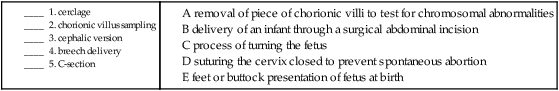
Pregnancy, Childbirth, and the Puerperium
Anatomy and Physiology of Pregnancy
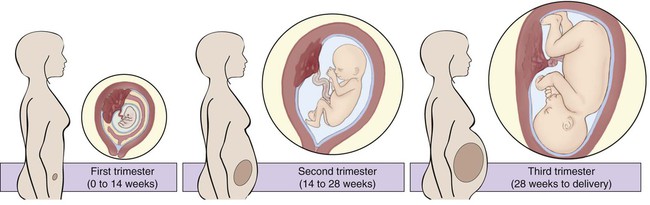
Time periods are important when using the terminology of pregnancy. A normal pregnancy is approximately 38 to 40 weeks, or 9 months. This time period is divided into trimesters, three 3-month segments. Specifically, the first trimester is less than 14 weeks 0 days; the second trimester is 14 weeks 0 days to less than 28 weeks 0 days; and the third trimester is 28 weeks 0 days until delivery (Fig. 7-1). Many ICD-10-CM codes require the addition of information as to the specific trimester of the patient’s pregnancy. The estimated date of delivery (EDD) of the infant can be calculated using a formula, Naegeli’s rule, that uses the first day of a woman’s last menstrual period (LMP), subtracts 3 months, and adds 7 days to come up with a “due” date. Note that this is based on 38 weeks (266 days). Forty weeks (280 days) is the standard time period for a pregnancy.
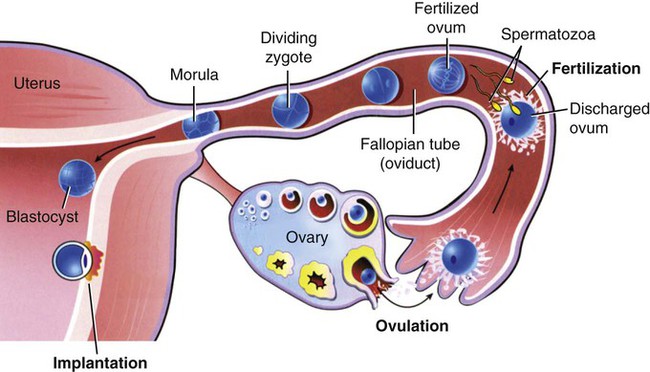
The one-celled fertilized egg, or zygote, carrying the genome (complete set of chromosomal information) divides as it moves through the fallopian tube towards the uterus (Fig. 7-2). In the first few days after fertilization, when the zygote has become a solid ball of cells from repeated divisions, it is called a morula. It is called a morula, which is Latin for mulberry, because of its similar appearance. As it continues to develop, it moves from the fallopian tube into the uterus, and becomes implanted in the uterine wall. At this point, it is identified as a blastocyst. Upon implantation, human chorionic gonadotropin (hCG), the pregnancy hormone, is secreted by the blastocyst. The hCG stimulates the corpus luteum in the ovary to continue to produce progesterone and estrogen. The continued secretion of progesterone maintains the endometrial lining to nourish the growing zygote, while the estrogen contributes to increasing the size of the lining of the uterus and the number of blood vessels that it has.
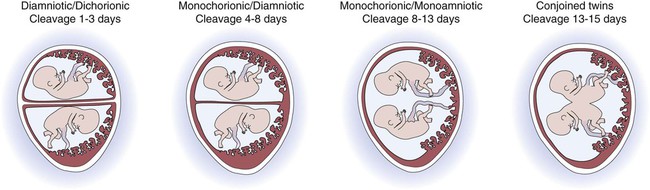
Twins are the result of a modification of this process. In the case of identical (monozygotic) twins, one zygote divides to develop into two genetically identical copies of chromosomes (identical genomes). When two ova are released and fertilized by two different sperm, fraternal (dizygotic) twins develop with two different sets of chromosomes (two genomes), making them not identical, but only as similar as siblings. Although a normal zygote has one set of membranes (an outer chorionic and inner amniotic) to support it through the pregnancy, twins may have a different configuration of sacs depending on when their fertilized eggs divide. If the egg divides 3 to 4 days after it is fertilized, the monozygotic twins will develop in two sets of sacs (dichorionic/diamniotic). If the division happens 3 to 8 days after fertilization, the twins will share the same outer sac (monochorionic) but each will be in its own inner sac (diamniotic). If the split occurs from 8 to 13 days after fertilization, they share the same outer and inner sac (monochorionic/monoamniotic). Finally, if the split happens after 13 days, the twins share the same outer and inner sac (monochorionic/monoamniotic), but the division is incomplete and results in conjoined twins (Fig. 7-3).
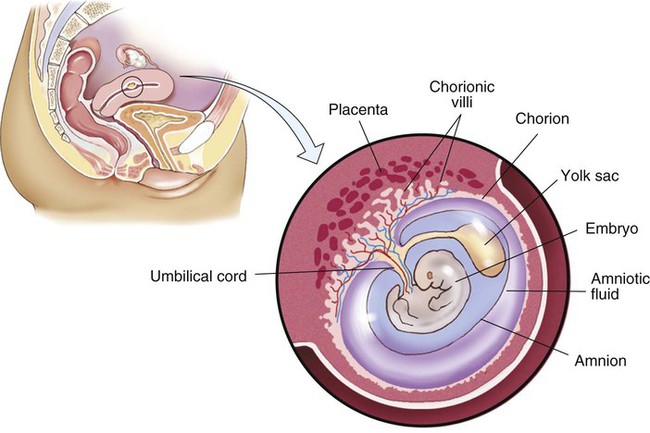
At the same time that the embryo is developing, extraembryonic membranes are forming to sustain the pregnancy. Two of these, the amnion and the chorion, form the inner and outer sacs that contain the embryo (Fig. 7-4). The outer sac, the chorion, forms part of the placenta, a highly vascular structure that acts as a physical communication between the mother and the embryo. The chorionic villi are small projections that extend from the outer sac to provide a maximum amount of contact with the maternal blood supply. The inner sac, the amnion and its amniotic fluid, cushion the embryo, protect it against temperature changes, and allow it to move. On the outer side, the amniotic sac is connected to the yolk sac, the allantois, and to the placenta by way of the umbilical cord. The yolk sac, attached to the developing embryo, provides a source of nutrition for the early stage of development. The allantois is an embryonic structure that assists in waste removal and gas exchange. It later develops into the placenta and umbilical cord, which share similar functions. The umbilical cord is the tissue that connects the embryo to the placenta (and hence to the mother). When the baby is delivered, the umbilical cord is cut, and the baby is then dependent on his/her own body for all physiological processes. The remaining “scar” is the umbilicus, or navel.
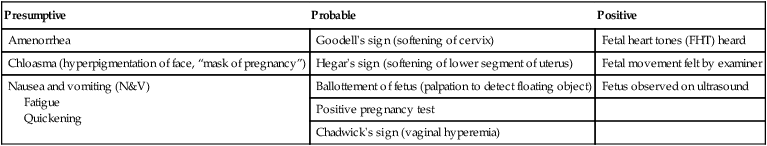
| Presumptive | Probable | Positive |
| Amenorrhea | Goodell’s sign (softening of cervix) | Fetal heart tones (FHT) heard |
| Chloasma (hyperpigmentation of face, “mask of pregnancy”) | Hegar’s sign (softening of lower segment of uterus) | Fetal movement felt by examiner |
| Nausea and vomiting (N&V) Fatigue Quickening |
Ballottement of fetus (palpation to detect floating object) | Fetus observed on ultrasound |
| Positive pregnancy test | ||
| Chadwick’s sign (vaginal hyperemia) |
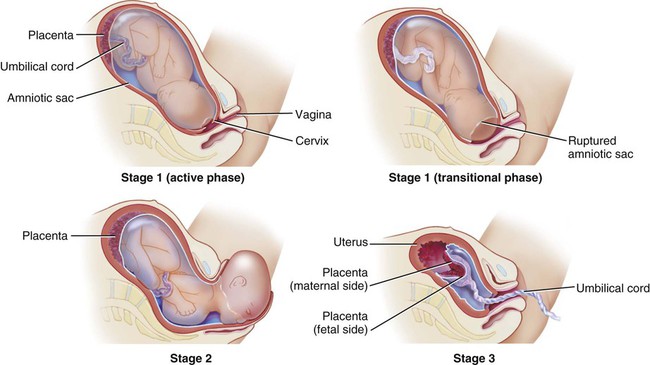
Stages of labor: Like the trimesters, labor is also divided into three stages: first, second, and third (Fig. 7-5). The first stage is the longest and, again, includes three parts: an early (or latent) phase, an active phase, and a transitional phase. The early phase, the longest, is marked by dilation of the cervix to approximately 4 centimeters and a changeover from irregular to regular contractions. The active phase has the now regular contractions becoming stronger and closer together. The final phase of the first stage, the transition phase, is the time when the cervix dilates to 10 centimeters and the baby moves down into the birth canal. The second stage is the time when the actual birth takes place and the umbilical cord is cut and clamped. The third stage is the delivery of the placenta.
17. A woman who has been pregnant two or more times is termed a/an ________________________________.
18. Once the fertilized egg has implanted in the uterine wall it is called a/an ___________________________.
19. Fraternal twins are called _____________ twins, whereas identical twins are called _____________ twins.
20. A developing fertilized egg is called a/an ___________ in its first 2 weeks, a/an __________ in weeks 3 to 8, and a/an ____________ for the remainder of the pregnancy.
21. The inner sac that contains the embryo is called the _____________, whereas the outer sac is called the ________________________________________________________________________________________________.
22. The tissue that connects the embryo to the placenta is called the __________________________________.
23. __________________ is the term for the act of giving birth.
24. A nullipara has delivered how many babies? ______________________________________________________
25. LGA stands for _____________________ and SGA stands for _________________________________________.
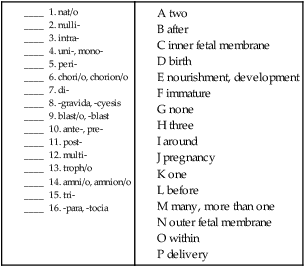
Combining Forms for the Anatomy and Physiology of Pregnancy
| Meaning | Combining Form |
| amnion, inner fetal sac | amni/o, amnion/o |
| birth | nat/o |
| chorion, outer fetal sac | chorion/o, chori/o |
| development, nourishment | troph/o |
| embryonic, immature | blast/o |
| parturition, delivery | part/o |
| placenta | placent/o |
| pregnancy | gravid/o |
| umbilicus | umbilic/o, omphal/o |
Prefixes for the Anatomy and Physiology of Pregnancy
| Prefix | Meaning |
| ante- | before |
| di- | two |
| intra- | within |
| mono- | one |
| multi- | many |
| neo- | new |
| nulli- | none |
| peri- | around |
| post- | after |
| pre- | before |
| primi- | first |
Suffixes for the Anatomy and Physiology of Pregnancy
| Suffix | Meaning |
| -blast | embryonic, immature |
| -cyst | sac |
| -gravida, -cyesis | pregnancy |
| -para, -tocia | delivery |
Pathology
Terms Related to Pregnancy with Abortive Outcome (OØØ-OØ8)
| Term | Word Origin | Definition |
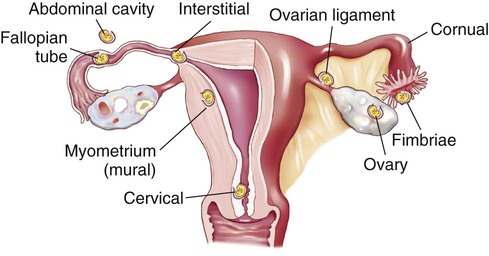
| ectopic pregnancy | ec- out top/o place -ic pertaining to |
Implantation of the embryo in any location but the uterus (Fig. 7-6). |
| hydatidiform mole | hydatid/i water drop -form shape |
Rare, cystlike growth of a nonviable embryo (Fig. 7-7). |
| miscarriage/abortion | Termination of a pregnancy before the fetus is viable. If spontaneous, it may be termed a miscarriage or a spontaneous abortion. If induced, it can be referred to as a therapeutic abortion. A missed abortion is fetal death <20 weeks with retention of the dead fetus. An incomplete abortion includes the retained products of conception after a spontaneous abortion. |
Terms Related to Edema, Proteinuria, and Hypertensive Disorders in Pregnancy, Childbirth, and the Puerperium (O1Ø-O16)
| Term | Word Origin | Definition |
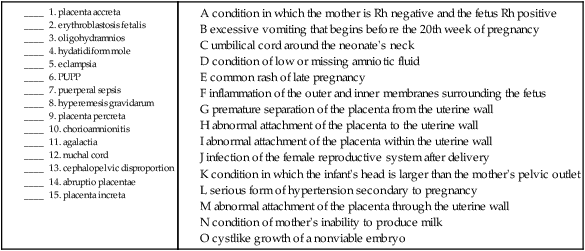
| eclampsia in pregnancy | Extremely serious form of hypertension secondary to pregnancy. Patients are at risk from coma, convulsions, and death. | |
| gestational edema | edema swelling | An abnormal accumulation of fluid in the body limited to the pregnancy time period. |
| HELLP syndrome | hem/o blood -lysis breaking down |
Preeclampsia with hemolysis (destruction of blood cells), elevated liver enzymes, and low platelet count. |
| preeclampsia | pre- before | Abnormal condition of pregnancy with unknown cause, marked by hypertension, edema, and proteinuria. Also called toxemia of pregnancy. |
Terms Related to Other Maternal Disorders Predominantly Related to Pregnancy (O2Ø-O29)
| Term | Word Origin | Definition |
| gestational diabetes mellitus | Abnormally high blood glucose levels during pregnancy in women with normal blood glucose levels. | |
| gestational phlebitis | phleb/o vein -itis inflammation |
Inflammation of veins during pregnancy. |
| hyperemesis gravidarum | hyper- excessive -emesis vomiting gravidarum pregnancy |
Excessive vomiting that begins before the 20th week of pregnancy. |
| pruritic urticarial papules and plaques (PUPP) | prurit/o itching -ic pertaining to |
A common rash of late pregnancy with itchy wheals, papules (bumps), and plaques (patches) that develop on the abdomen, breasts, arms, and legs (Fig. 7-8). |
Terms Related to the Fetus and Amniotic Cavity and Possible Delivery Problems (O3Ø-O48)
| Term | Word Origin | Definition |
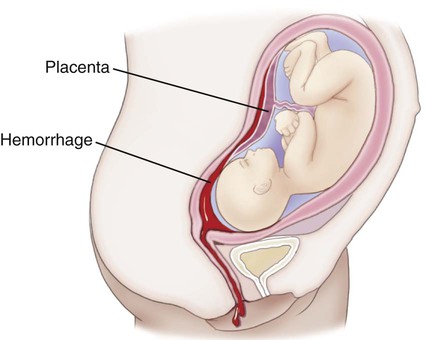
| abruptio placentae | Premature separation of the placenta from the uterine wall; may result in a severe hemorrhage that can threaten both infant and maternal lives. Also called ablatio placentae (Fig. 7-9). | |
| cephalopelvic disproportion | cephal/o head pelv/i pelvis -ic pertaining to |
Condition in which the infant’s head is larger than the pelvic outlet it must pass through, thereby inhibiting normal labor and birth. It is one of the indications for a cesarean section. |
| cervical incompetence | cervic/o cervix, neck -al pertaining to |
Lack of cervical closure during pregnancy. May lead to early termination of pregnancy. |
| chorioamnionitis | chori/o chorion amnion/o amnion -itis inflammation |
Inflammation of the outer and inner membranes (chorion and amnion) surrounding the fetus. |
| erythroblastosis fetalis | erythr/o red (blood cell) blast/o immature -osis abnormal condition |
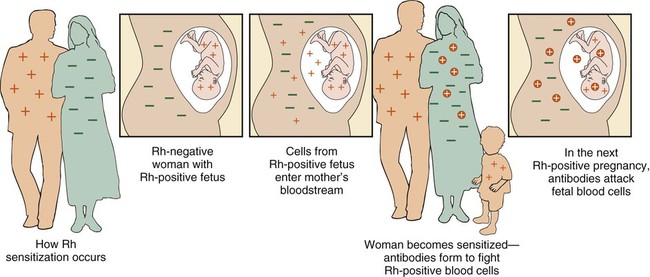
Condition in which the mother is Rh negative and her fetus is Rh positive, causing the mother to form antibodies to the Rh-positive factor. Subsequent Rh-positive pregnancies will be in jeopardy because the mother’s anti-Rh antibodies will cross the placenta and destroy fetal blood cells (Fig. 7-10). |
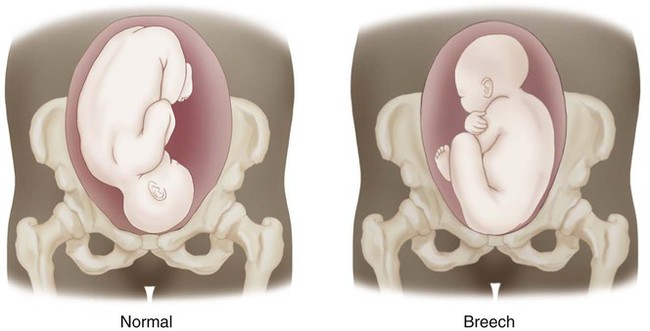
| malpresentation of fetus | mal- bad, abnormal | Any fetal position but cephalic for birth. A breech presentation is an example (Fig. 7-11). |
| oligohydramnios | olig/o scanty hydr/o water, fluid -amnios amnion |
Condition of low or missing amniotic fluid. |
| placenta accreta | ac- toward cret/o to grow -a noun ending |
An abnormal attachment of the placenta to the uterine wall. |
| placenta increta | in- in cret/o to grow -a noun ending |
An abnormal attachment of the placenta within the uterine wall. |
| placenta percreta | per- through cret/o to grow -a noun ending |
An abnormal attachment of the placenta through the uterine wall. |
| placenta previa | previa in front of | Placenta that is malpositioned in the uterus, so that it covers the opening of the cervix. |
| placentitis | placent/o placenta -itis inflammation |
Inflammation of the placenta. |
| polyhydramnios | poly- excessive, many hydr/o water, fluid -amnios amnion |
Condition of excessive amniotic fluid. |
| twin-to-twin transfusion syndrome (TTTS) | Complication of blood supply with one twin receiving a deficient amount (the donor) and other receiving too much (the recipient). |
Terms Related to Complications of Labor and Delivery (O6Ø-O77)
| Term | Word Origin | Definition |
| dystocia | dys- abnormal, difficult -tocia delivery |
Abnormal or difficult childbirth. Meconium staining (fetal defecation in utero) indicates fetal distress that may accompany dystocia. |
| nuchal cord | nuch/o neck -al pertaining to |
Abnormal but common occurrence of the umbilical cord wrapped around the neck of the neonate. |
Terms Related to Complications Predominantly Related to the Puerperium (O85-O92)
| Term | Word Origin | Definition |
| agalactia | a- without galact/o milk -ia condition |
Condition of mother’s inability to produce milk. |
| galactorrhea | galact/o milk -rrhea flow, discharge |
Abnormal discharge of milk. |
| hypogalactia | hypo- deficient, below galact/o milk -ia condition |
Abnormally low production of milk. |
| puerperal sepsis | puerper/o puerperium -al pertaining to sepsis infection |
Infection of female reproductive system after delivery. |
Terms Related to Malignant Neoplasms (C58)
| Term | Word Origin | Definition |
| choriocarcinoma | chori/o chorion -carcinoma cancer of epithelial origin |
A malignant tumor arising from the chorionic membrane surrounding the fetus. |
16. choriocarcinoma ________________________________________________________________________________
17. hypogalactia ____________________________________________________________________________________
18. polyhydramnios _________________________________________________________________________________
19. placentitis ______________________________________________________________________________________
Procedures
Terms Related to Prenatal Diagnosis
| Term | Word Origin | Definition |
| alpha fetoprotein (AFP) test | Maternal serum (blood) alpha fetoprotein test performed between 14 and 19 weeks of gestation; may indicate a variety of conditions, such as neural tube defects (spina bifida is the most common finding) and multiple gestation. | |
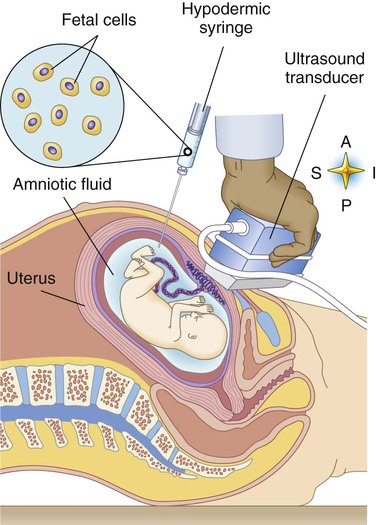
| amniocentesis | amni/o amnion -centesis surgical puncture |
Removal and analysis of a sample of the amniotic fluid with the use of a guided needle through the abdomen of the mother into the amniotic sac to diagnose fetal abnormalities (Fig. 7-12). |
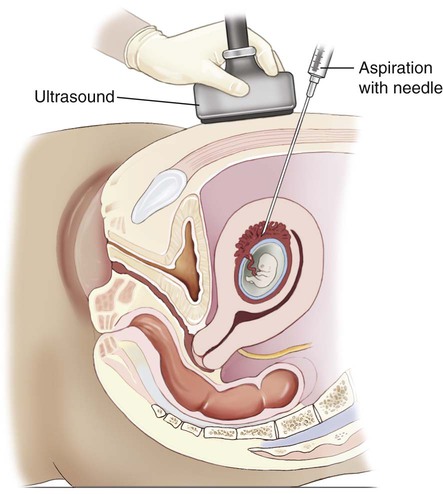
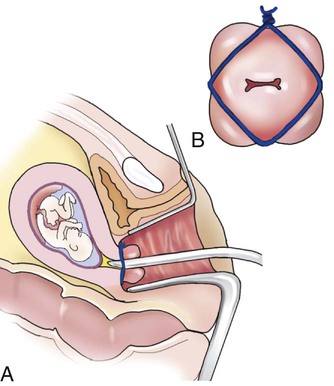
| chorionic villus sampling (CVS) | chorion/o chorion -ic pertaining to |
Removal of a small piece of the chorionic villi that develop on the surface of the chorion, either transvaginally or through a small incision in the abdomen, to test for chromosomal abnormalities (Fig. 7-13). |
| contraction stress test (CST) | Test to predict fetal outcome and risk of intrauterine asphyxia by measuring fetal heart rate throughout a minimum of three contractions within a 10-minute period. | |
| nonstress test (NST) | The fetus is monitored for a normal, expected acceleration of the fetal heart rate. A reactive nonstress test should be followed by a CST and possible ultrasound studies. | |
| pelvimetry | pelv/i pelvis -metry measuring |
Measurement of the birth canal. Types of pelvimetry include clinical and x-ray, although x-ray pelvimetry is not commonly done. |
| pregnancy | Test available in two forms: a standard over-the-counter pregnancy test, which examines urine for the presence of hCG; and a serum (blood) pregnancy test performed in a physician’s office or laboratory to get a quantitative hCG. A “triple screen” is a blood test for hCG, AFP, and uE3 (unconjugated estradiol). |
Terms Related to Pregnancy and Delivery Procedures
| Term | Word Origin | Definition |
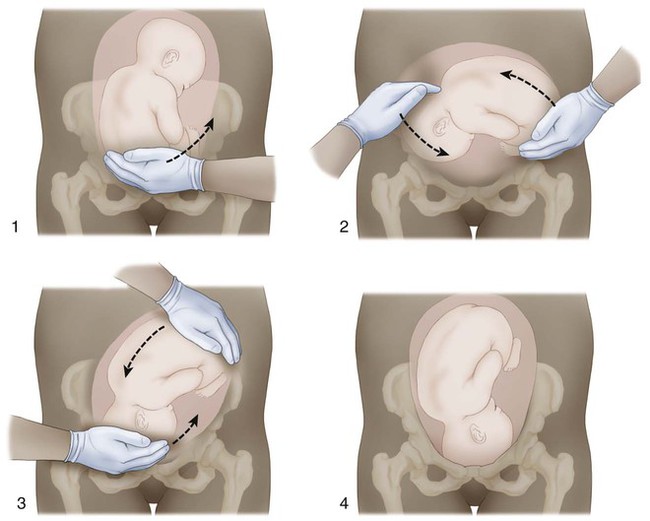
| cephalic version | cephal/o head –ic pertaining to version turning |
Process of turning the fetus so that the head is at the cervical outlet for a vaginal delivery (Fig. 7-14). |
| cerclage | Suturing the cervix closed to prevent a spontaneous abortion in a woman with an incompetent cervix. The suture is removed when the pregnancy is at full term to allow the delivery to proceed normally (Fig. 7-15). | |
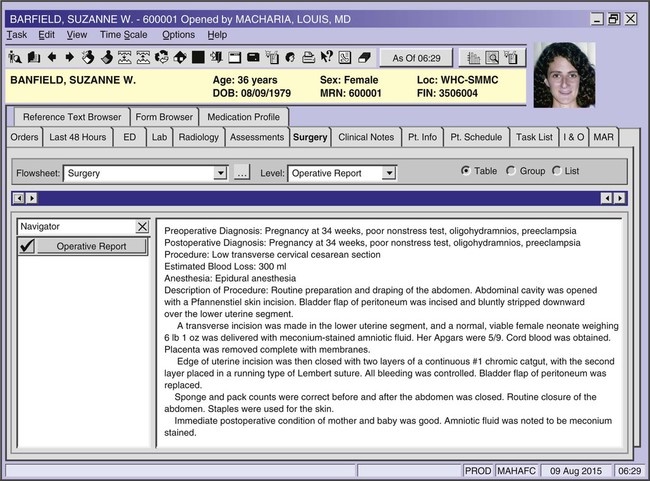
| cesarean section (C-section, CS) | Delivery of an infant through a surgical abdominal incision (Fig. 7-16). | |
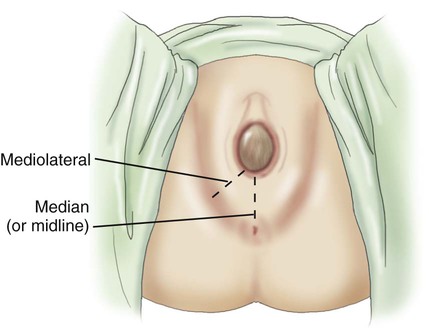
| episiotomy | episi/o vulva -tomy cutting |
Incision to widen the vaginal orifice to prevent tearing of the tissue of the vulva during delivery (Fig. 7-17). |
| vaginal birth after C-section (VBAC) | vagin/o vagina -al pertaining to |
Delivery of subsequent babies vaginally after a C-section. In the past, women were told “once a C-section, always a C-section.” Currently, this is being changed by recent developments in technique. |
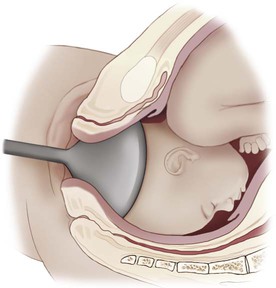
| vaginal delivery | vagin/o vagina -al pertaining to |
(Usually) cephalic presentation (head first) through the vagina. Feet or buttock presentation is a breech delivery. Assistance may include instruments, such as forceps or vacuum extraction (Fig. 7-18). |
6. amniocentesis ___________________________________________________________________________________
7. episiotomy ______________________________________________________________________________________
8. pelvimetry ______________________________________________________________________________________
Pharmacology
Contraceptive Management
abortifacient: Medication that terminates pregnancy. Mifepristone (Mifeprex) and dinoprostone (Prostin E2) may be used as abortifacients.
abstinence: Total avoidance of sexual intercourse as a contraceptive option.
barrier methods: See diaphragm and cervical cap.
birth control patch: Timed-release contraceptive worn on the skin that delivers hormones transdermally.
cervical cap: Small rubber cup that fits over the cervix to prevent sperm from entering.
contraceptive sponge: Intravaginal barrier with a spermicidal additive.
diaphragm: Soft, rubber hemisphere that fits over the cervix, which can be lined with a spermicidal lubricant prior to insertion.
emergency contraception pill (ECP): Medication that can prevent pregnancy after unprotected vaginal intercourse; does not affect existing pregnancies or cause abortions. Plan B is a popular brand-name ECP that is now available OTC behind the counter. Commonly called the “day-after pill.”
female condom: Soft, flexible sheath that fits within the vagina and prevents sperm from entering the vagina.
hormone implant: Timed-release medication placed under the skin of the upper arm, providing long-term protection. The Norplant system is an example.
hormone injection: Contraceptive hormones such as Depo-Provera that may be given every few months to provide reliable pregnancy prevention.
intrauterine device (IUD): Small, flexible device inserted into the uterus that prevents implantation of a zygote (Fig. 8-26).
male condom: Soft, flexible sheath that covers the penis and prevents sperm from entering the vagina. If may also be coated with a spermicide.
oral contraceptive pill (OCP) or birth control pill (BCP): Pill containing estrogen and/or progesterone that is taken daily to fool the body into thinking it is pregnant, so that ovulation is suppressed.
procreative and contraceptive management: Term for a variety of medications and techniques that describe the options available for women’s reproductive health.
rhythm method: A natural family planning method that involves charting the menstrual cycle to determine fertile and infertile periods.
spermicides: Foam or gel applied as directed prior to intercourse to kill sperm.
vaginal ring: Flexible ring containing contraceptive hormones inserted into the vagina to prevent pregnancy.
Fertility Drugs
bromocriptine (Parlodel): Oral medication typically used with in vitro fertilization to reduce prolactin levels (which suppresses ovulation).
clomiphene (Clomid, Serophene): Oral medication that stimulates the pituitary gland to produce the hormones that trigger ovulation.
gonadotropin-releasing hormone (GRH) agonist (Lupron): Agent injected or inhaled nasally to prevent premature release of eggs.
human chorionic gonadotropin (hCG) (Novarel): Hormone given intramuscularly to trigger ovulation, typically administered with another hormone that will stimulate the release of developed eggs.
human menopausal gonadotropins (hMG) (Repronex): Dual gonadotropins that both stimulate the production of egg follicles and cause the eggs to be released once they are developed. These are given by intramuscular or subcutaneous injection.
lutropin alfa (Luveris): A gonadotropin that stimulates the production of egg follicles.
urofollitropin (Bravelle): Hormone given subcutaneously that mimics follicle-stimulating hormone (FSH) to directly stimulate the ovaries to produce egg follicles.
Drugs to Manage Delivery
oxytocic: Medication given to induce labor by mimicking the body’s natural release of the oxytocin hormone or to manage postpartum uterine hemorrhage. Oxytocin (Pitocin) is the most commonly used agent to induce labor. Other available oxytocic agents are methylergonovine (Methergine) and ergonovine (Ergotrate).
tocolytic: Medication given to slow down or stop preterm labor by inhibiting uterine contractions. Various drugs such as magnesium sulfate, terbutaline (Brethine), nifedipine (Procardia), or indomethacin (Indocin) may be used for this purpose.
Recognizing Suffixes for PCS
Suffixes and Root Operations for Pregnancy, Childbirth, and the Puerperium
| Suffix | Root Operation(s) and Categories |
| -centesis | Drainage (products of conception) |
| -metry | Measurement |
| -tomy | Division |
| Abbreviation | Definition |
| AFP | alpha fetoprotein test |
| CS | cesarean section |
| CST | contraction stress test |
| CVS | chorionic villus sampling |
| EDD | estimated date of delivery |
| FHT | fetal heart tones |
| hCG | human chorionic gonadotropin |
| HELLP | hemolytic elevated liver enzymes low platelet |
| LGA | light for gestational age |
| LMP | last menstrual period |
| N&V | nausea and vomiting |
| NST | nonstress test |
| PUPP | pruritic urticarial papules and plaques |
| Rh | Rhesus factor |
| SGA | small for gestational age |
| TTTS | twin-to-twin transfusion syndrome |
| uE3 | unconjugated estradiol |
| VBAC | vaginal birth after C-section |




 pounds and is 18 inches long. At this time, the pregnancy is considered to be at term. ICD-10 classifies late pregnancies as post-term pregnancy (from 40 to 42 completed weeks) and prolonged pregnancy (over 42 weeks).
pounds and is 18 inches long. At this time, the pregnancy is considered to be at term. ICD-10 classifies late pregnancies as post-term pregnancy (from 40 to 42 completed weeks) and prolonged pregnancy (over 42 weeks).