4 Practical pharmacology in paediatric emergencies
Do not skip this chapter! It is not mind-numbing pharmacology and should offer some useful tips on drug dosing in paediatric emergency management. (Please refer to Chapters 5 and 6 for drug dosing tables.)
Pharmacokinetics in critical illness
• Hypoxaemia as well as poor perfusion leads to decreased or unpredictable drug absorption from the GIT. This, in addition to variable first pass metabolism, is one of the reasons that intravenous administration is favoured to ensure optimum bioavailability of the drug.
• Rectal absorption can vary because of hypoperfusion and depending on how high in the rectum the medication is administered – higher up means absorption into the portal system and a greater enterohepatic first pass metabolism with a resultant decreased bioavailability. Drugs administered low in the rectum are delivered systemically via the inferior and middle rectal veins, before passing through the liver.
• Hepatic and renal function may be impaired because of decreased cardiac output, leading to diminished clearance of drugs and prolonged duration of action.
• Significant oedema may change the volume of distribution of hydrophilic drugs.
Pharmacokinetics in the developing human
• Changes in volume of distribution – neonates have a relatively higher proportion of body water, which reaches adult levels before 1 year of age.
• Changes in plasma protein levels – these reach adult levels in early infancy.
• Changes in drug metabolizing enzyme systems – Phase I and Phase II liver enzymes reach adult levels of function by about 2 years of age (with much variation between individual enzymes).
• Changes in renal function – glomerular filtration rate and drug excretion reach adult levels at about 1 year of age.
Methods of estimating drug doses in children
Dose modification for developmental stage, critical illness and abnormal body composition
Developmental stage
• Drug doses for neonates and infants may need to be relatively higher in mg/kg values than for older children – be prepared to repeat a dose or to administer slightly higher doses than expected. On the contrary, drugs are cleared more slowly and so have a longer duration of action. Repeated drug doses must be given at longer intervals and infusions administered at slower rates than for older children.
• Percutaneous absorption of medications is much higher in infants and neonates (and even more so in preterm neonates) than older children and adults. Toxicity from dermal application of medication is a real danger in this group.
• Rectal administration of drugs in neonates and infants is subject to variable absorption and metabolism and should be used with care.
• Children of 2 to 6 years of age appear to clear drugs more rapidly than other developmental ages. Higher doses and shorter dosing intervals or higher infusion rates may be required in this group.
Critical illness
• Critically ill children often have renal dysfunction. The doses of drugs that are excreted via the kidneys should therefore be reduced for subsequent doses.
• Hepatic dysfunction should also be taken into account. Enzymes for Phase I and II reactions will be hindered in their functioning, leading to a decreased metabolism of certain drugs as well as decreased perfusion of the liver, which again affects subsequent doses rather than the initial one.
• Acidosis impedes the body’s ability to respond to catecholamines. Higher doses of these vasoactive drugs may be required in this setting, or the acidosis may require aggressive treatment.
Obesity
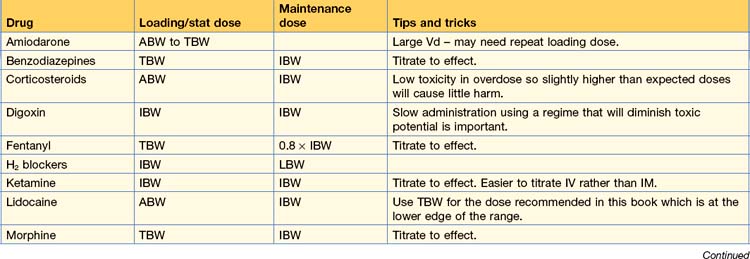
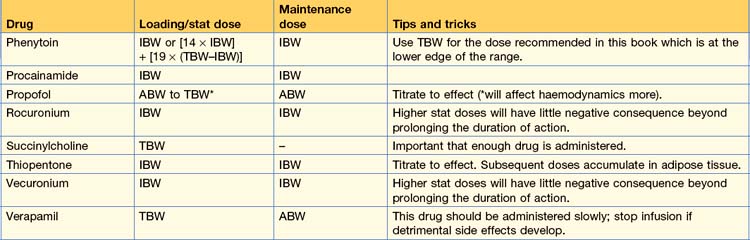
• Hydrophilic drugs – dose according to IBW or ABW in the obese patient, e.g. phenytoin, rocuronium, adrenaline, sodium bicarbonate.
• Lipophilic drugs – dose according to TBW, e.g. amiodarone, benzodiazepines, carbamazepine.
• Ventilator weight – There is no evidence to support which is the appropriate weight to use in obese children who are being ventilated. By extrapolating from adult studies, the most rational approach to ventilation in children would be to calculate tidal volume at 6 mL/kg using IBW or tape predicted weight based on length.
1. Fortunately, there is little need to modify drug dosages for stat administration. Always use TBW for an initial drug dose if there is any doubt, and administer it slowly while observing for the desired clinical effect. Don’t let thoughts about dose modification impair your ability to manage the patient in an emergency– the paralysis by indecision of cognitive overload.
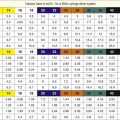
2. Use a tape-based weight prediction rather than any other form of weight estimation – it will probably offer the best indication of correct dosing. A system like the PAWPER tape will offer the best weight estimation and the least chance of under- or overdosing both in children with a higher and a lower than average weight-for-length.
3. Use a PAWPER tape-based weight estimation (with a habitus score of 5) for obese children – this will offer a weight close to an ABW and will pose little danger of overdosing.
4. Before subsequent doses are due in the ED or ICU there will be time to obtain a measured TBW, calculate IBW and plan the strategy for further dosing.