CHAPTER 36 Preoperative Planning, Imaging, and Special Tests
Revision shoulder arthroplasty is more challenging overall than primary shoulder arthroplasty. Preoperative planning for a revision arthroplasty case is critically important and is initiated as soon as revision arthroplasty is being considered; it should never be an afterthought the morning of surgery. Preoperative planning for revision shoulder arthroplasty is similar to, albeit more complex than, planning for primary shoulder arthroplasty and consists of reviewing the patient’s clinical history and physical examination, radiographs, and secondary imaging studies, as well as any special tests obtained. This chapter reviews our approach to preoperative planning for revision shoulder arthroplasty.
CLINICAL HISTORY AND EXAMINATION
All of our patients undergo a thorough shoulder examination, much of which is detailed in Chapter 7. The visual appearance of the shoulder yields useful information in candidates for revision shoulder arthroplasty. The presence and location of surgical scars are noted. The preoperative plan should include whether all or part of a previous skin incision site is to be used or whether a completely new incision is to be created (Fig. 36-1). In thin patients, anterior superior escape of a prosthetic humeral head caused by anterior superior rotator cuff deficiency may be obvious (Fig. 36-2). Special attention should be paid to the condition of the deltoid, especially if it has previously been surgically violated (Fig. 36-3). Atrophy of the supraspinatus and infraspinatus should be noted as well (Fig. 36-4).
Both active and passive mobility is recorded, as detailed in Chapter 7. Special attention should be paid to evaluation of the deltoid muscle. If deltoid contractility appears to be compromised, further evaluation with electromyography and nerve conduction studies should be performed before revision shoulder arthroplasty.
The integrity of the rotator cuff is tested (see Chapter 7). Details of this examination are of paramount importance in preoperative planning for revision surgery. Although a minor rotator cuff deficiency such as an isolated supraspinatus tendon tear may have little influence on preoperative planning, larger rotator cuff tears (two-, three-, and four-tendon tears), especially when coupled with static or dynamic glenohumeral instability, may change the type of revision prosthesis to be inserted (reverse instead of unconstrained).
RADIOGRAPHY
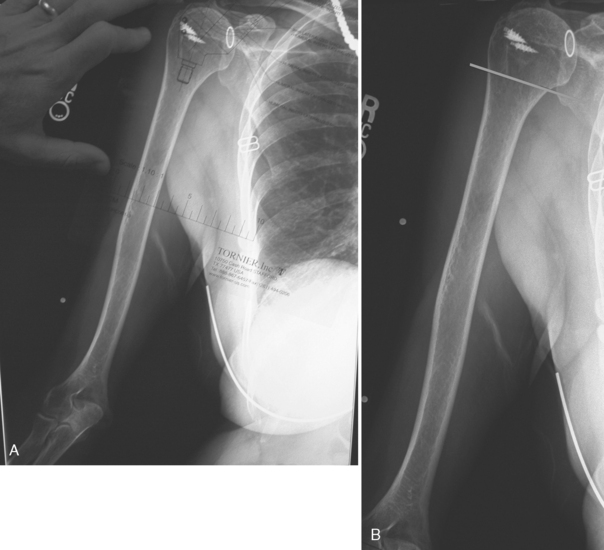
Recent (within 3 months) magnification- and fluoroscopy-controlled radiographs are obtained in all patients who are candidates for revision shoulder arthroplasty. The same views obtained for primary arthroplasty, including an anteroposterior view of the glenohumeral joint with the arm in neutral rotation, an axillary view, and a scapular outlet view, are obtained in the revision scenario. Additionally, full-length orthogonal views of the humerus (anteroposterior and lateral) are obtained to evaluate diaphyseal cortical bone quality (Fig. 36-5). The previous arthroplasty is inspected on these radiographs for signs of loosening of the glenoid and humeral components, signs of mechanical failure of components (Fig. 36-6), appropriateness of component size and position, signs of static or dynamic instability (Fig. 36-7), and signs of infection (Fig. 36-8).
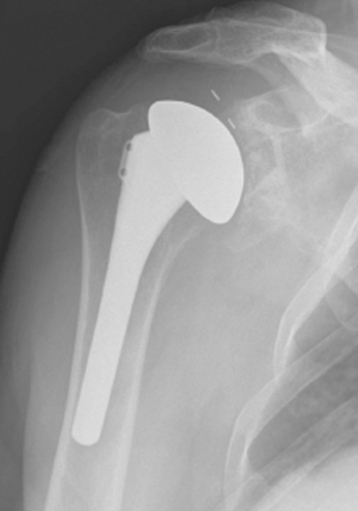
Figure 36-6 Mechanical failure of a keeled glenoid component detected on anteroposterior radiography.
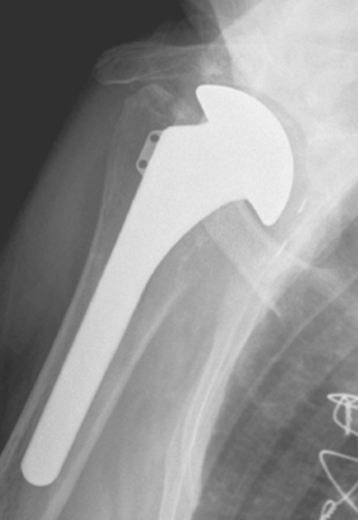
Figure 36-8 Osteolysis around both the glenoid and humeral components is strongly suggestive of infection.
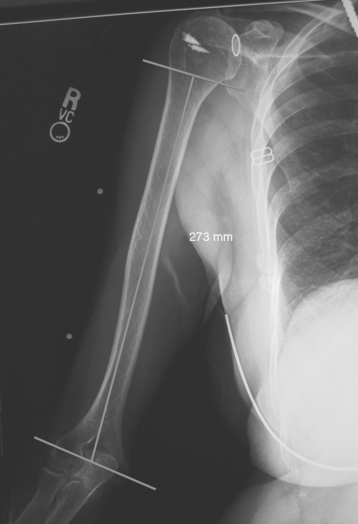
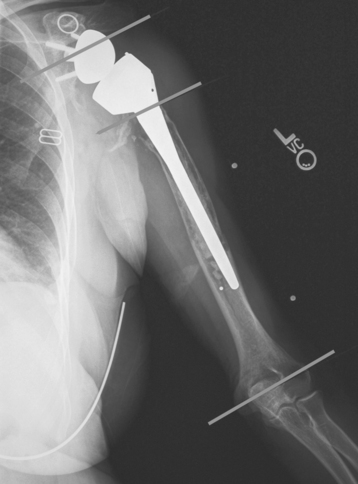
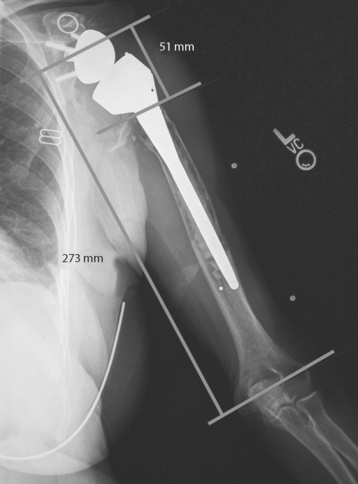
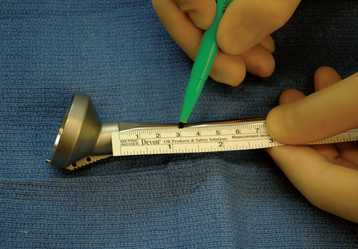
Preoperative radiographic templating can be useful in planning revision shoulder arthroplasty, especially in cases of proximal humeral deficiency. In most of these cases, the proximal humeral deficiency with resultant rotator cuff compromise constitutes an indication for revision with a reverse-design prosthesis. In patients demonstrating proximal humeral bone loss, bilateral full-length magnification-controlled anteroposterior humeral radiographs are obtained. These radiographs are used to help select the height at which to implant the humeral stem. Using the full-length humeral radiographs, the desired position of the reverse prosthesis is templated on the radiograph of the unaffected humerus, and the level of the metaphyseal-diaphyseal junction of the humeral component is marked (Fig. 36-9). The distance from the transepicondylar axis at the elbow to this point is measured (Fig. 36-10). A mark is made at the same distance from the transepicondylar axis on the affected radiograph. A second mark is made at the most proximal extent of the humeral shaft (Fig. 36-11). The distance between the desired prosthetic level at the metaphyseal-diaphyseal junction and the proximal extent of the humeral shaft is measured (Fig. 36-12). A ruler is used during surgery to measure the distance and mark the level on the humeral stem for the desired prosthetic position (Fig. 36-13). This technique of preoperative planning provides only a guideline and may be superseded by intraoperative observations.
SECONDARY IMAGING
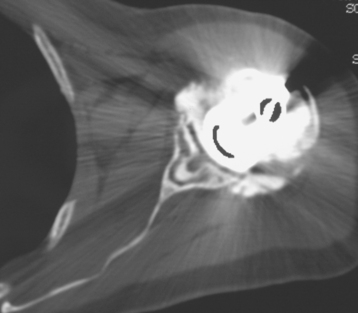
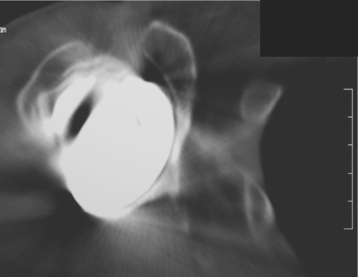
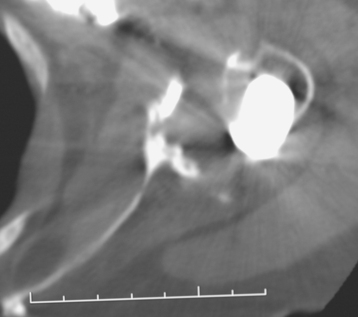
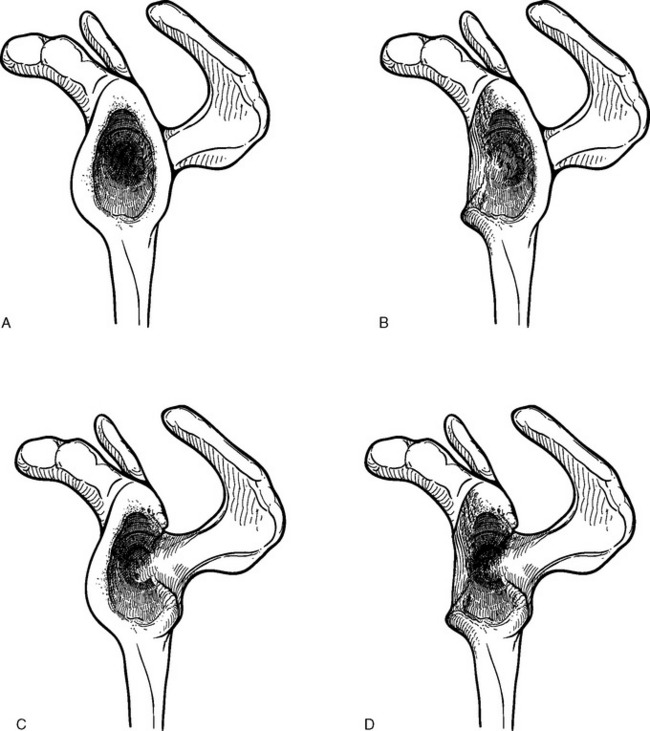
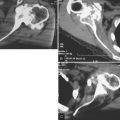
A computed tomographic arthrogram is obtained in all patients for evaluation of the rotator cuff tendons and musculature before revision shoulder arthroplasty (Fig. 36-14). This study further assists in evaluation of possible component loosening. Many patients exhibit radiolucent lines around the glenoid component after unconstrained total shoulder arthroplasty. Use of computed tomographic arthrography assists in determining whether these components are indeed loose by demonstrating radiographic contrast material around the base of the component (Fig. 36-15). Computed tomography also provides the greatest osseous detail of the glenoid and can show the presence and extent of bony glenoid deficiency. Bony deficiencies can occur after erosion from hemiarthroplasty (Fig. 36-16). In these cases the computed tomogram helps determine whether the existing glenoid bone is sufficient to allow implantation of a glenoid component. Bony deficiencies more commonly occur concomitantly with loosening of the glenoid component (Fig. 36-17). In these cases the computed tomogram allows the bony deficiency to be classified as contained or uncontained (Fig. 36-18).1
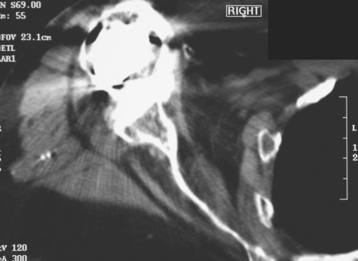
Figure 36-14 Evaluation of the rotator cuff tendons and musculature with computed tomographic arthrography.