CHAPTER 7 Preoperative Planning and Imaging
Although the majority of cases of unconstrained shoulder arthroplasty are routine, certain patients have unique characteristics that merit special consideration. Preoperative planning identifies patients who may require deviation from routine unconstrained shoulder arthroplasty. Preoperative planning should be done well in advance of the surgical procedure and not be an afterthought the morning of surgery. The surgeon should review the patient’s clinical history and physical examination, radiographs, and any secondary imaging studies. This chapter presents our approach to preoperative planning for unconstrained shoulder arthroplasty.
CLINICAL HISTORY AND EXAMINATION
Any symptoms of infection, especially in patients who have previously undergone surgery or injections, should be investigated further. If patients have a history of infection after shoulder surgery or have had symptoms suggestive of infection (systemic fever; shoulder warmth, redness), a preoperative infection workup, including hematologic evaluation with a complete blood cell count and differential, a sedimentation rate, and C-reactive protein, is indicated. Additionally, a fluoroscopically guided shoulder aspirate is obtained and the specimen submitted for aerobic, anaerobic, fungal, and mycobacterial culture. If the findings are suggestive or diagnostic of infection, shoulder arthroplasty is postponed or canceled until infectious disease consultation is obtained and the infection is appropriately treated (Table 7-1).
Table 7-1 WORKUP FOR INFECTION BEFORE UNCONSTRAINED SHOULDER ARTHROPLASTY
| Test | If Abnormal |
|---|---|
| White blood cell count with differential | Increase suspicion for infection; consider arthroscopic biopsy |
| Sedimentation rate | Increase suspicion for infection if combined with an abnormal white blood cell count or C-reactive protein; consider arthroscopic biopsy |
| C-reactive protein | Increase suspicion for infection; consider arthroscopic biopsy |
| Fluoroscopically guided aspiration | Consider the shoulder as actively infected and treat as such; arthroscopic biopsy is unnecessary |
| Arthroscopic biopsy | Consider the shoulder as actively infected and treat as such |
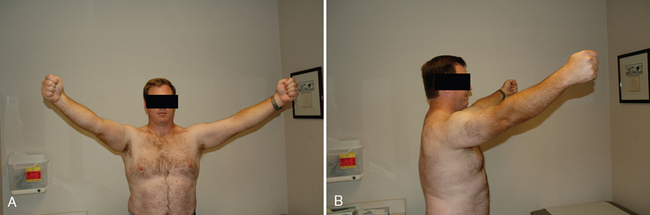
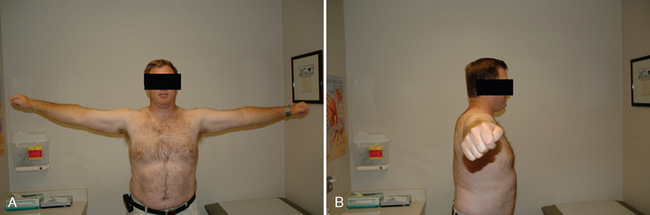
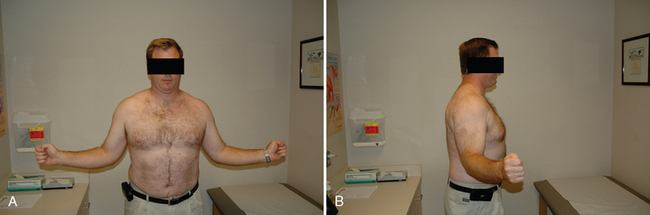
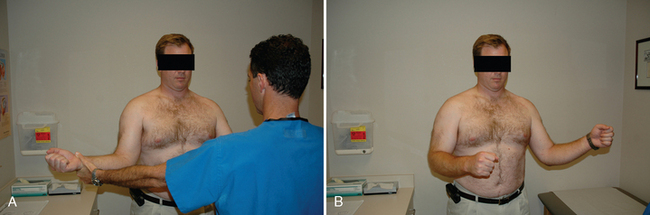
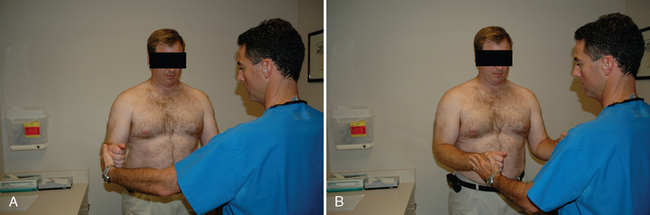
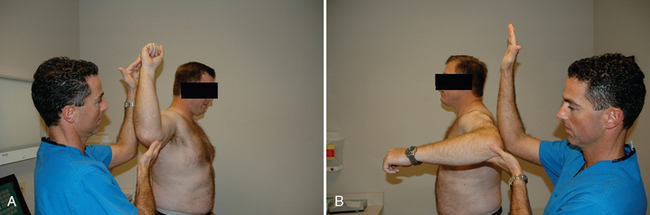
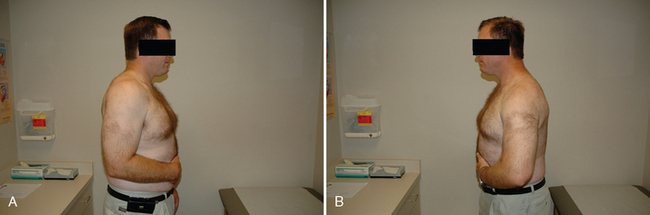
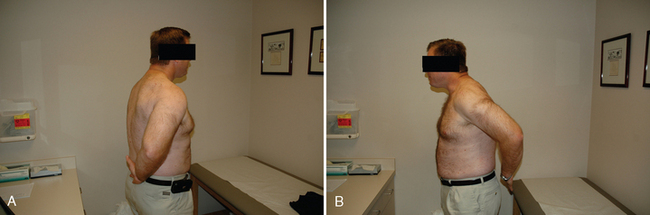
All our patients undergo a thorough shoulder examination. Motion and rotator cuff strength are of critical importance. Both active and passive mobility is recorded. Mobility parameters recorded are elevation in the plane of the scapula (Fig. 7-1), abduction (Fig. 7-2), external rotation with the arm at the side (Fig. 7-3), external rotation with the arm abducted 90 degrees (when possible) (Fig. 7-4), and internal rotation as determined by the vertebral level reached with an outstretched thumb (Fig. 7-5). Any incongruity of the glenohumeral joint as indicated by the presence of glenohumeral crepitus with motion is noted, as is any discrepancy in active and passive mobility.
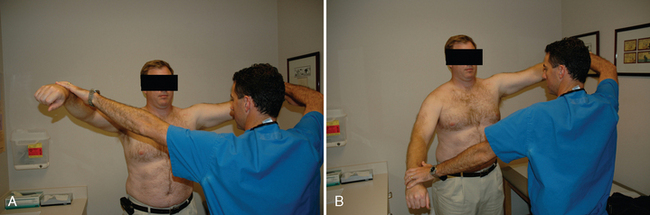
Rotator cuff examination consists of testing each tendon of the rotator cuff by isolating it as much as possible. Jobe’s test is used to test supraspinatus integrity (Fig. 7-6).1 The external rotation lag sign and evaluation of external rotation strength with the arm at the side are used to test the infraspinatus (Figs. 7-7 and 7-8).2 The teres minor is tested via the horn blower’s sign (Fig. 7-9).3 The subscapularis is tested with the belly press test and, when mobility allows, the lift-off test (Figs. 7-10 and 7-11).4
The results of the clinical history and physical examination are documented in the patient’s chart and are reviewed well in advance of surgery as part of preoperative planning.
RADIOGRAPHY
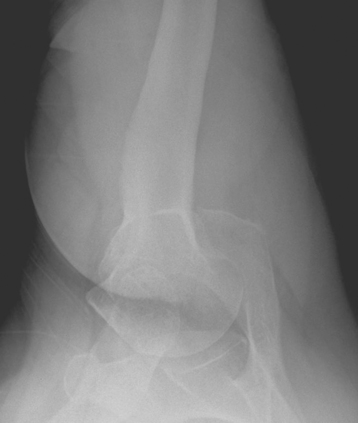
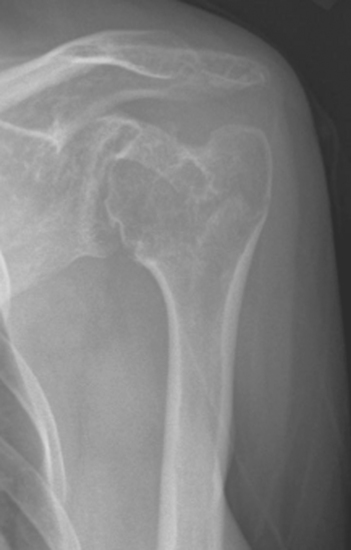
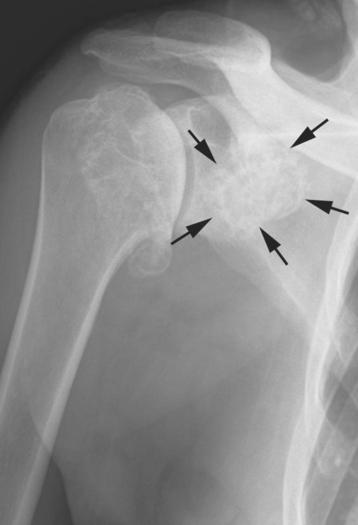
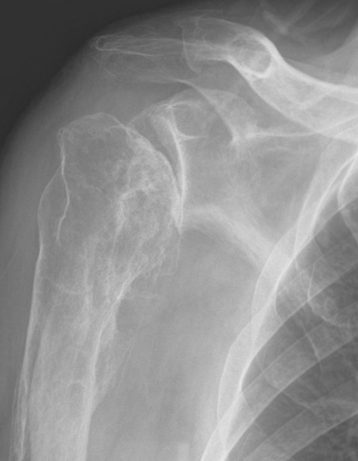
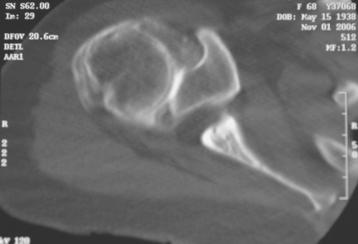
Radiographs are obtained in all patients who are candidates for shoulder arthroplasty. We prefer an anteroposterior view of the glenohumeral joint with the arm in neutral rotation (Fig. 7-12), an axillary view (Fig. 7-13), and a scapular outlet view (Fig. 7-14). The anteroposterior radiograph is used to evaluate the glenohumeral joint space, the presence of humeral and glenoid osteophytes, the size of the humeral canal (Fig. 7-15), the presence of any loose bodies (Fig. 7-16), and the presence of any deformity of the humeral shaft (Fig. 7-17) because these factors may all have an impact on the planned procedure. The axillary radiograph is used to evaluate the glenohumeral joint space, the presence of anterior or posterior humeral head subluxation, and the presence of osseous glenoid wear and dysplasia (Fig. 7-18). The scapular outlet radiograph is used to evaluate the presence of anterior or posterior humeral head subluxation (Fig. 7-19), the presence of loose bodies in the subscapularis recess, and any deformity of the humeral shaft. Findings on these radiographs assist the surgeon in predicting the need for custom implants (proximal humeral deformity), predicting the need to remove large loose bodies in the subscapularis recess that may not be visible at the time of surgery, and predicting cases in which the glenoid portion of the procedure may be exceptionally difficult.
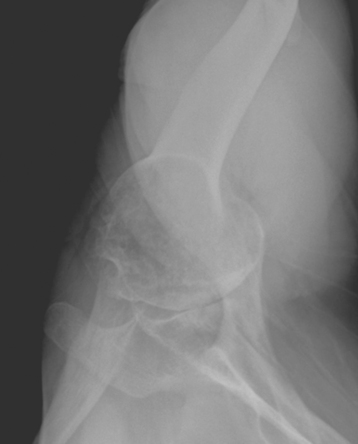
Figure 7-18 Posterior glenoid wear with posterior humeral head subluxation identified on an axillary radiograph.

Figure 7-19 Anterior humeral head subluxation with coracohumeral impingement identified on a scapular outlet radiograph.
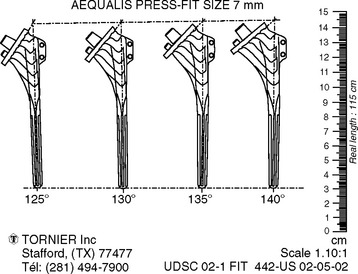
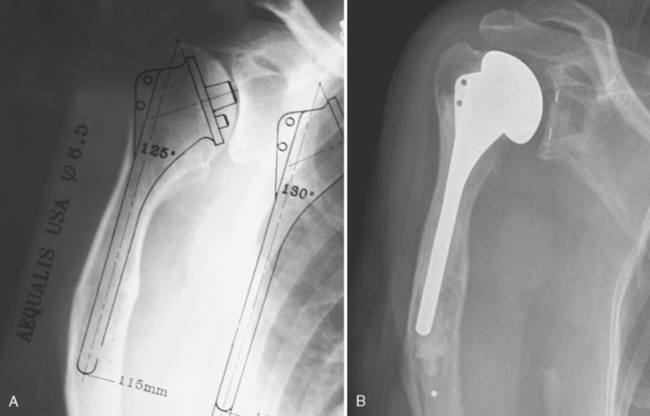
Most shoulder arthroplasty prosthetic systems have radiographic templates available for preoperative planning (Fig. 7-20). Use of an adaptable, anatomic prosthetic system minimizes the need for radiographic templates in most cases because humeral stem size, humeral head size and position, and glenoid size will be determined intraoperatively. In select cases, such as patients with substantial deformity of the proximal humerus (Fig. 7-21) or an excessively small humeral canal, use of radiographic templates preoperatively is mandatory. We use these templates to determine whether existing prefabricated implants are sufficient or a custom-manufactured implant is required.
SECONDARY IMAGING
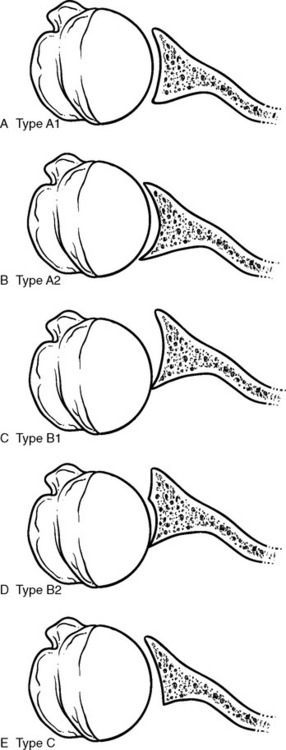
Glenoid morphology is classified by computed tomography (or magnetic resonance imaging) according to the system of Walch and colleagues (Fig. 7-22).5 In type A, or concentric glenoid morphology, the humeral head is centered, and loads are equally distributed on the glenoid. Glenoid osseous erosion may be minor, type A1, or major, type A2. Type B, or nonconcentric glenoid morphology, is characterized by a posteriorly subluxated humeral head and asymmetric loads across the glenoid. Type B1 shows narrowing of the posterior joint space, subchondral sclerosis, and osteophytes, and type B2 demonstrates a biconcave glenoid resulting from posterior osseous erosion. The final glenoid morphology, type C or dysplastic, is defined by glenoid retroversion greater than 25 degrees and a centered or only slightly subluxated humeral head. Classification of glenoid morphology is critical in two scenarios when performing unconstrained shoulder arthroplasty. First, in a patient with severe glenoid erosion (A2 and B2) or severe dysplasia (C), insufficient glenoid bone stock may prohibit implantation of a standard glenoid component (Fig. 7-23). In this case the surgeon must opt for hemiarthroplasty or choose to alter the glenoid component (i.e., shorten the keel or pegs). Second, in cases of posterior humeral head subluxation and a biconcave glenoid (B2), posterior capsulorrhaphy may be required at the time of shoulder arthroplasty. When these cases are identified by preoperative secondary imaging, an additional step of testing glenohumeral stability with the trial components is included as part of the surgical technique (Chapter 13).
The rotator cuff is next evaluated with secondary imaging modalities, including assessment of tendon integrity and evaluation of muscle quality (fatty infiltration). In addition, the condition of the long head of the biceps tendon is noted, particularly its position (centered, subluxated, dislocated, ruptured) to assist in identifying it at the time of surgery. Although full-thickness rotator cuff tears limited to the supraspinatus tendon may not change the operative plan, tears of the supraspinatus combined with either posterior (infraspinatus) or anterior (subscapularis) rotator cuff tears are contraindications to glenoid resurfacing and may best be treated with a reverse-design prosthesis (Fig. 7-24).6 The degree of fatty infiltration of the supraspinatus and infraspinatus musculature has been shown to influence the results of unconstrained shoulder arthroplasty in patients with primary osteoarthritis.6 Although we do not necessarily change our operative plan based on fatty infiltration, we routinely classify the degree of fatty infiltration of these muscles by using a three-tiered modification of the Goutallier classification to assist in determining the patient’s postoperative prognosis.7 The soft tissue axial sections of a computed tomogram or the T1-weighted axial sections of magnetic resonance imaging are used to classify fatty infiltration (Fig. 7-25).
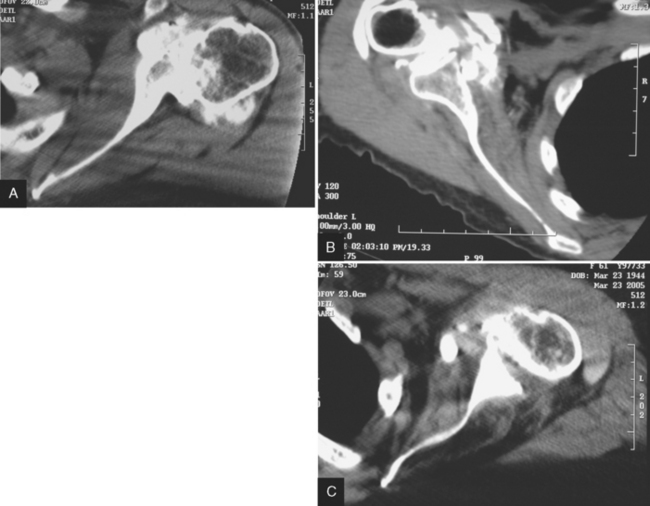
Figure 7-25 Fatty infiltration of the infraspinatus on computed tomography using a three-tiered modification of the Goutallier classification.7 In this system, mild fatty infiltration (Goutallier stage 0 and stage 1) is defined by essentially normal muscle without any or with minimal fatty streaks (A). Moderate fatty infiltration (Goutallier stage 2) is characterized by marked fatty infiltration, but there is more muscle than fat (B). In severe fatty infiltration (Goutallier stage 3 and stage 4), there is at least as much fat as muscle (C). The same classification system is used for the subscapularis.
1 Jobe FW, Jobe C. Painful athletic injuries of the shoulder. Clin Orthop Relat Res. 1983;173:117-124.
2 Hertel R, Ballmer FT, Lambert SM, et al. Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg. 1996;5:307-313.
3 Gerber C, Vinh TS, Hertel R, Hess CW. Latissimus dorsi transfer for the treatment of massive tears of the rotator cuff: A preliminary report. Clin Orthop Relat Res. 1988;232:51-61.
4 Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle: Clinical features in 16 cases. J Bone Joint Surg Br. 1991;73:389-394.
5 Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999;14:756-760.
6 Edwards TB, Boulahia A, Kempf JF, et al. The influence of the rotator cuff on the results of shoulder arthroplasty for primary osteoarthritis: Results of a multicenter study. J Bone Joint Surg Am. 2002;84:2240-2248.
7 Goutallier D, Postel JM, Bernageau J, et al. Fatty muscle degeneration in cuff rupture. Clin Orthop Relat Res. 1994;304:78-83.