CHAPTER 18 Preoperative Planning and Imaging
Preoperative planning is important for all shoulder arthroplasty indications, but it is most crucial for fracture cases. Although proximal humeral anatomy may be somewhat distorted by prolonged wear and osteophyte formation in cases of chronic disease for which shoulder arthroplasty is performed, most reliable anatomic landmarks remain consistent despite the disease process. In fracture cases, however, these normally reliable landmarks are often displaced, thus making them useless as points of reference. Because of the lack of recognizable landmarks, preoperative planning becomes of paramount importance when attempting to establish the proper position for humeral stem implantation. Thorough preoperative planning minimizes the risk of placing the humeral stem at the incorrect height or version. We have successfully used two techniques to place the humeral stem at the appropriate height. Preoperative planning is of paramount importance for both these techniques and is detailed in this chapter. Additionally, important aspects of the clinical history and physical examination, the radiographic examination, and secondary imaging studies are highlighted.
RADIOGRAPHY
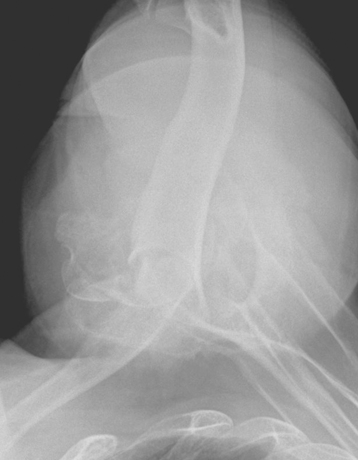
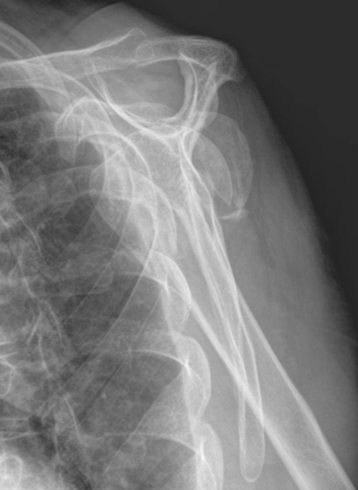
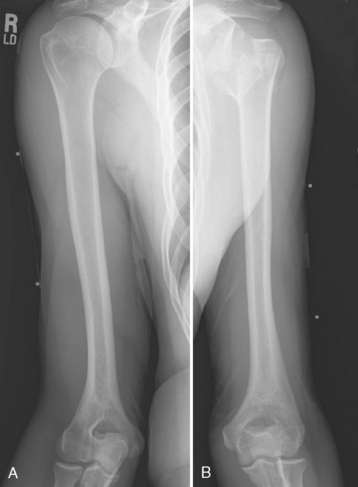
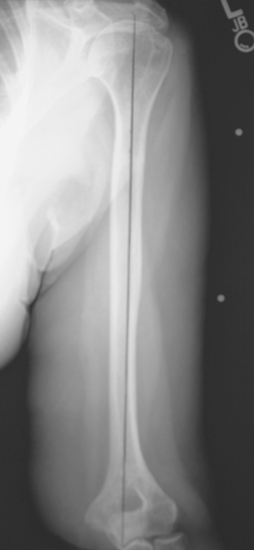
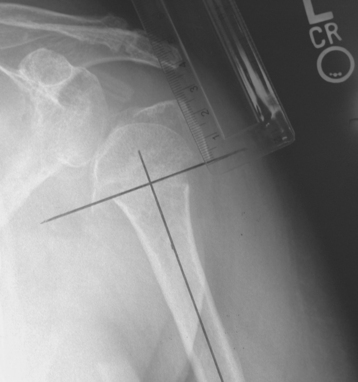
Three radiographic views are obtained in all patients with a proximal humeral fracture. We prefer the same radiographic views that we obtain for patients being considered for unconstrained shoulder arthroplasty for chronic conditions: an anteroposterior view of the glenohumeral joint with the arm in neutral rotation (Fig. 18-1), an axillary view (Fig. 18-2), and a scapular outlet view (Fig. 18-3). These radiographs are used to evaluate the fracture pattern (two part, three part, four part), the amount of displacement of the fracture fragments, the presence of humeral head dislocation, and the presence of a split in the humeral head fragment. Frequently, the patient has radiographs obtained in an emergency department that are of poor quality. We always repeat these radiographs to obtain better-quality films and to assess for progressive displacement. Once it is determined that the patient is a potential candidate for shoulder hemiarthroplasty, anteroposterior full-length radiographs of both humeri taken with the arm in neutral rotation are obtained for use in preoperative determination of appropriate humeral head height. These radiographs must include the entire length of the humerus and must be controlled for magnification (Fig. 18-4).
SECONDARY IMAGING
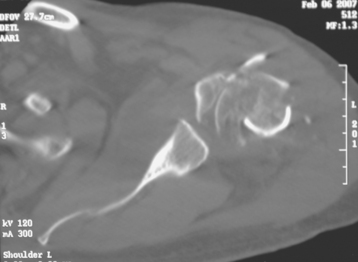
Computed tomography is performed in all patients with substantially displaced proximal humeral fractures (Fig. 18-5). This study allows further elucidation of the fracture pattern and assessment of the amount of displacement of the fracture fragments. Additionally, the position of the tuberosities and humeral head is visualized, thereby allowing easier identification at the time of surgery. Any comminution of the tuberosities can be identified with computed tomography as well.
PROSTHETIC POSITIONING WITH ANCILLARY INSTRUMENTATION—THE FRACTURE JIG TECHNIQUE
Placement of the prosthesis at the correct height and version remains one of the most difficult challenges when performing shoulder arthroplasty for fracture. Use of specialized instrumentation enhances the surgeon’s ability to place the prosthesis at the correct height and in the correct amount of retroversion.1 The fracture jig references the humeral epicondyles to allow intraoperative estimation of proper prosthetic height and retroversion. More importantly, the fracture jig permits trial reduction of the glenohumeral joint and reduction of the tuberosities before final cementation of the humeral implant, thus allowing adjustment of prosthetic position.
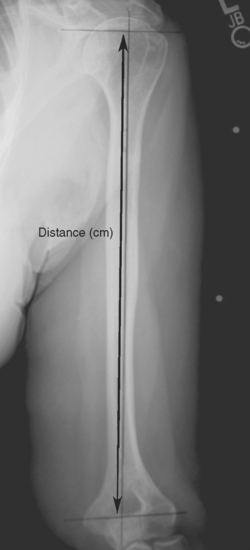
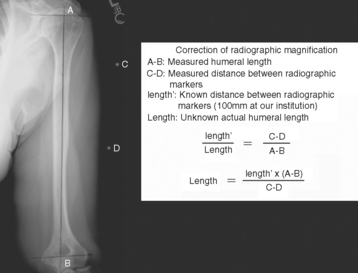
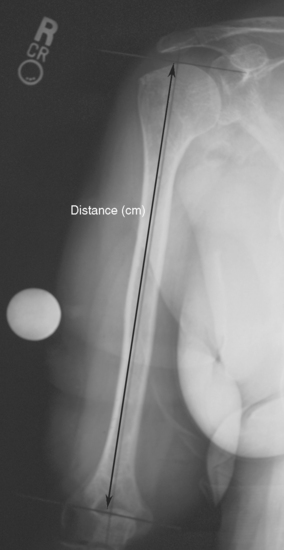
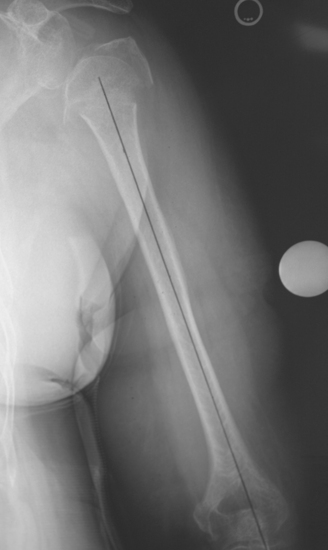
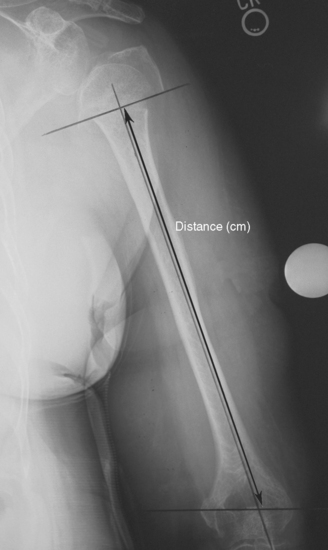
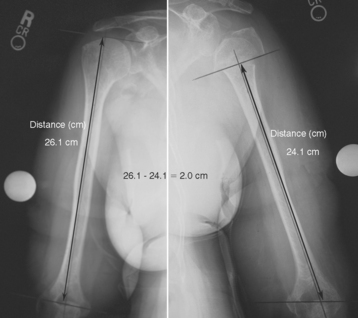
When preoperative planning is performed for the fracture jig technique, only the anteroposterior full-length humeral radiograph of the unaffected arm is required. From this radiograph the length of the humerus from the superior aspect of the greater tuberosity to the transepicondylar axis is measured and normalized for magnification. This measurement is obtained by first establishing the prosthetic axis proximally within the humeral canal. We do this by measuring the center point of the proximal diaphysis at two locations and connecting these points with a line running the length of the humerus (Fig. 18-6). Next, a line perpendicular to the prosthetic axis is drawn at the level of the greater tuberosity (Fig. 18-7). A third line intersecting the prosthetic axis is drawn at the transepicondylar axis of the distal humerus (Fig. 18-8). The distance between the greater tuberosity and the transepicondylar axis is measured in centimeters along the prosthetic axis (Fig. 18-9). This value is corrected for magnification if necessary (a digital radiography system does this step automatically at our institution) by using the mathematical formula shown in the example in Figure 18-10. This measurement, once corrected for radiographic magnification, provides an estimated height at which to set the fracture jig during the procedure.
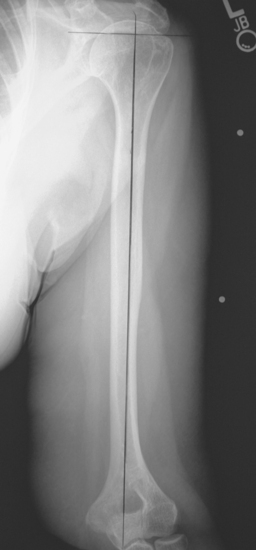
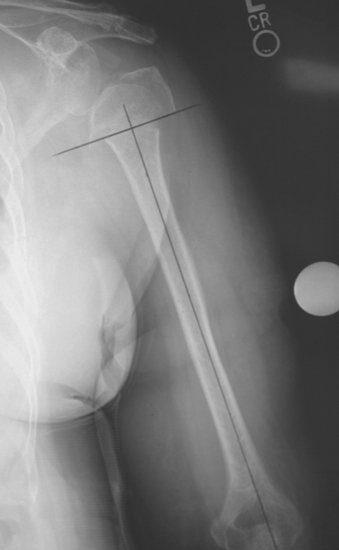
Figure 18-7 A perpendicular is constructed to the prosthetic axis at the level of the greater tuberosity.
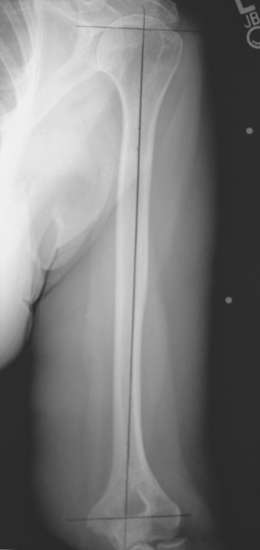
Figure 18-8 A line is drawn at the transepicondylar axis of the distal humerus intersecting the prosthetic axis.
PROSTHETIC POSITIONING WITHOUT ANCILLARY INSTRUMENTATION—THE GOTHIC ARCH TECHNIQUE
Although the fracture jig technique has proved valuable in improving prosthetic positioning during shoulder hemiarthroplasty performed for fracture, it does have certain disadvantages. First, many surgeons consider the instrumentation bulky and awkward. Second, lack of familiarity with the instrumentation combined with the infrequency with which hemiarthroplasty is performed for fracture by many surgeons has prevented them from using the fracture jig technique. Finally, the body habitus (obesity or soft tissue swelling from trauma) of many patients limits the usefulness of the fracture jig because their humeral epicondyles are not readily palpable and the large amount of soft tissue between the fracture jig and the humerus allows the fracture jig to be positioned improperly initially or to translate during the procedure. As a result of these concerns, Sumant “Butch” Krishnan has developed a technique for prosthetic positioning that we have found useful and reproducible; he terms the technique “restoration of the Gothic arch.”2
When using this technique it is necessary to perform preoperative planning with anteroposterior radiographs of the affected and unaffected humeri. Use of the radiograph of the unaffected humerus is similar to the technique involving the fracture jig. From this radiograph, the length of the humerus from the superior aspect of the humeral head to the transepicondylar axis is measured and normalized for magnification. This measurement is obtained by first establishing the prosthetic axis proximally within the humeral canal. This is done by measuring the center point of the proximal diaphysis at two locations and connecting these points with a line running the length of the humerus. Next, a line perpendicular to the prosthetic axis is drawn at the superior aspect of the humeral head (Fig. 18-11). A third line intersecting the prosthetic axis is drawn at the transepicondylar axis of the distal humerus. The distance between the superior aspect of the humeral head and the transepicondylar axis is measured in centimeters along the prosthetic axis (Fig. 18-12). Just as with the fracture jig technique, this value is corrected for magnification if necessary (a digital radiography system does this step automatically at our institution) by using the mathematical formula shown in the example in Figure 18-10.
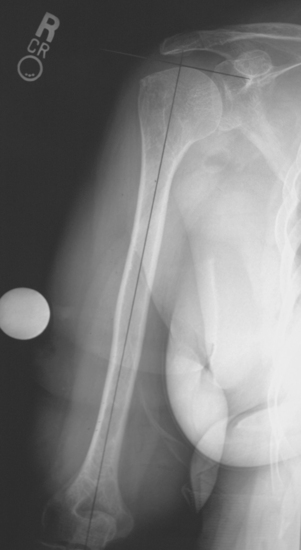
By using the anteroposterior humeral radiograph of the affected extremity, the prosthetic axis and transepicondylar axis are established (Fig. 18-13). A line perpendicular to the prosthetic axis is drawn at the level of the fracture medially (Fig. 18-14). The distance between the medial fracture line and the transepicondylar axis (residual humeral length) is measured and corrected for magnification if necessary (Fig. 18-15). In cases in which the greater tuberosity is visible as a single fragment, the length of the greater tuberosity is measured and corrected for magnification (Fig. 18-16). The difference between humeral length measured on the unaffected radiograph and residual humeral length measured on the affected radiograph is calculated (Fig. 18-17). This difference is marked on the humeral implant to establish the height at which the humeral stem should be positioned with respect to the medial fracture line (Fig. 18-18). The length of the greater tuberosity, when available, is used as a checkrein. When the length of the greater tuberosity is added to length of the residual humerus, the sum should be approximately 3 to 5 mm less than the humeral length measured on the radiograph of the unaffected humerus (Fig. 18-19).
1 Boileau P, Coste JS, Ahrens PM, Staccini P. Prosthetic shoulder replacement for fracture: Results of the multicentre study. In: Walch G, Boileau P, Molé D, editors. 2000 Prosthèses d’Epaule … Recul de 2 à 10 Ans. Paris: Sauramps Medical; 2001:561-578.
2 Krishnan SG, Pennington SD, Burkhead WZ, Boileau P. Shoulder arthroplasty for fracture: Restoration of the “gothic arch”. Tech Shoulder Elbow Surg. 2005;6:57-66.