Problem 2 Postoperative fever
As part of her initial management the patient will require some investigations and treatment.
While the various investigations are arranged, treatment must be started.
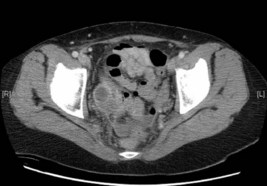
A CT scan of the abdomen is performed. One slice is shown.
Answers
As the patient is septic she may be coagulopathic and her clotting profile should be established.
Revision Points
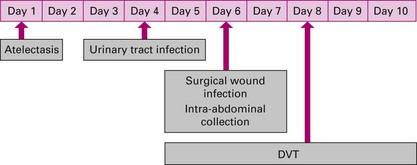
The time of onset of fever in relation to the surgery can be a useful guide in assessment and determining the underlying cause (Figure 2.2).
When assessing a patient with a postoperative fever it is important to consider the surgery that has been performed, as the risk of complications is directly related to the nature of the surgical procedure and this may guide the investigations. The risk of infection depends on the bacterial load related to the operation (Box 2.1). Similarly, other causes of postoperative fever are more common following certain operations, for example venous thrombo-embolic events are high risks following orthopaedic operations.
Box 2.1
Classification of risk of postoperative infection
Antibiotics should be used on a prophylactic basis for those at increased risk of infection through the type of procedure to be performed (contaminated and dirty procedures – see Box 2.1). Two other groups of patients likely to require prophylactic antibiotics, no matter what the type of procedure, are (i) those who might be immunocompromised (diabetes, steroids, cytotoxic therapy) and (ii) those who have prostheses (e.g. heart valves) in whom any infection could have disastrous consequences. Other patients at increased risk of infection include the obese, those who are malnourished, the anaemic and those who suffer with alcoholism.