Postural alignment
What is postural alignment?
Postural alignment refers to the relationship between body segments and in basic terms refers to the structure of the musculoskeletal system, bones, joints and muscles. The alignment of the musculoskeletal system, within normal limits, is important in terms of minimizing stresses on soft tissue, minimizing muscle effort and providing sensory information to the centres involved in motor control (the control of movement). Hence, the musculoskeletal alignment plays a significant role in facilitating efficient movement during functional activities (Lennon 2003; Mayston 2000a,b; Carr and Shepherd 2003).
The importance of sensory feedback to successful motor control is well established (Kandel et al. 2000), with all decisions made by the nervous system being based upon the sensory feed forward/feedback it receives. A successful outcome is therefore reliant upon receiving sufficient accurate sensory information, a large amount of which comes from the somatosensory receptors (S3.23) embedded in the musculoskeletal system. In the main, this information relates to proprioception (S3.23), joint and muscle position and movement sense. Therefore it is the alignment of the musculoskeletal system which informs the nervous system of its present state for the planning of movement and also its ongoing state during movement when outcome can be monitored.
Why do I need to assess postural alignment?
A deviation from the most efficient alignment of the musculoskeletal system can occur as a direct effect of various neurological impairments, e.g. as a result of hypertonia, hypotonia (S3.21); pain (S3.29); weakness (S3.30) or altered sensation (S3.23). The malalignment of one body segment may also produce further deviations from normal range in other segments. For example, hypotonia involving the shoulder complex will directly result in reduced stability at the glenohumeral joint and possibly a subluxation. However, the changes in biomechanics will also immediately influence the alignment of both the upper limbs and the trunk as the patient finds strategies to compensate and remain balanced. The extra effort required to move and the stresses on soft tissue may later produce pain which will further limit the biomechanics of the movement. Over time, soft tissue adaptation occurs and the new compensatory strategies become learned via the physiological processes of neuroplasticity (Ungerleider et al. 2002; Marrone 2007).
How do I assess postural alignment?
Observation
As the patterns of musculoskeletal alignment are similar for posture and movement, the initial assessment can be carried out in a static posture. The assessment of alignment during movement is covered in the second part of the objective assessment section whereby the therapist performs a movement analysis of a functional task (S3.18).
Therapist
1. Where possible each of the main joints should be observed individually. This is necessary in order to establish the specific location of any deviation. For example, recording protraction at the shoulder complex is insufficient, as protraction involves a combination of movements at the glenohumeral joint, sternoclavicular and acromioclavicular joint and scapulothoracic joint. In order to target treatment effectively, the alignment of each should be evaluated.
2. The therapist should observe the alignment of all the body segments from all directions (in front, behind and from the side) taking into account all aspects of the segment orientation (anterior/posterior, superior/inferior, medial/lateral and rotation). Observing from different directions will allow the therapist to confirm the location of a deviation and its orientation/relationship with other segments.
3. The therapist may gain clues related to any deviation by observing or palpating:
4. The orientation of each segment can be noted using descriptors based on the physiological movements possible at the joint. For example, when evaluating the hip joint, the descriptors available would be flexion, extension, abduction, adduction, medial and lateral rotation.
Is the segment orientated in a neutral position?
Is the segment symmetrical in relation to a bilateral structure (e.g. the scapulas), to a midline structure (e.g. spinous processes) and to structures above and below?
Is the posture itself having any influence on segment alignment? Certain postures will impose deviations and should be recorded (e.g. hip flexion in sitting) but should not influence analysis. However, if the response bilaterally is not symmetrical (e.g. left hip is externally rotated and abducted in relation to the right), then further analysis is recommended.
Recording
When recording the findings there are a few viable options to choose from. Namely:
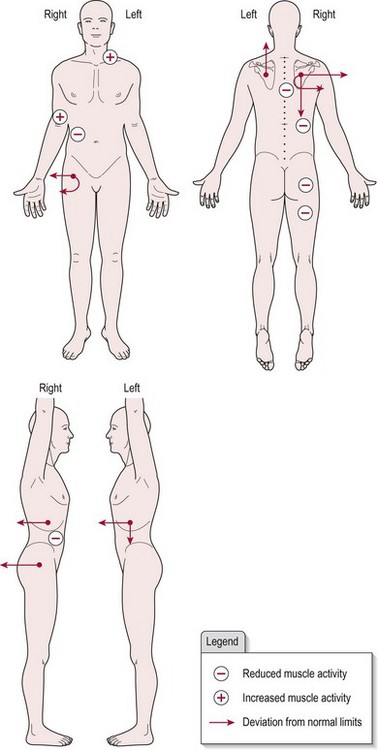
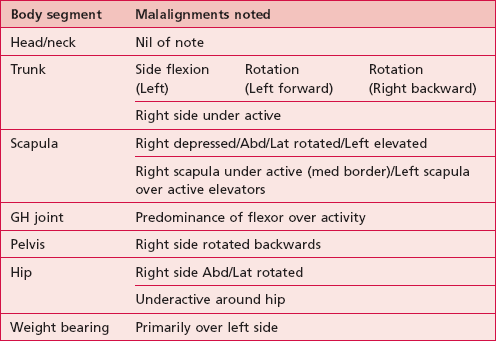
• Body chart (see Fig. 20.3). Remember that when using a body chart include a key to identify the symbols used and before adding data to the chart, label left and right on each figure to avoid mistakes
Analysis
Example
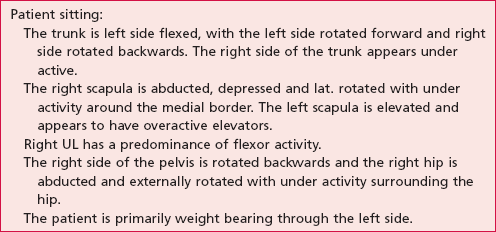
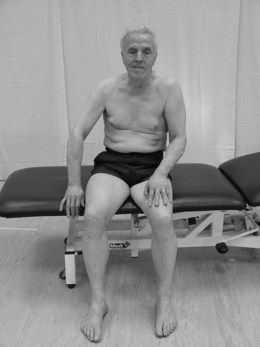
The body chart (Fig. 20.3) represents patient X shown in Figures 20.1 and 20.2 who has suffered a right hemiplegia. Following analysis of all the objective markers and examination of the body chart the following is hypothesized. The right pelvis, hip, trunk and shoulder complex are seen to be rotated backwards probably due to hypotonia. In response, the patient works harder with the left side, especially the shoulder complex (elevation) and forward trunk rotation in an attempt to maintain an upright posture against gravity. The latter is a normal response to the deviation imposed by the hypotonia on the right. Therefore treatment would be most effective aimed at the hypotonia with the assumption that the compensatory activity would then no longer be required.
Outcome measures
References and Further Reading
Carr, J, Shepherd, R. Stroke rehabilitation guidelines for exercise and training to optimize motor skill. Edinburgh: Butterworth-Heinemann; 2003.
Kandel, ER, Schwartz, JH, Jessell, TM. Principles of neural science, ed 4. New York: McGraw-Hill Health professions Division; 2000.
Lennon, S. Physiotherapy practice in stroke rehabilitation: a survey. Disability and Rehabilitation. 2003; 259:455–461.
Marrone, DF. Ultrastructural plasticity associated with hippocampal learning: a meta analysis. Neurobiology of Learning and Memory. 2007; 873:361–371.
Mayston, M. Handling and spasticity letter to the editor. Physiotherapy. 2000; 86:559.
Mayston, M. Compensating for CNS dysfunction letter to the editor. Physiotherapy. 2000; 86:612.
SiliconCOACH. SiliconCOACH coaching solutions for a digital age [online]. New Zealand www.siliconcoach.com, 2004. [(Accessed 1 September 2006)].
Ungerleider, LG, Doyon, J, Karni, A. Imaging brain plasticity during motor skill learning. Neurobiology of Learning and Memory. 2002; 783:553–564.