Chapter 7 Postoperative Pain Relief
Introduction and background
The goal of postoperative pain relief is to achieve optimal analgesia, facilitating a quick return to normal activities with minimal side effects. In addition, the effective treatment of acute postoperative pain may reduce the incidence of chronic pain after surgery. Acute postoperative pain differs from chronic or cancer pain because it is more transitory and there may be an affective component relating to anxiety about the outcome of the surgical procedure and concern for suboptimal analgesia. Studies have shown that for patients awaiting surgery the possibility of severe acute postoperative pain is a major concern.1 In addition, uncontrolled postoperative pain can lead to delayed recovery from surgery, pulmonary dysfunction and hypoxia, together with restriction of mobility and subsequent increased risk of thromboembolism. Surveys in the UK, the USA and Europe have identified an unacceptable prevalence of poor pain control after surgery.2,3 However, in recent years the introduction of acute pain management services in hospitals has promoted improvements in postoperative pain.4 In addition, the use of ‘multimodal’ or ‘balanced’ analgesia – a combination of opiates, non-steroidal antiinflammatory drugs (NSAIDs), local anaesthetics and other adjuvants have been recommended to manage postoperative pain. Recently, White and Power reviewed the evidence for such pain management. They showed that multimodal analgesia improves the efficacy of pain relief, decreases the risk of side effects and is an evidence-based, established effective strategy for postoperative pain management.5,6
Measurement of pain
In adults, three common methods of self-reported pain measurement are used.
Visual analogue scale
The visual analogue scale (VAS) uses a 10 cm line with endpoint descriptors such as ‘no pain’ marked at the left end of the line and ‘worst pain imaginable’ marked at the right end (Fig. 7.1). Patients are asked to mark a point on the line that best represents their pain. The distance from ‘no pain’ to the patient’s mark is then measured and this equals the VAS score.
Available methods of pain relief
Paracetamol
Oral paracetamol
Paracetamol is well absorbed from the proximal small bowel and is not subject to significant first-pass metabolism in the liver, with oral bioavailability estimated at between 63% and 89% in adults. Because paracetamol does not cause gastric irritation, is relatively non-toxic in therapeutic doses and has minimal side effects, it should be considered as the basic building block of most postoperative analgesic regimens. Paracetamol is considered an effective and well-tolerated agent in the management of mild to moderate pain and, as it has none of the renal or cardiovascular side effects that characterize antiinflammatory drugs, it can be used in both NSAID and opioid-sparing roles. Studies have shown that paracetamol combined with patient-controlled analgesia (PCA) morphine induces a significant morphine-sparing effect of the order of 20% in the first 24 h.7 However, this is not associated with a reduction in morphine-related side effects. Combining paracetamol with NSAIDs appears to result in a synergistic interaction but so far there is only limited evidence that this interaction is advantageous in the clinical setting.
Parental paracetamol
An intravenous formulation of paracetamol is now available in the UK which facilitates its administration in patients under anaesthesia (or who cannot swallow) before the end of surgery, with the aim of reducing opioid-induced sedation and respiratory depression in the recovery room. The recommended dose of paracetamol is 15 mg/kg, with a maximum daily dose of 60 mg/kg. Peak plasma concentration (Cmax) is achieved approximately 25 min after a 1 g intravenous infusion compared to 45 min after 1 g orally. Clinically this difference has been shown to lead to a quicker onset of analgesia. Several recent studies have looked at the use of an initial loading dose of paracetamol of 2 g to improve early postoperative analgesia, with conflicting results.8 In our practice we routinely give a 1 g dose of i.v. paracetamol at the start of surgery.
Non-steroidal antiinflammatory drugs
Postoperative analgesia comparable with that of opioids has been demonstrated with NSAIDs. An opioid-sparing effect of the order of 30–50% has also been observed with NSAIDs, as well as a reduction in opioid-induced nausea, vomiting and respiratory depression. This reduction in opioid requirement and side effects may benefit the patient by producing increased postoperative analgesia and potentially reducing hospital stay.9
Summary Box 7.2 Side effects of NSAIDs
| Gastrointestinal | Gastric erosions |
| Renal | Decreased renal blood flow |
| Acute renal failure | |
| Haematological | Prolonged bleeding time |
| Respiratory | Bronchospasm |
| Others | Skin rashes |
Adverse effects/complications
Haematological
Aggregation of platelets depends on a balance between prostacyclin (from endothelial cells) and thromboxane A2 (from platelets). The former is a vasodilator and inhibits platelet aggregation; the latter is a vasoconstrictor which stimulates platelet aggregation. NSAIDs inhibit the synthesis of both these factors and the net balance will determine the tendency to bleed. NSAIDs also inhibit platelet COX, although the effect lasts only as long as the drug remains in the blood (five half-lives). An increase in operative bleeding has been reported as a result of the use of NSAIDs and surgeons should be aware of this risk. A meta-analysis of several randomized controlled trials showed a higher risk of postoperative bleeding after tonsillectomy with the postoperative use of NSAIDs.10 However, others have disagreed with this analysis, citing poor surgical technique and that in some patients the bleeding occurred at a time when the drug had been eliminated from the body.11
Cox-2 inhibitors
In an effort to minimize the potential for bleeding at the surgical site and to reduce the incidence of serious gastrointestinal adverse effects and renal dysfunction associated with traditional NSAIDs, selective COX-2 inhibitors, also named ‘coxibs’, such as rofecoxib and celecoxib, were developed . Other novel COX-2 inhibitors with improved biochemical selectivity recently developed include etoricoxib, valdecoxib, parecoxib and lumiracoxib. These ‘coxibs’ have similar analgesic efficacy to that of NSAIDs, with reduced risk of bleeding and less gastrointestinal toxicity. However, large outcome and epidemiological studies suggest that while COX-2 inhibitors do confer improved gastrointestinal safety, they are not devoid of gastrointestinal effects during long-term use. Two of these drugs have already been withdrawn because of safety concerns: rofecoxib because of cardiovascular problems and valdecoxib because of serious subcutaneous adverse reactions.12
Concerns have also been raised regarding the increased incidence of thrombotic complications (leading to myocardial infarction and stroke) associated with selective COX-2 compounds.13 COX-2 inhibition with coxibs may increase the risk of vascular thrombus formation by upsetting the balance between pro- and anti-platelet aggregation effects: thromboxane A2 synthesis is primarily a COX-1-induced effect, and prostaglandin I2 synthesis a COX-2 effect.
Pre-emptive use
Analgesics given before surgical trauma are thought to have a pre-emptive effect. This implies that analgesia will start before the surgical stimulus, leading to a reduction of CNS input and hence reducing pain. This is commonly referred to as controlling the ‘wind-up’ phenomenon. There have been many studies done using different NSAIDs pre-emptively and, while there have been some mixed results (some showing a benefit, others showing no benefit), it is common practice in orthopaedic patients to commence NSAIDs pre-emptively either orally, sublingually or intravenously using standard drugs (naproxen, piroxicam, ibuprofen or diclofenac).14,15
Opiates
Opioid receptors
Summary Box 7.3 Side effects of opioids
| Respiratory | Respiratory depression |
| Central nervous system | Sedation, euphoria |
| Nausea and vomiting | |
| Cardiovascular | Vasodilation, bradycardia |
| Myocardial depression | |
| Genitourinary | Urinary retention |
| Gastrointestinal | Delayed gastric emptying |
| Constipation | |
| Pruritus |
Side effects (complications) of opioid drugs
All of the opioid drugs that we commonly use for pain management in the postoperative setting act primarily at the µ receptor sites and all have a fairly similar spectrum of side effects. In equianalgesic doses and in most patients, the incidence of side effects is generally very similar regardless of the opioid used (Table 7.1).
| 1. Respiratory | Respiratory depression |
| 2. Central nervous system | Sedation, euphoria (or dysphoria) |
| Nausea, vomiting, miosis, muscle rigidity | |
| 3. Cardiovascular | Vasodilatation, bradycardia, myocardial depression |
| 4. Pruritus | Common with morphine |
| 5. Genitourinary | Urinary retention |
| 6. Gastrointestinal | Delayed gastric emptying constipation |
| 7. Allergy | Allergic reactions to opioid drugs are very uncommon |
The most important side effects of opioids are respiratory depression, which may be severe and result in hypoxia. Sedation is routinely monitored postoperatively using a sedation score and, while respiratory rate is also monitored, it is routine practice to use continuous pulse oximetry in all postoperative patients in the recovery room or postanaesthetic care unit (PACU). Opioids are implicated as one of the risk factors in postoperative nausea and vomiting (PONV) and are assigned 1 point in the Apfel risk scoring system.16 In all cases where opioids are used intraoperatively or postoperatively, antiemetics should be given as prophylaxis. Combination antiemetic prophylaxis with drugs having different mechanisms of action have been shown in many studies to markedly reduce the incidence of PONV. Ondansetron and cyclizine have been shown to achieve a response rate of 95%.17
Patient-controlled analgesia
Effectiveness of PCA
Many studies have been carried out comparing PCA to conventional methods of analgesia. Systemic reviews in 1992 and 2001 (Acta Anaesth Scand 2001) found conflicting results regarding the effectiveness of PCA compared to traditional analgesia. However, a Cochrane review in 2007 of 55 studies involving a total of 3861 patients found that, overall, more patients were satisfied with the analgesia provided by the PCA pump. Also, pain intensity during the first 24 h was 8 points lower in the PCA group than in the group receiving conventional analgesia, 9 points lower between 25 and 48 h and 13 points lower between 49 and 72 h.18
Oral analgesics
Oxycodone
Oxycodone is a thebaine derivative and is used for the management of moderate to severe pain. A sustained-release preparation of oxycodone has been developed which has been shown to be very effective in postoperative pain relief. The biphasic pattern of absorption of the drug following oral administration results in an initial rapid absorption of approximately 40% of the dose, with rapid onset of analgesia (at about 1 h), which is then followed by sustained release of drug and stable plasma levels over a further 12 h period; therefore twice daily dosing is all that is required. A trial of this drug in orthopaedic patients showed that it provided effective analgesia, shortened hospital stay and reduced the frequency of analgesic administration after hip and knee arthroplasty.19
Adjuvant analgesic agents
A number of other adjuvant analgesic drugs, anticonvulsants, ketamine, clonidine, neostigmine and magnesium, have been shown in clinical trials to be useful in controlling postoperative pain.20 However, these modalities are not yet used in routine clinical practice and are best managed by specialist anaesthetists and pain medicine practitioners.
Local anaesthetic techniques
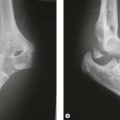
Intra-articular joint Injections/catheters
Intra-articular local anaesthetic infiltration has been used for many years in arthroscopic knee surgery with improved pain relief demonstrated in the postoperative period. Similarly in shoulder and elbow arthroscopies intra-articular injection of local anaesthetic appears superior to surgical wound infiltration. Intra-articular catheter techniques have recently been developed where at the end of surgery a 20-gauge catheter is inserted by the surgeon into the joint under direct visualization. Dilute solutions of local anaesthetics are then infused through the catheter postoperatively. While intra-articular local anaesthetic infiltration has the potential advantages of better preservation of motor function and technical simplicity, a study comparing this technique to perioperative interscalene block in shoulder surgery demonstrated superior analgesia in the interscalene group.21
Peripheral nerve blocks
Continuous peripheral nerve blocks
This technique involves the percutaneous insertion of a catheter directly adjacent to the peripheral nerve(s) innervating the surgical site (as opposed to a ‘wound’ catheter placed directly at a surgical site). Infusing local anaesthetic via the perineural catheter then provides potent, site-specific and continuous analgesia. Since the 1990s, advances in needle technology, placement techniques (e.g. nerve stimulators, ultrasound guidance) catheter design and infusion pump mechanics have resulted in widespread use of this technique. Particularly for painful shoulder surgeries, continuous perineural catheters provide superior analgesia, limit opioid-related side effects and improve patient satisfaction.22 This technology has also proven useful and safe for outpatient use using disposable elastomeric pumps.23
Clinical Pearl 7.2
Ultrasound-guided regional nerve block
The use of ultrasound guidance has become increasingly popular in regional anaesthesia over the past few years. The advantages of ultrasound guidance include the real-time visualization of anatomical structures and the spread of anaesthetic.24 Peripheral nerve stimulation relies on placing the needle close to the target nerve, but cannot make allowances for individual anatomical variation or reliably predict the spread of the local anaesthetic. Using high-resolution real-time ultrasound visualization during peripheral nerve block may further increase success rates, decrease latency of the block, reduce the volume of local anaesthetic used, shorten time to perform the blocks and has the potential to reduce or eliminate the risk of accidental intravascular or intraneural injection. A number of recent studies support these claims.
A study by Chan et al, reporting a retrospective analysis of 662 axillary blocks, found that in the ultrasound-guided group the block success rate was higher compared to the traditional group (91.6% versus 81.9%). The US-guided axillary block group also required a lower volume of local anaesthetic and had a shorter time in the block room.25 Combined ultrasound and nerve stimulation guided techniques are now being used more frequently with high success rates. Finally, National Institute for Health and Clinical Excellence (NICE) guidelines (January 2009) also supported the increased efficacy and safety profile of ultrasound-guided nerve blocks.26
1 Van den Bosch JE, Bonsel GJ, Moons KG, et al. Effect of postoperative experiences on willingness to pay to avoid postoperative pain, nausea, and vomiting. Anaesthesiology. 2006;104:1033-1039.
2 Bruster S, Jarman B, Bosanquet N, et al. National survey of hospital patients. BMJ. 1994;309:1542-1546.
3 Apfelbaum JL, Chen C, Mehta S, et al. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be under-managed. Anesth Analg. 2003;97:534-540.
4 Werner MU, Soholm L, Rotboll-Nielsen P, et al. Does an acute pain service improve postoperative outcome? Anesth Analg. 2002;95:1361-1372.
5 White PF. The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesth Analg. 2005;101:S5-22.
6 Power I. Recent advances in postoperative pain therapy. Br J anaesth. 2005;95:43-51.
7 Hyllested M, Jones S, Pedersen JL, et al. Comparative effect of paracetamol, NSAIDS or their combination in postoperative pain management: a qualitative review. Br J Anaesth. 2002;88:199-214.
8 Gregoire N, Hovsepian L, Gualano V, et al. Safety and pharmacokinetics of paracetamol following intravenous administration of 5 g during the first 24 h with a 2 g starting dose. Clin Pharmacol Ther. 2007;81:401-405.
9 Marret E, Kurdi O, Zufferey P, et al. Effects of nonsteroidal anti-inflammatory drugs on patient-controlled analgesia morphine side effects: meta-analysis of randomised controlled trials. Anesthesiology. 2005;102:1249-1260.
10 Marret E, Flahaut A, Samama C-M, et al. Effects of postoperative nonsteroidal anti-inflammatory drugs on bleeding risk after tonsillectomy. Anaesthesiology. 2003;98:1497-1502.
11 Dsida R, Cote C. Nonsteroidal anti-inflammatory drugs and hemorrhage following tonsillectomy: do we have the data? Anaesthesiology. 2004;100:749-751.
12 Nussmier NA, Whelton AA, Brown MT, et al. Complications of the COX-2 inhibitors parecoxib and valdecoxib after cardiac surgery. N Engl J Med. 2005;352:1081-1091.
13 Kearney PM, Baigent C, Godwin J, et al. Do selective cyclo-oxygenase-2 inhibitors and traditional non-steroidal anti-inflammatory drugs increase the risk of atherothrombosis? Meta-analysis of randomised trials. BMJ. 2006;332:1302-1303.
14 Comfort VK, Code WE, Rooney ME, et al. Naproxen premedication reduces postoperative tubal ligation pain. Can J Anaesth. 1992;39:349-352.
15 O’Hanlon JJ, Muldoon T, Lowry D, et al. Improved postoperative analgesia with preoperative piroxicam. Can J Anaesth. 1996;43:102-105.
16 Apfel CC, Roewer N, Kortila K. How to study postoperative nausea and vomiting. Acta Anaesth Scand. 2002;46:921-928.
17 Ahmed AB, Hobbs GJ, Curran JP. Randomized, placebo-controlled trial of combination antiemetic prophylaxis for day-case gynaecological laparoscopic surgery. Br J Anaesth. 2000;85:678-682.
18 Cochrane for Clinicians. Patient-controlled analgesia for postoperative pain. Am Fam Physician. 2007;76(11):1645.
19 de Beer JdeV, Winemaker MJ, Donnely GA, et al. Efficacy and safety of controlled-release oxycodone and standard therapies for postoperative pain after knee or hip replacement. Can J Surg. 2005;48:277-283.
20 Beaulieu P. Non-opioid strategies for acute pain management. Can J Anesth. 2007;54:481-485.
21 Beaudet V, Williams SR, Tetreault P, et al. Perioperative interscalene block versus intra-articular injection of local anesthetics for postoperative analgesia in shoulder surgery. Reg Anaesth Pain Med. 2008;33(2):134-139.
22 Borgeat A, Schapp B, Biasca N, et al. Patient controlled analgesia after major shoulder surgery: patient controlled interscalene analgesia versus patient controlled analgesia. Anaesthesiology. 1997;87:1343-1347.
23 Rawal N, Axelsson K, Hylander J, et al. Postoperative patient-controlled local anesthetic administration at home. Anesth Analg. 1998;86:86-89.
24 Marhofer P, Greher M, Kapral S. Ultrasound guidance in regional anaesthesia. Br J Anaesth. 2005;94:7-17.
25 Lo N, Brull R, Perlas A, et al. Evolution of ultrasound guided axillary brachial plexus blockade: retrospective analysis of 662 blocks. Can J Anesth. 2008;55:408-413.
26 Ultrasound-guided regional nerve block. Interventional procedure guidance 285. National Institute for Health and Clinical Excellence, Ref No. N1779; January 2009.