (Figs. 19-10 through 19-15).3,4,15,18,41,40,46,49,60 An assessment of the baseline chin morphology is also important. Anticipating the location of the pogonion after jaw repositioning and considering the advantage of an osseous genioplasty to achieve an enhanced horizontal and vertical position of the chin are important (see Chapter 37).
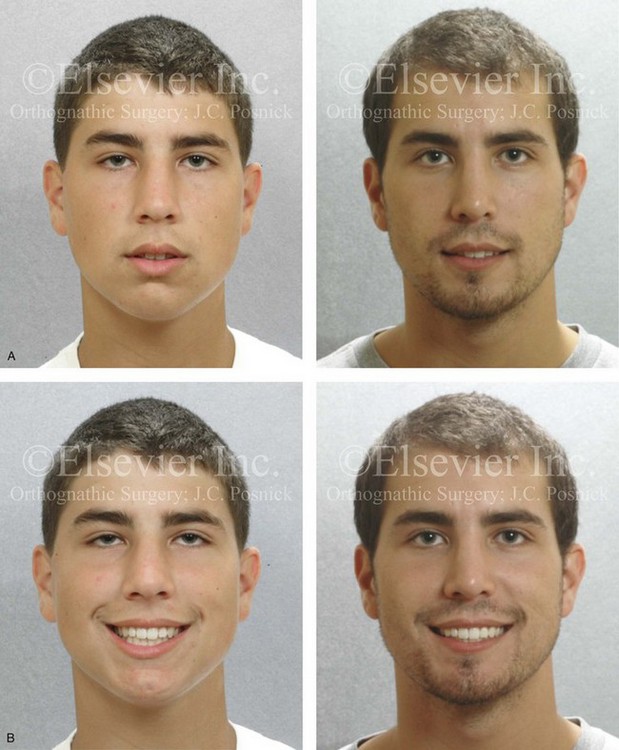
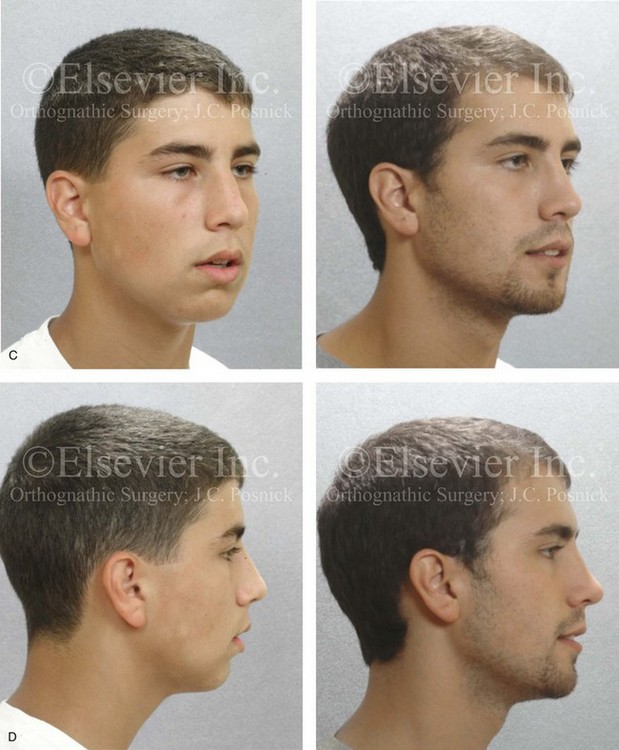
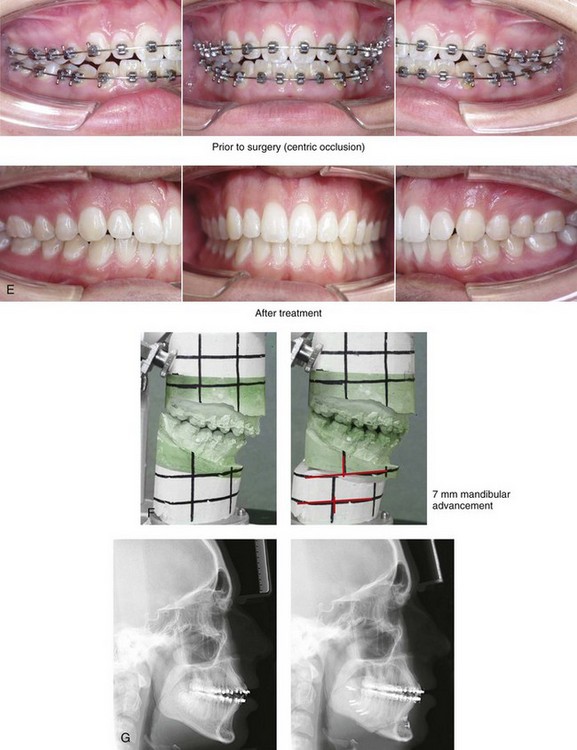
Figure 19-6 A 15-year-old boy with mandibular deficiency and microgenia underwent a combined orthodontic and surgical approach. The procedures included bilateral sagittal split ramus osteotomies (horizontal advancement) and an osseous genioplasty (horizontal advancement). One year later, he underwent a septorhinoplasty procedure to open the airway and to enhance nasal aesthetics. He is shown before and 5 years after reconstruction. A, Frontal view in repose before and 5 years after reconstruction. B, Frontal views with smile before and 5 years after reconstruction. C, Oblique facial views before and 5 years after reconstruction. D, Profile views before and 5 years after reconstruction. E, Occlusal views with orthodontics in progress (centric occlusal) and 5 years after treatment. F, Articulated dental casts before (centric relation) and after model planning. G, Lateral cephalometric radiographs before and after reconstruction.


Figure 19-7 A 15-year-old girl with mandibular deficiency and microgenia underwent a combined orthodontic and surgical approach. The surgery included bilateral sagittal split ramus osteotomies (horizontal advancement) and an osseous genioplasty (horizontal advancement). A, Frontal view in repose before and after reconstruction. B, Oblique facial views before and after reconstruction. C, Profile views before and after reconstruction. D, Occlusal views before and after the completion of treatment. E, Articulated dental casts that indicate analytic model planning. F, Lateral cephalometric radiographs before and after treatment.


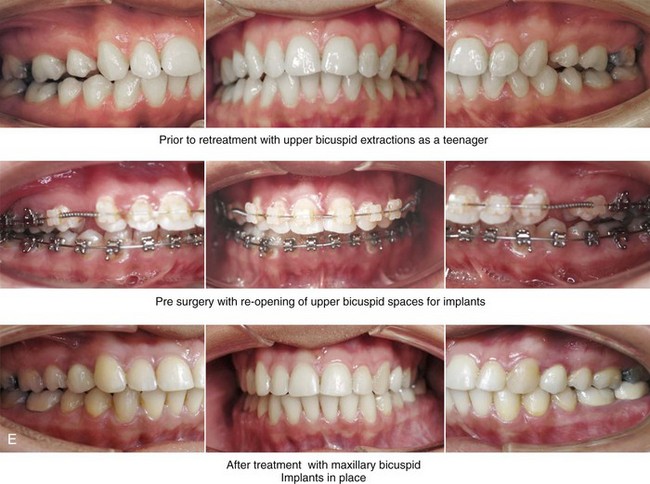
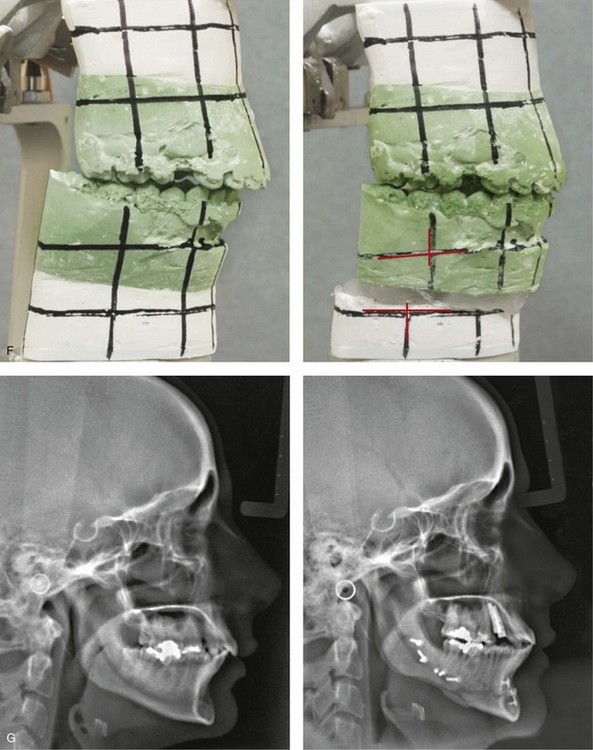
Figure 19-8 A woman in her late 20s was referred by an orthodontist for surgical evaluation. During her high school years, the patient underwent maxillary first bicuspid extractions with orthodontic retraction to neutralize the occlusion in the presence of mandibular deficiency. She now hoped to improve her profile aesthetics and to achieve long-term dental health. The patient agreed to an orthodontic and surgical approach. Orthodontic (dental) decompensation required opening the maxillary bicuspid extraction spaces for dental implants and crowns. The mandibular arch was also decompensated. The patient then underwent surgery that included bilateral sagittal split ramus osteotomies (horizontal advancement); osseous genioplasty (horizontal advancement); and an anterior approach to the soft tissues of the neck (cervical flap elevation, neck defatting, and vertical platysma muscle plication). A, Frontal views in response before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views before retreatment, with orthodontic decompression in progress, and then after treatment. F, Articulated dental casts indicating analytic model planning. G, Lateral cephalometric radiographs before and after reconstruction.
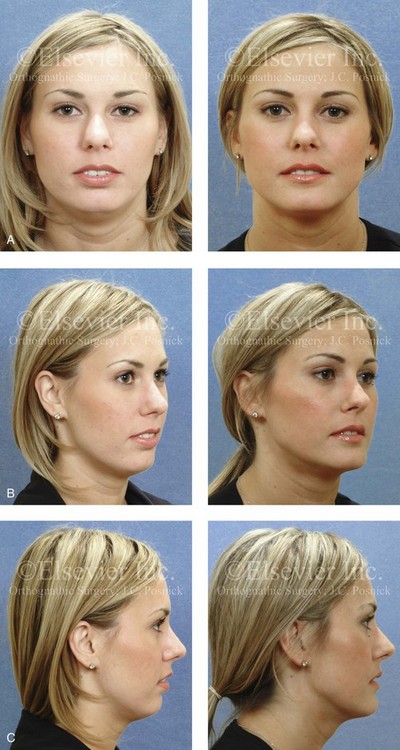

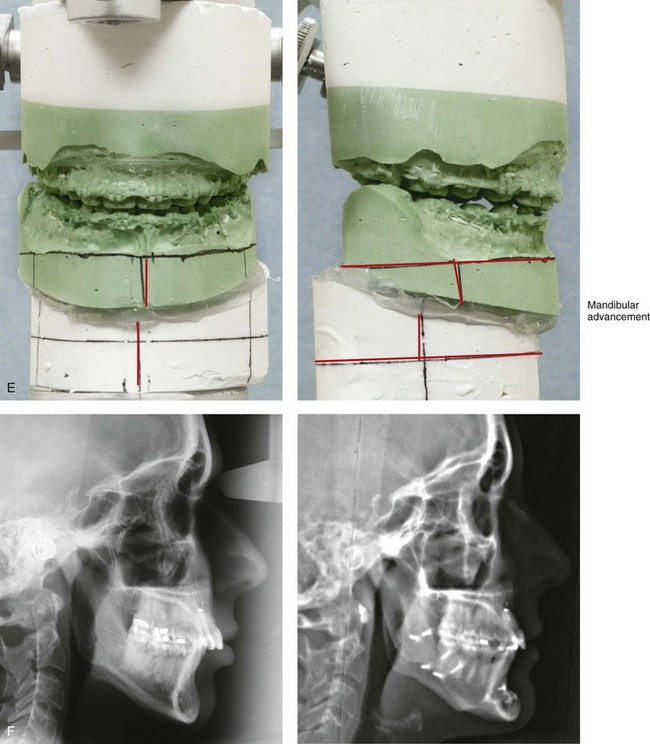
Figure 19-9 A woman in her late 20s was referred by an orthodontist for surgical evaluation. During her teenage years, she underwent camouflage orthodontics to neutralize the occlusion, including maxillary first bicuspid extractions with space closure. She arrived for evaluation to improve the occlusion and to achieve enhanced profile aesthetics. She agreed to an orthodontic and surgical approach. Orthodontic (dental) decompensation required the proclination of the maxillary anterior dentition and mandibular first bicuspid extractions with the retraction of the anterior dentition. This was followed by surgery that included bilateral sagittal split osteotomies of the mandible (horizontal advancement); osseous genioplasty (horizontal advancement); and an anterior approach to the soft tissues of the neck (cervical flap elevation and neck defatting). A, Frontal views in repose before and after reconstruction. B, Oblique facial views before and after reconstruction. C, Profile views before and after reconstruction. D, Occlusal views early during orthodontic retreatment, before surgery, and after reconstruction. E, Articulated dental casts indicating analytic model planning. F, Lateral cephalometric radiographs before and after treatment.


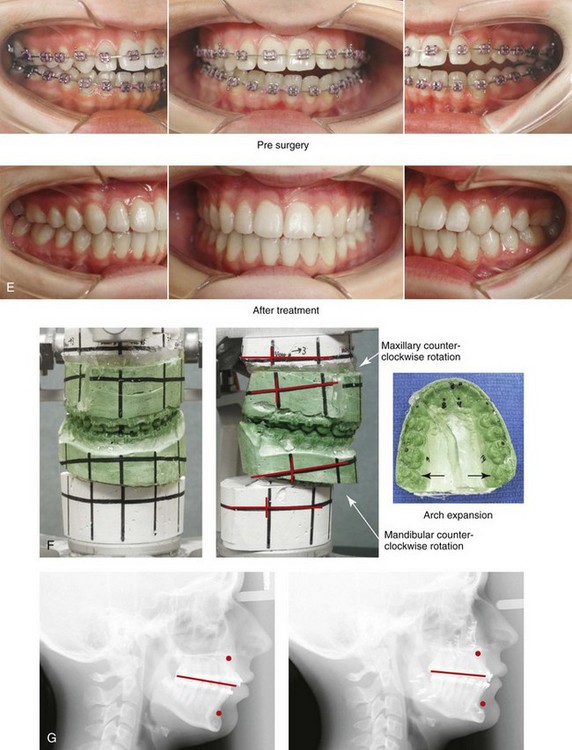
Figure 19-10 A teenaged girl was referred by her orthodontist for surgical assessment. She had a primary mandibular deficiency and maxillary arch constriction. She also had a Class II anterior open-bite malocclusion. A comprehensive orthodontic and surgical approach was selected. No extractions were required. Her surgery included a Le Fort I osteotomy in two segments (transverse widening, horizontal advancement, and counterclockwise rotation); bilateral sagittal split osteotomies of the mandible (horizontal advancement and counterclockwise rotation); and osseous genioplasty (horizontal advancement). A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views during orthodontic decompensation and after treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after reconstruction.


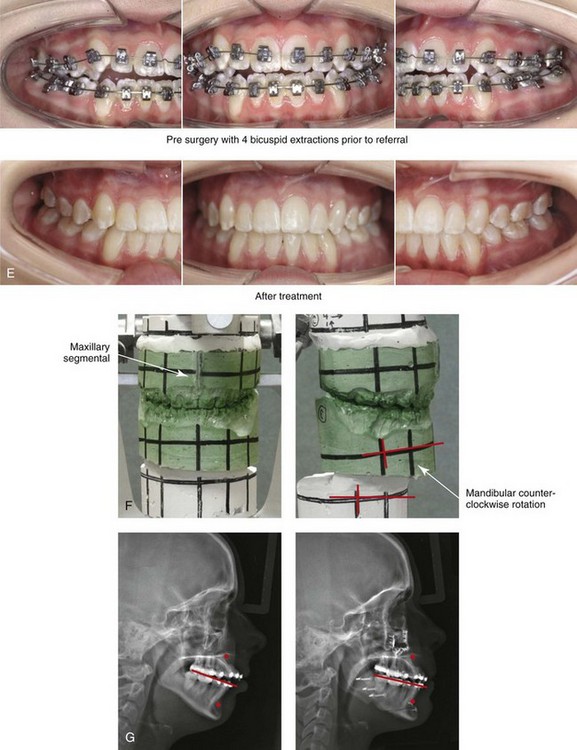
Figure 19-11 A 16-year-old girl was referred for surgical assessment only after orthodontic treatment was well under way. She had undergone four bicuspid extractions and compensating orthodontics, but these were unsuccessful with regard to the neutralization of the occlusion. She was then recognized as having mandibular deficiency with a significant overjet, an anterior open bite, and obstructed nasal breathing. A degree of gingival recession on the labial aspect of the lower canines was appreciated. The maxillary incisors were procumbent but without space for further retraction. Reconstruction included a Le Fort I osteotomy in segments (horizontal advancement and transverse widening); bilateral sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (horizontal advancement); and septoplasty and inferior turbinate reduction. The patient’s gingival recession which was present prior to surgery is being monitored. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before surgery and after reconstruction. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.


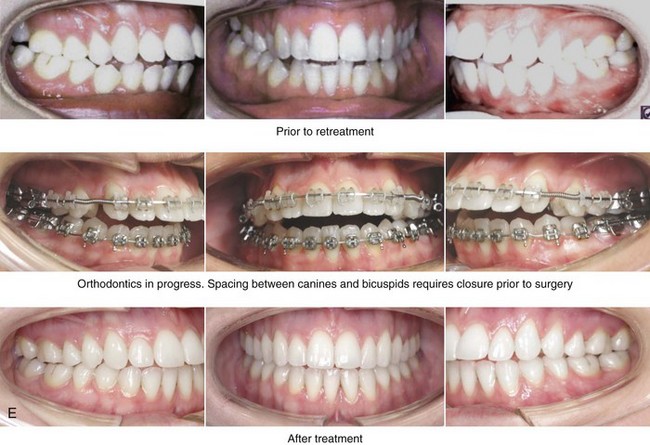
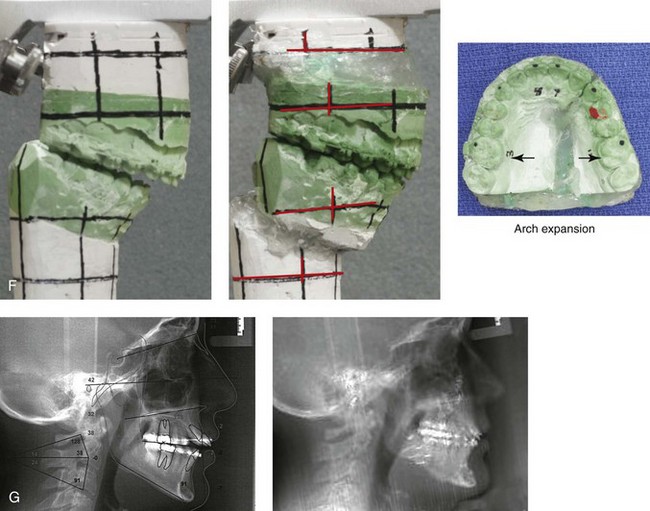
Figure 19-12 A 30-year-old woman was referred for surgical assessment only after orthodontic treatment was well under way. When the patient was between 9 and 15 years old, orthodontic growth modification and then a camouflage approach were carried out, but these were not successful. The current orthodontic treatment was flaring the maxillary anteriors even further forward. The patient was referred to this surgeon and agreed to a combined surgical and orthodontic approach. Orthodontic retraction of the maxillary anteriors was then initiated. With sufficient orthodontic (dental) decompensation, surgery was carried out, including bilateral sagittal split osteotomies of the mandible (horizontal advancement and counterclockwise rotation); maxillary Le Fort I osteotomy in segments (arch expansion, horizontal advancement, and minimal counterclockwise rotation); osseous genioplasty (horizontal advancement); and an anterior approach to the soft tissues of the neck (cervical flap elevation, neck defatting, and vertical platysma muscle plication). A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment, with orthodontics in progress, and after the completion of treatment. Note the early gingival recession of the maxillary canine and bicuspid teeth as a result of orthodontic mechanics. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.



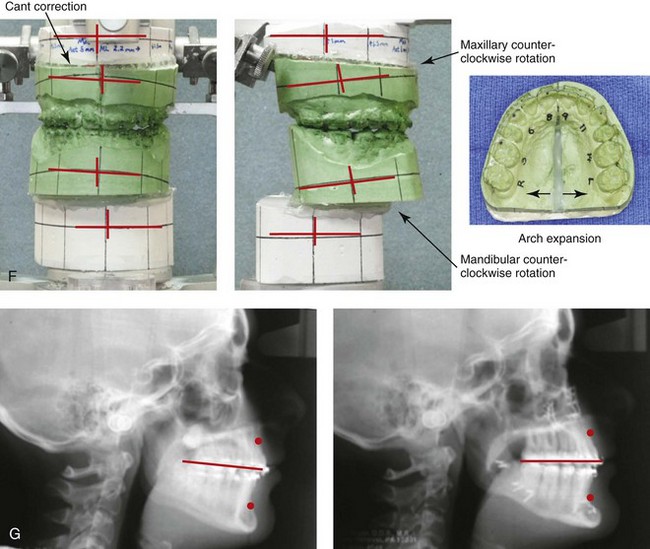
Figure 19-13 A 15-year-old girl was referred for surgical evaluation only after orthodontic treatment was well under way. She has primary mandibular deficiency with maxillary arch construction. There is a Class II negative overjet malocclusion despite four bicuspid extractions. The patient agreed to an orthodontic and surgical approach. After orthodontic (dental) decompensation, she underwent surgery that included a maxillary Le Fort I osteotomy in segments (horizontal advancement, counterclockwise rotation, transverse expansion, and cant correction); bilateral sagittal split osteotomies of the mandible (horizontal advancement, counterclockwise rotation, and asymmetry correction); and osseous genioplasty (horizontal advancement). A, Frontal views in repose before and 3 years after treatment. B, Frontal views with smile before and 3 years after treatment. C, Oblique facial views before and 3 years after treatment. D, Profile views before and 3 years after treatment. E, Occlusal views before treatment, with orthodontics in progress, and 3 years after treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.


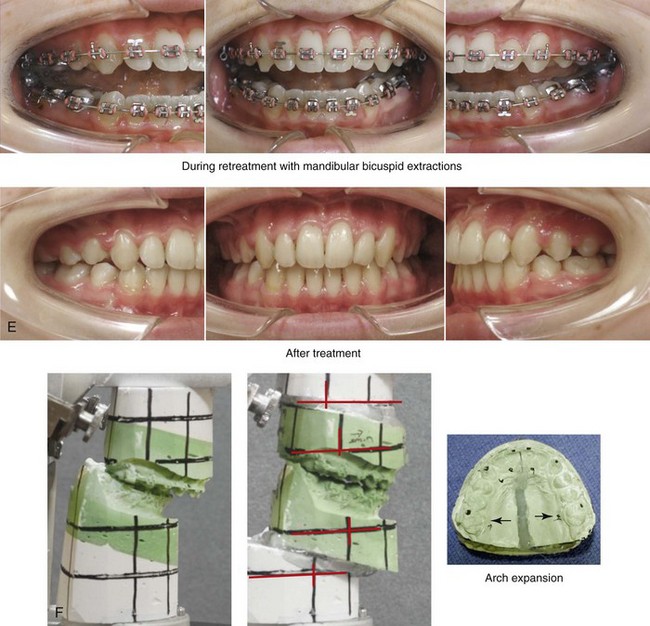
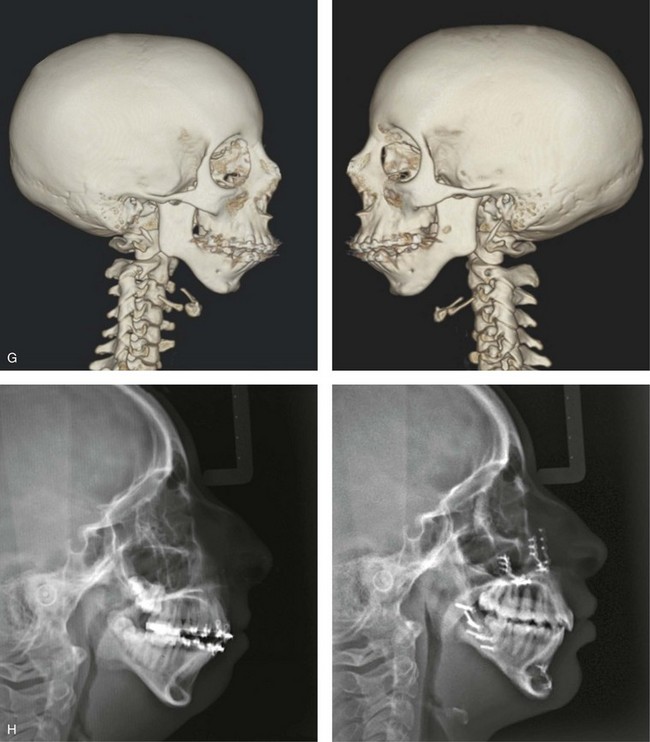
Figure 19-14 A 16-year-old girl was referred for surgical evaluation only after orthodontic treatment was well under way. Lower bicuspid extractions with the retraction of the anterior dentition were recommended for full decompensation. A computed tomography scan was obtained and confirmed congenital dysplasia of the condyle–glenoid fossa complex; however, there was a functional temporomandibular joint complex on each side. There was no suggestion of condylar resorption now or in the past. The reconstruction included a maxillary Le Fort I osteotomy in segments (arch expansion and horizontal advancement); bilateral sagittal split ramus osteotomies (horizontal advancement); osseous genioplasty (horizontal advancement); and septoplasty and inferior turbinate reduction. The patient is shown before and after treatment. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views with orthodontics in progress and after treatment. F, Articulated dental casts that indicate analytic model planning. G, Computed tomography scan views before reconstruction that indicate congenital dysplasia of the condyle–glenoid fossa complex. H, Lateral cephalometric radiographs before and after treatment.



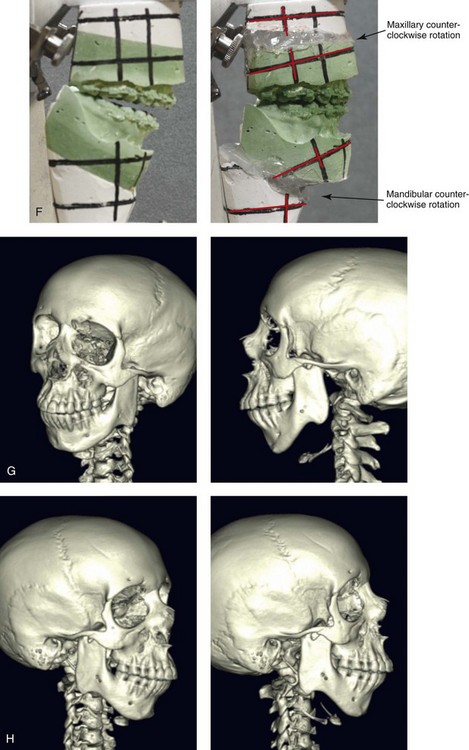
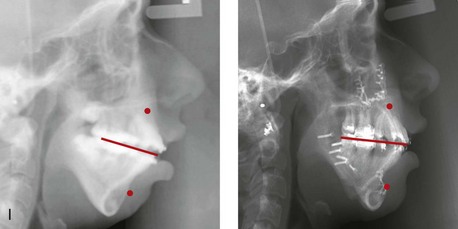
Figure 19-15 A 15-year-old girl was referred for surgical assessment only after orthodontic treatment was well under way. She had severe mandibular deficiency and microgenia, and she had already undergone four bicuspid extractions and a full course of orthodontic treatment. An anterior open bite with procumbent maxillary incisors remained. Evaluation was carried out, including a computed tomography scan, a sleep study, and speech and otolaryngology consultations. The computed tomography scan confirmed congenital dysplasia of the condyle–glenoid fossa complex without condylar resorption. Orthodontics were reinitiated, and surgical reconstruction was chosen. The surgical procedures included a maxillary Le Fort I osteotomy (horizontal advancement, vertical shortening, and counterclockwise rotation); bilateral sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); and osseous genioplasty (horizontal advancement). A mild anterior open bite has recurred, but this had been stable for several years. A review of the immediate and late postoperative cephalometric radiographs confirmed a consistent sella–nasion–B-point angle without radiographic evidence of condylar resorption (i.e., no skeletal relapse could be documented). Dental relapse in the anterior dentition was felt to be the cause of recurrent malocclusion. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment (after four bicuspid extractions), before surgery, and then after treatment. F, Articulated dental casts that indicate analytic model planning. G and H, Computed tomography scans of the maxillomandibular complex that indicate congenital condyle glenoid fossa dysplasia. I, Lateral cephalometric radiographs before and after treatment.
Basic Surgical Approach
In addition to lower jaw advancement (i.e., sagittal ramus osteotomies), maxillary surgery to correct arch-width discrepancies may be required for the individual with primary mandibular deficiency. This is generally accomplished by segmental maxillary osteotomies. Through the Le Fort I down-fracture, any needed improvement in the upper-lip-to-upper-tooth relationship can also be simultaneously carried out via the alteration of the vertical height. Any deficiencies in the horizontal position (i.e., projection) of the maxilla are also managed. The correction of a maxillary midline discrepancy (i.e., yaw), the aesthetic advantages of maxillary plane alteration (i.e., pitch), cant correction (i.e., roll), and intranasal procedures (i.e., septoplasty and inferior turbinate reduction) can also be simultaneously accomplished through the Le Fort I osteotomy (see Chapter 12).
• When the decision is made to limit surgery to the mandible and with only a minimum arch-width discrepancy, the option of narrowing the mandible (i.e., a midline symphyseal split) may be considered.
• When only borderline maxillary vertical deficiency coexists (i.e., not enough to warrant a Le Fort I osteotomy), additional surgical vertical lengthening of the chin may be incorporated to achieve an aesthetic advantage.
• When mandibular deficiency is combined with a less than ideal clockwise rotated and vertically deficient maxilla, the surgically advanced mandible (without simultaneous Le Fort I osteotomy) may not achieve the preferred profile aesthetics (i.e., there will be a suboptimal A-point to B-point relationship in profile). In borderline cases, a vertical lengthening and a limited horizontal advancement osseous genioplasty may provide the necessary degree of aesthetic compensation.
Postsurgical Orthodontic Maintenance and Detailing
If segmental maxillary osteotomies were also carried out, a prefabricated splint will have been secured to the maxillary occlusal surfaces during surgery. The orthodontist sees the patient within 24 hours of splint removal (approximately 5 weeks after surgery) and replaces the maxillary sectional arch wires with a rigid continuous arch wire. The maxillary teeth are ligated together to maintain the arch form. The use of a transpalatal appliance or a palatal plate may also be used to stabilize and maintain the arch form if significant transverse expansion was carried out.12 Close orthodontic monitoring for skeletal and dental shifts during the first 6 months after surgery is essential (see Chapter 17).1,8,9,10,16,22,26,33,54,56,63
Complications, Informed Consent, and Patient Education
The orthodontist is frequently asked to evaluate a preadolescent child who is presenting with primary mandibular deficiency. The clinician may attempt to alter nature’s events through growth modification maneuvers.53 Clinical studies now confirm limited success with a growth modification approach if the goal is to “normalize” the deficient lower jaw. The camouflage orthodontic approach that often follows may neutralize the occlusion, but it will not improve baseline upper airway dysfunction, and it will not enhance the appearance of a retrusive profile. Furthermore, it may have detrimental effects on the periodontium (see Figs. 19-1 through 19-5). The onus is on the clinician to communicate the shortcomings of these isolated orthodontic maneuvers to the patient and the family before beginning treatment.
After a combined surgical and orthodontic approach is agreed to, the clinician’s ability to communicate the potential risks, complications, and benefits of the recommended coordinated plan to the patient and the family is essential (see Chapter 17).19,24 The patient’s and the family’s informed decision to proceed provides the basis for shared responsibility of the outcome (see Chapter 7).
Temporomandibular Disorders: The Effects of Orthodontics and Orthognathic Surgery
Occlusal features more likely to be associated with symptomatic TMDs include a centric relation to centric occlusion slide of more than 2 mm; overjets of more than 4 mm; and the presence of a skeletal anterior open bite. It is likely for these reasons that White and colleagues found that TMDs were significantly greater among patients with Class II skeletal deformities as compared with those patients with Class III deformities.58 Westermark and colleagues studied a consecutive series of Class II patients to understand the effects of orthognathic surgery on the signs and symptoms of TMD.57 Preoperatively, 43% of the patients reported subjective symptoms of TMD; postoperatively, 28% reported such symptoms. This difference suggests an overall beneficial effect of orthognathic surgery for many individuals with Class II mandibular deficiencies.28 Interestingly, clinical studies indicate that patients with mandibular retrusion and TMD do not improve as much from an orthognathic correction as patients with a Class III skeletal pattern do (see Chapter 9).
References
1. Abeloos, J, De Clercq, C, Neyt, L. Skeletal stability following miniplate fixation after bilateral sagittal split osteotomy for mandibular advancement. J Oral Maxillofac Surg. 1993; 91:624.
2. Angle, EH. Treatment of malocclusion of the teeth: Angle’s system, ed 7. Philadelphia: S. S. White; 1907.
3. Arnett, GW, Bergman, RT. Facial keys to orthodontic diagnosis and treatment planning—part I. Am J Orthod Dentofacial Orthop. 1993; 103:299–312.
4. Arnett, GW, Bergman, RT. Facial keys to orthodontic diagnosis and treatment planning—part II. Am J Orthod Dentofacial Orthop. 1993; 103:395–411.
5. Bell, WH, Proffit, WR, White, RP. Surgical correction of dentofacial deformities. Philadelphia: W. B. Saunders Company; 1980.
6. Bell, WH, Schendel, SA. Biologic basis for modification of the sagittal split ramus osteotomy. J Oral Surg. 1977; 35:362.
7. Blair, VP. Surgery of the mouth and jaws. St. Louis: Mosby; 1914.
8. Blomqvist, JE, Ahlborg, G, Isaksson, S, et al. A comparison of skeletal stability after mandibular advancement and use of two rigid fixation techniques. J Oral Maxillofac Surg. 1997; 55:568.
9. Bouwman, JP, Kerstens, HC, Tuinzing, DB. Condylar resorption in orthognathic surgery. The role of intermaxillary fixation. Oral Surg Oral Med Oral Pathol. 1994; 78:138.
10. Broadbend, TR, Woolf, RM. Our experience with sagittal split osteotomy for retrognathia. Plast Reconstr Surg. 1977; 60:860.
11. Burstein, FD, Cohen, SR, Scott, PH, et al. Surgical therapy for severe refractory sleep apnea in infants and children: application of the airway zone concept. Plast Reconstr Surg. 1995; 96:34.
12. Chamberland, S, Proffit, WL. Short-term and long-term stability of surgically assisted rapid palatal expansion revisited. Am J Orthod Dentofacial Orthop. 2011; 139:815–822.
13. Coben, SE. Growth and Class II treatment. Am J Orthod. 1966; 52:5–26.
14. Cozza, P, Baccetti, T, et al. Mandibular changes produced by functional appliances in Class II malocclusion: A systematic review. Am J Orthod Dentofacial Orthop. 2006; 129:599e1–599e12.
15. Epker, BN. Occlusal plane alteration in orthognathic surgery [discussion]. J Oral Maxillofac Surg. 1993; 51:740–741.
16. Epker, BN, Wessberg, GA. Mechanisms of early skeletal relapse following surgical advancement of the mandible. Br J Oral Surg. 1982; 20:175–182.
17. Ewing, M, Ross, RB. Soft tissue response to mandibular advancement and genioplasty. Am J Orthod Dentofacial Orthop. 1992; 101:550–555.
18. Finn, RA. Biomechanical considerations in the surgical correction of mandibular deficiency. J Oral Surg. 1980; 38:257–264.
19. Friehofer, H, Petresevic, D. Late results after advancing the mandible by sagittal splitting of the rami. J Maxillofac Surg. 1975; 3:250–257.
20. Friehofer, HP. Results of osteotomies of the facial skeleton in adolescence. J Maxillofac Surg. 1977; 5:267–297.
21. Gallo, W, Moss, M, Gaul, J. Modification of the sagittal split ramus osteotomy for retrognathia. J Oral Surg. 1976; 34:178–179.
22. Guernse, YL. Stability of treatment results in Class II malocclusion corrected by full mandibular advancement surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1974; 37:668.
23. Huang, CS, Bruce-Ross, R. Surgical advancement of the retrognathic mandible in growing children. Am J Orthod. 1982; 82:89–103.
24. Jackson, L. Outpatient orthognathic surgery: review of 205 cases [discussion]. J Oral Maxillofac Surg. 1997; 55:563.
25. Jacobs, JS. Mandibular retrusion, temporomandibular joint derangement, and orthognathic surgery planning [discussion]. Plast Reconstr Surg. 1992; 90:230.
26. Jäger, A, Kubein-Meesenburg, D, Luhr, HG. Longitudinal study of combined orthodontic and surgical treatment of Class II malocclusion with deep overbite. Int J Adult Orthod Orthognath Surg. 1991; 6:29.
27. Johnston, LEJr. Level of agreement in clinicians’ perceptions of Class II malocclusions [discussion]. J Oral Maxillofac Surg. 1994; 52:572.
28. Magnusson, T, Ahlborg, G, Svartz, K. Function of the masticatory system in 20 patients with mandibular hypo- or hyperplasia after correction by a sagittal split osteotomy. Int J Oral Maxillofac Surg. 1990; 19:289.
29. McNeil, RW, West, RA. Severe mandibular retrognathism: orthodontic versus surgical orthodontic treatment. Am J Orthod. 1977; 72:176–182.
30. Newman, GV. Prevalence of malocclusion in children six to fourteen years of age and treatment in preventable cases. J Am Dent Assoc. 1965; 52:566–575.
31. Ngan, PW, Byczek, E, Scheick, J. Longitudinal evaluation of growth changes in Class II Division 1 subjects. Semin Orthod. 1997; 3:222–231.
32. O’Brian, K. Is early treatment for Class II malocclusion effective? Results from a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2006; 120(Suppl 1):564–565.
33. O’Brian, K, Wright, J, Conboy, F, et al. Effectiveness of early orthodontic treatment with the twin-block appliance: a multi-center, randomized, controlled trial. Part 2: Psychosocial effects. Am J Orthod Dentofacial Orthop. 2003; 124:488–495.
34. Obwegeser, HL. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty: part 1. Oral Surg. 1957; 10:677.
35. Obwegeser, HL. The indications for surgical correction of mandibular deformity by the sagittal splitting technique. Br J Oral Surg. 1964; 1:157–171.
36. Obwegeser, HL. Variations of a standard approach for correction of the bird-face deformity. J Craniomaxillofac Surg. 1988; 16:247–265.
37. Obwegeser, HL, Hadjianghelou, O. Two ways to correct bird-face deformity. Oral Surg Oral Med Oral Pathol. 1987; 64:507–518.
38. Otuyemi, OD, Jones, SP. Long-term evaluation of treated Class II Division 1 malocclusions utilizing the PAR index. Br J Orthod. 1995; 22:171–178.
39. Phillips, C, Bailey, LJ, Sieber, RP. Level of agreement in clinicians’ perceptions of Class II malocclusions. J Oral Maxillofac Surg. 1994; 52:565.
40. Posnick, J, Fantuzzo, J, Orchin, J. Deliberate operative rotation of the maxillo-mandibular complex to alter the A-point to B-point relationship for enhanced facial esthetics. J Oral Maxillofac Surg. 2006; 64:1687–1695.
41. Posnick, JC. Occlusal plane rotation: aesthetic enhancement in mandibular micrognathia [discussion]. Plast Reconstr Surg. 1993; 91:1241.
42. Posnick JC, ed. Mandibular deficiency with or without maxillary deformity. Craniofacial and maxillofacial surgery in children and young adults. W. B. Saunders Company: Philadelphia, 2000:981–1003.
43. Proffit, WR, Fields, HW, Jr., Moray, LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult Orthodon Orthognath Surg. 1998; 13:97.
44. Proffit, WR, Phillips, C, Douvartzidis, N. A comparison of outcomes of orthodontic and surgical-orthodontic treatment of Class II malocclusion in adults. Am J Orthod Dentofacial Orthop. 1992; 101:556–565.
45. Reichenback, E. Uber den zeitpunk kieferchirurgisch-orthod-padischer, Eingriffe, Stsch. Zahn-Mund-Kierferheilkd. 1966; 47:302.
46. Reyneke, JP, Evans, WG. Surgical manipulation of the occlusal plane. Int J Adult Orthodon Orthognath Surg. 1990; 5:99–110.
47. Rosen, H. Aesthetics in facial skeletal surgery. Perspect Plast Surg. 1993; 6:1.
48. Rosen, HM. Surgical correction of the vertically deficient chin. Plast Reconstr Surg. 1988; 82:247.
49. Rosen, HM. Occlusal plane rotation: aesthetic enhancement in mandibular micrognathia. Plast Reconstr Surg. 1993; 91:1231.
50. Rowe, NL. The etiology, clinical features and treatment of mandibular deformity. Br Dent J. 1960; 108:45–112.
51. Schellhas, KP, Piper, MA, Bessette, RW, et al. Mandibular retrusion, temporomandibular joint derangement, and orthognathic surgery planning. Plast Reconstr Surg. 1992; 90:218.
52. Schendel, SA, Wolford, LM, Epker, BN. Mandibular deficiency syndrome. III. Surgical advancement of the deficient mandible in growing children: treatment results in twelve patients. Oral Surg Oral Med Oral Pathol. 1978; 45:364–377.
53. Simmons, KE, Turvey, TA, Phillips, C, Proffit, WR. Surgical orthodontic correction of mandibular deficiency: five-year follow-up. Int J Adult Orthodon Orthognath Surg. 1992; 7:67–80.
54. Snow, MD, Turvey, TA, Walker, D, et al. Surgical mandibular advancement in adolescents: postsurgical growth related to stability. Int J Adult Orthodon Orthognath Surg. 1991; 6:143.
55. Stahl, F, Baccetti, T, Franchi, L, McNamara, JA. Longitudinal growth changes in untreated subjects with Class II Division 1 malocclusion. Am J Orthod Dentofacial Orthop. 2008; 134:125–137.
56. Van Sickels, JE. A comparative study of bicortical screw and suspension wires versus bicortical screws in large mandibular advancements. J Oral Maxillofac Surg. 1991; 49:1293.
57. Westermark, A, Shayeghi, F, Thor, A. Temporomandibular dysfunction in 1516 patients before and after orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 2001; 16:145–151.
58. White, CS, Dolwick, MF. Prevalence and variance of temporomandibular dysfunction in orthognathic surgery patients. Int J Adult Orthodon Orthognath Surg. 1992; 7:7–14.
59. Wolfe, SA, Berkowitz, S. The mandible. In: Wolfe SA, Berkowitz S, eds. Plastic surgery of the facial skeleton. Boston: Little, Brown; 1989:149.
60. Wolford, LM, Chemello, PD, Hilliard, FW. Occlusal plane alteration in orthognathic surgery. J Oral Maxillofac Surg. 1993; 51:730.
61. Woldford, LM, Schendel, SA, Epker, BN. Surgical orthodontic correction of mandibular deficiency in growing children (long term treatment result). J Maxillofac Surg. 1979; 7:61–72.
62. Yu, LF, Pogrel, MA, Ajayi, M. Pharyngeal airway changes associated with mandibular advancement. J Oral Maxillofac Surg. 1994; 52:40.
63. Zarrinkelk, HM, Throckmorton, GS, Ellis, E, III., et al. A longitudinal study of changes in masticatory performance of patients undergoing orthognathic surgery. J Oral Maxillofac Surg. 1995; 53:777.



