Presacral Neurectomy
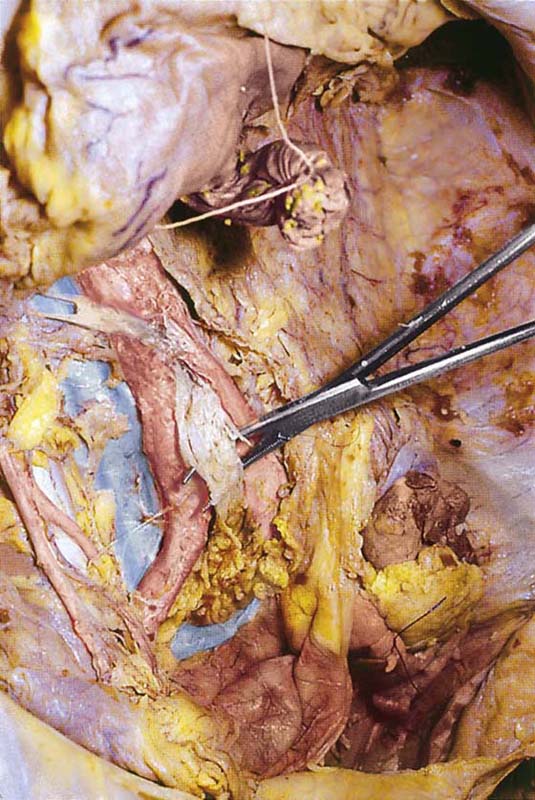
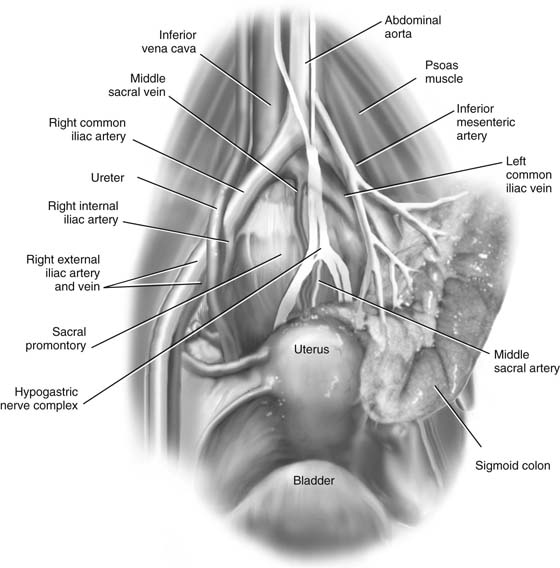
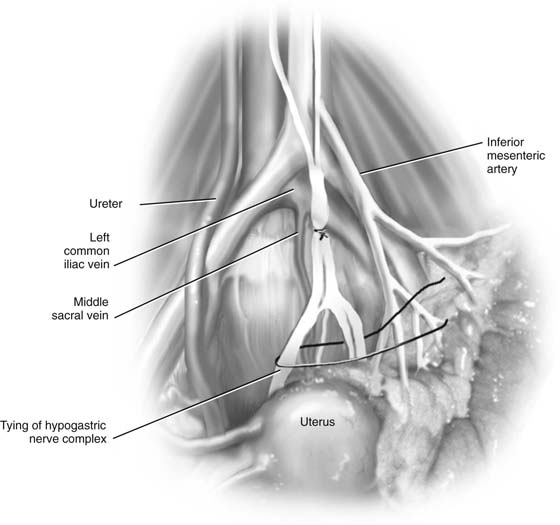
Pain fibers are transmitted from the uterus via the hypogastric plexus. The hypogastric plexus of nerves cascades downward as a continuation of the celiac plexus on the anterior aspect of the distal portion of the abdominal aorta (Fig. 38–1). The hypogastric plexus is variable in configuration but can be rather loosely separated into superior, middle, and inferior divisions. The middle hypogastric plexus typically divides into two main nerve trunks coursing inferiorly within the presacral space. The nerves are always medial to the common iliac arteries but cross over (anteriorly) the left common iliac vein (Fig. 38–2). The middle sacral vessels are located posterior (deep) to these nerves. The inferior hypogastric plexus continues to descend into the lower pelvis and joins with the pelvic plexus, receiving rectal, vesical, and uterine afferents and carrying sympathetic efferents.
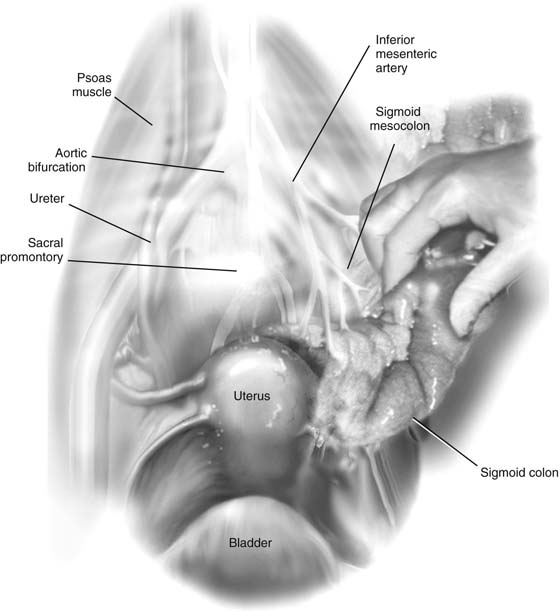
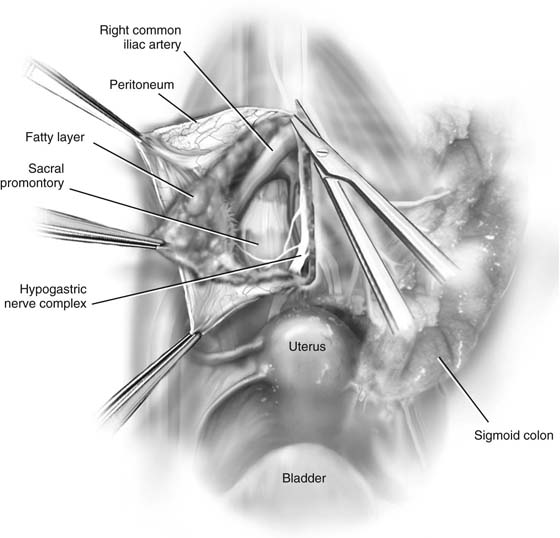
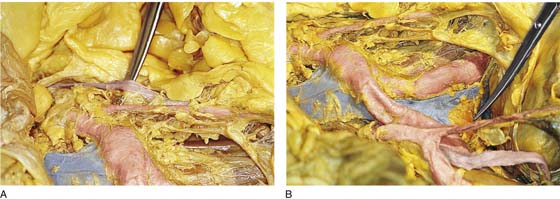
The middle hypogastric plexus is accessed by reflecting the sigmoid to the left and anteriorly (Fig. 38–3). The peritoneum overlying the sacrum is grasped and incised vertically toward the sacral promontory (Fig. 38–4). Care is taken to identify the left common iliac vein, the left ureter, and the inferior mesenteric artery (and vein) (Fig. 38–5A, B).
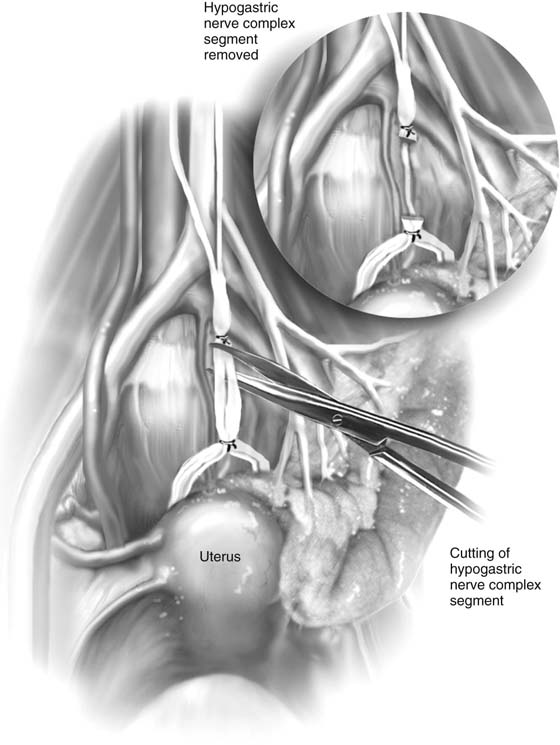
The hypogastric nerves are dissected with a long tonsil clamp or right-angle clamp, with care taken to avoid injuring the middle sacral vessels (Fig. 38–6). A 3- to 4-cm segment of nerve is isolated. At the upper and lower extremes of the dissection, a permanent ligature is passed beneath the dissected hypogastric nerve and is tied tightly (Fig. 38–7). The segment of nerve between the two ligatures is dissected from its loose attachments to the underlying sacral bone. With long curved Mayo scissors, the nerve segment is cut out and is placed in fixative for subsequent pathologic diagnosis (Fig. 38–8).
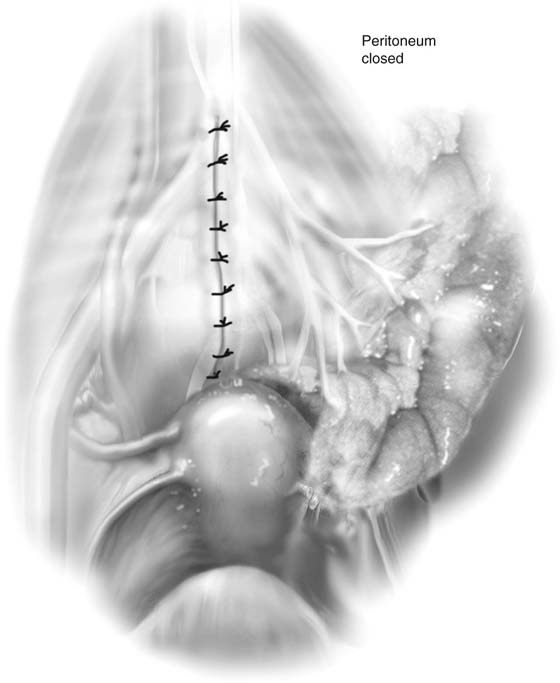
The operative site is examined for bleeding and is irrigated with normal saline. The cut edges of the peritoneum are grasped and closed with running or interrupted 3-0 Vicryl sutures (Fig. 38–9).
If the middle sacral vessels are injured, significant bleeding will occur. This hemorrhage is difficult to control because these vessels are difficult to clamp or suture. The author recommends pushing a sterile stainless steel thumb tack into the sacrum, thereby compressing the vessels.
FIGURE 38–1 The curved clamp lies on the abdominal aorta just cranial to its bifurcation. The clamp has dissected free and lies beneath the hypogastric nerve (plexus). The view is from below, looking into the pelvis. Note the inferior vena cava to the right of the aorta.
FIGURE 38–2 The tip of the clamp points to the left common iliac vein. The elevated ligature encircles the middle hypogastric plexus as it descends into the pelvis over the presacral space.
FIGURE 38–3 The operator has retracted the sigmoid colon to the left. The peritoneum covering the presacral space remains intact.
FIGURE 38–4 The peritoneum has been excised upward toward the sacral promontory. The structures overlying the anterior surface of the sacrum and the L5 vertebra are visualized.
FIGURE 38–5 A. The scissors lie under the dissected left ureter (far lateral); the scissors tip points to the takeoff (origin) of the inferior mesenteric artery. The latter supplies the left and sigmoid colon. The right common iliac artery is seen in the foreground. B. The tip of the scissors points to the sacral promontory. The right ovarian vessels and the right ureter (below the vessels) cross the right iliac artery and descend into the pelvis at the right lateral margin of the presacral space.
FIGURE 38–6 The hypogastric nerve has been exposed by careful dissection. The important anatomic relationships must be recognized. Posterior to the nerve are the middle sacral vessels and the sacral bone. To the right are the common iliac vessels and the ureter. To the left and above are the left common iliac vein and the inferior mesenteric vessels.
FIGURE 38–7 A 2-0 silk ligature is passed around the upper and lower margins of the nerve segment to be removed. The ligatures are tied tightly into place and cut.
FIGURE 38–8 The segment of hypogastric nerve is cut out with the use of Metzenbaum scissors. The segment is placed in fixative and is sent to pathology. The field is irrigated with normal saline and is carefully examined for any bleeding.
FIGURE 38–9 The peritoneum overlying the sacrum is closed with interrupted or running 3-0 Vicryl sutures. Care is taken to avoid encroaching on the right ureter or inferior mesenteric artery during closure.