CHAPTER 101 Postoperative Deformity of the Cervical Spine
Preventing Iatrogenic Cervical Malalignment During Anterior Surgery
Positioning
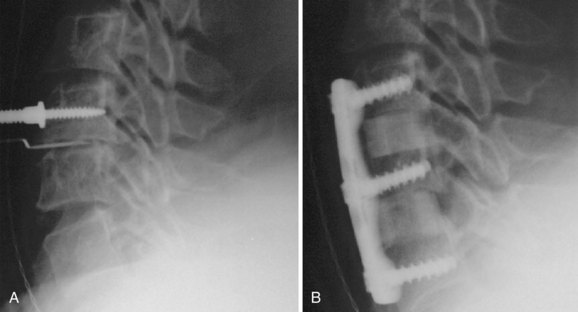
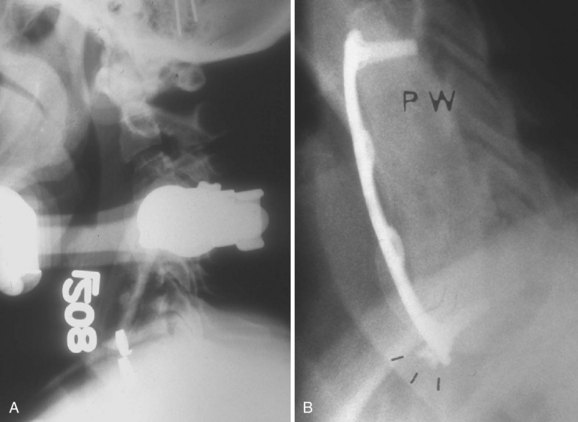
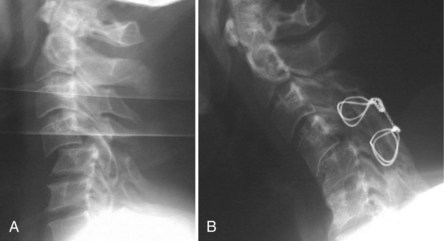
The most common error of patient positioning for anterior surgery is to put the patient’s neck into hyperlordosis. A rolled towel is often placed underneath the patient across the shoulders to extend the neck. Whereas moderate cervical lordosis is desirable, hyperlordosis such that the spinous processes are touching is, in general, excessive. If the patient is fused in this position he or she will often have severe interscapular and posterior cervical pain, especially if an extensive foraminotomy is not performed at the time of the procedure. Extension of the neck narrows the posterior neural foramen and may result in root compression. To avoid this complication, we routinely inspect the position with the patient supine to ensure that the neck is in a relatively neutral or slightly lordotic position. In addition, we examine the localizing radiograph to verify that the neck is in an acceptable amount of lordosis. If the patient’s neck is hyperlordotic on this radiograph, we place Caspar distractor pins with the tips converging. When the distractor is placed over the pins, the amount of lordosis will be reduced (Fig. 101–1). At the end of the procedure, the goal is to have the neck in a normal lordotic configuration.
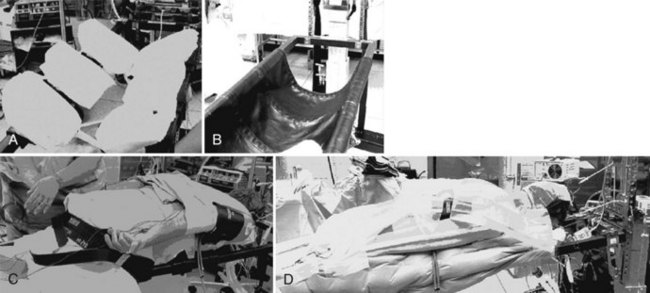
The surgeon can avoid creating a rotational deformity by using one of two techniques. The first is to ask the anesthesiologist to confirm that the nose is pointed straight up before placing any grafts and putting on the instrumentation. This, however, requires that the surgeon remember to ask the anesthesiologist. We prefer to use a more foolproof technique of routinely placing a tape across the forehead to prevent inadvertent rotation of the head during the operation (Fig. 101–2). Another variation on this technique is to use commercially available head holders with an elastic chinstrap to stabilize the head. When one is performing high cervical approaches to C2-3 or C3-4, it is sometimes advantageous to rotate the neck to the contralateral side so as to gain better access to the spine. Under those circumstances, it is a good idea to write a reminder on the sterile drape to turn the head back into neutral alignment before grafting and plating are done.
Decompression
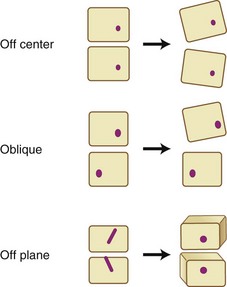
We routinely use Caspar distractor pins to open the disc space during anterior cervical surgery. Although the distractor is quite useful in exposing the disc space, one must be careful in placing the pins. If both pins are placed off center to one side, the disc space will open asymmetrically, causing segmental coronal angulation. If the pins are placed in an oblique position, the disc space will open asymmetrically and relative lateral translation of the vertebral bodies will occur. Finally, if the pins are placed in different planes, a rotational malalignment of the vertebra can occur (Fig. 101–3).
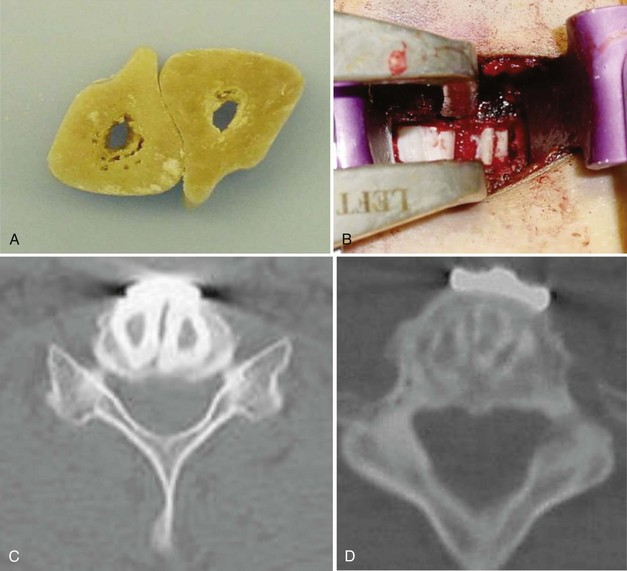
Failure to expose the entire disc space may increase the likelihood of performing an asymmetrical discectomy or corpectomy. Placing a graft asymmetrically on one side may result in a coronal plane deformity (Fig. 101–4). One can avoid this by exposing the intervertebral disc to the uncovertebral joints bilaterally before starting the decompression. These lateral structures provide a fixed reference to the surgeon and assist in performing a symmetrical decompression and reconstruction.
The type of decompression one performs also matters. Long corpectomies reconstructed with an allograft long bone can only be placed into a neutral or kyphotic position; because the graft is straight, it is impossible to produce lordosis. Kyphosis typically develops as the graft subsides into the endplates. To avoid this, we routinely use segmental decompression combining corpectomies at the levels that have retrovertebral compression with discectomies at levels that only have retrodiscal neural compromise (Fig. 101–5). For patients who have retrovertebral compression at more than one level, we perform a procedure that we call corpectomy-corpectomy: performing corpectomy at one level and skipping the next level, followed by a corpectomy at the third level (Fig. 101–6). This type of segmental decompression and fixation using several small grafts rather than one long strut graft allows for better preservation of cervical lordosis.
Noninstrumented Fusion
A multilevel noninstrumented arthrodesis of the cervical spine can result in kyphosis as the grafts collapse or resorb (Fig. 101–7). Whereas the use of a plate does not absolutely guarantee the avoidance of kyphosis, most surgeons would agree that anterior cervical plates decrease the likelihood of postoperative kyphosis.1,2
Graft Selection
The type of graft material that one uses can also influence the likelihood of postoperative kyphosis. In general, fresh frozen allografts are less likely to collapse than freeze-dried bone, and freeze-dried bone is less likely to collapse than irradiated, freeze-dried bone.3 If a surgeon finds a piece of allograft to be fragile, it is advisable to use another specimen rather than implanting an inferior allograft. We most commonly use cortical allografts harvested from the fibula, ulna, radius, humerus, and occasionally the tibia. We also use dense cancellous allograft from the patella (Fig. 101–8).
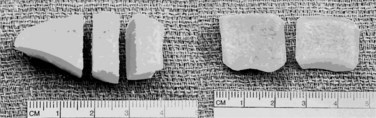
The size of the graft also influences the propensity to develop postoperative kyphosis (Fig. 101–9). The grafts should be large enough to allow for 1 or 2 mm of subsidence without creating kyphosis. In addition, the more graft one uses per level, the less likely it is to collapse. For this reason, we routinely fill the disc space with as much graft as possible, which often means placing two allografts side by side (Fig. 101–10).

FIGURE 101–9 This surgeon placed prefabricated grafts that are clearly undersized, resulting in segmental kyphosis.
Anterior Instrumentation
Although judicious and careful use of anterior cervical plates can help avoid postoperative kyphosis, poor attention to detail can result in plate-induced malalignment. If a screw inadvertently perforates an adjacent disc space, it can result in rapid degeneration and collapse of that disc space. Even if the screw does not perforate the next disc space, placement of a plate within 5 mm of an adjacent level increases the likelihood of adjacent-level ossification development (Fig. 101–11).4 The adjacent-level ossification can become quite profound, causing rapid deterioration of that adjacent disc space, and result in kyphosis. The surgeon must be careful not to use a plate that is too long, especially when using dynamic or subsidence plates because these will migrate toward the adjacent disc spaces as the grafts subside.

FIGURE 101–11 If a plate is too close to the neighboring disc space, adjacent-level ossification disease may occur.
Patients who have long corpectomies are prone to graft extrusion. The reported incidence is as high as 9%.5 Unfortunately, plates do not help prevent such complications (Fig. 101–12).6 With static plates, extension of the neck loads the graft as the plate acts as an anterior tension band. In flexion the graft is unloaded because the anterior cervical plate acts as the center of rotation. In extension the inferior screws can pull out, and in flexion they can be driven into the next disc space, resulting in graft collapse or extrusion. To avoid these complications, we routinely perform circumferential stabilization in patients who undergo corpectomies at two or more levels. We also prefer a circumferential approach in patients with poor quality bone who undergo single-level corpectomies.
Preventing Iatrogenic Cervical Malalignment During Posterior Surgery
Positioning
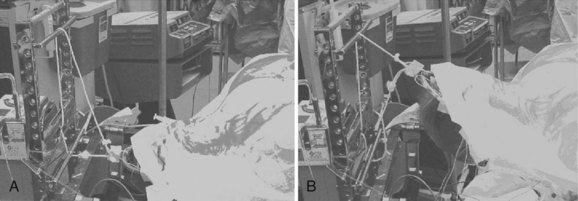
Positioning for posterior cervical procedures is just as critical as for anterior operations. We routinely use the Jackson frame (OSI-Orthopedic Systems, Inc., Union City, Calif.) to position our patients for posterior operations (Fig. 101–13). We tape the shoulders down just as for the anterior procedures. We also make sure that one shoulder is not pulled asymmetrically in order to prevent an iatrogenic coronal plane deformity. We place bolsters just underneath the clavicle and use Gardner-Wells tongs with bivector traction to allow us to position the neck in either flexion or extension (Fig. 101–14). We check the position preoperatively to ensure that we can place the neck into an adequate amount of flexion and extension. Foraminotomies are best accomplished with the neck in maximal flexion, which unshingles the facets and exposes the underlying superior articular facet. If the neck is not adequately flexed during a foraminotomy, one must resect a large amount of the overhanging inferior articular facet to expose the underlying superior facet. This may weaken the structure and lead to a fracture. More commonly, it makes it difficult to place a lateral mass screw in patients who require a fusion and decompression. Before fusion, we change the weight from the lower, or flexion, rope to the upper, or extension, rope. The advantage of using bivector tong traction is that the surgeon can easily alter the position of the neck intraoperatively. With fixed head holders such as Mayfield tongs, an assistant has to crawl under the table to reposition the head holder.
Although it is important to position the neck properly for fixation of the subaxial spine, it becomes even more critical when one is performing an occipitocervical or an occiput-to-thoracic fusion. If the neck is improperly positioned and instrumented, the resulting malalignment can be quite debilitating. Phillips and colleagues7 measured the occipitocervical angle on 30 normal cervical spine radiographs of patients in flexion, extension, and neutral alignment. The occipitocervical angle was defined as the angle between the McRae line (the line connecting the basion and opisthion, which demarcates the foramen magnum on a lateral radiograph) and a line parallel to the rostral endplate of C3. The mean occipitocervical angle on the neutral radiographs was 44 degrees. Phillips and colleagues7 recommend that when performing an occipitocervical fixation and fusion, the surgeon should try to fix the occiput and upper cervical spine in as close to this value as possible to provide the patient with a functional head position (Fig. 101–15). We concur with this for patients with occipitocervical fusions. However, when performing occiput-to-thoracic fusions, we prefer to fix the patient with 5 to 10 degrees of flexion compared with normal. This is because these patients are unable to bend their necks at all, and if they undergo fusion looking straight ahead they cannot look down to see their own bodies.
Decompression
Deformities can result from overly aggressive decompressions of the cervical spine. Even minimally invasive procedures such as posterior cervical foraminotomies can result in a postoperative deformity. If the procedure is performed through a small tubular retractor by a surgeon who is not intimately familiar with the microanatomy of the facet joint or who loses anatomic landmarks, too much of the facet may be resected. Zdeblick demonstrated that resection of more than 50% of a facet can result in instability (Fig. 101–16).8 To prevent this, one must always identify and visualize the lateral and medial aspects of the facet joint and take care to resect only the medial half of the joint.

FIGURE 101–16 Resection of more than 50% of the facet, particularly in the setting of a complete laminectomy, may lead to kyphosis.
A more common deformity-causing decompression is a laminectomy without a fusion. Laminectomies in children have been associated with a high incidence of postlaminectomy kyphosis (Fig. 101–17).9 Even in adults it is difficult to predict when a patient might develop postoperative kyphosis. We therefore reserve complete laminectomies for patients who have significant anterior-stabilizing osteophytes with minimal range of motion of the cervical spine.
Noninstrumented Fusion
We believe that noninstrumented fusions of the posterior cervical spine are rarely, if ever, indicated. With safe and effective modern instrumentation including lateral mass screws, spinous process wires/cables, and polyaxial screw-rod instrumentation, it is rare for us to find a situation in which we would consider a noninstrumented arthrodesis. A patient who undergoes a noninstrumented arthrodesis will often have pain posteriorly, resulting in the loss of normal lordosis. As the spine fuses, it generally does so in a kyphotic or, at best, straight alignment (Fig. 101–18).
Inadequate Instrumentation
The use of inadequate instrumentation can result in postoperative malalignment. For example, in trauma cases where patients have significant osteoligamentous disruption resulting in an unstable spine, one must achieve solid fixation with instrumentation to stabilize that segment. If the spinous processes and/or the lateral masses have been disrupted such that one cannot attain adequate bony purchase, then the fixation may have to be extended cranially and caudally until good purchase is obtained. Alternatively, circumferential stabilization can be performed. If the fixation is still inadequate, consideration should be given to immobilizing the patient in a halo vest. To the extent possible, all fixation points should be used. The greater the instability, the greater is the necessity to obtain adequate bony purchase at multiple levels (Figs. 101-19 and 101-20).
Surgical Treatment of Iatrogenic Deformity
Prior Laminectomies
A special situation arises when a patient who has previously undergone a laminectomy has persistent anterior compression and requires an anterior corpectomy with reconstruction. In these cases, we generally recommend a circumferential operation with anterior corpectomy followed by posterior stabilization with lateral mass instrumentation. Even with halo vest immobilization postoperatively, these patients are at a high risk for graft extrusion, collapse, and recurrent kyphosis.10 Patients who have undergone a laminectomy and subsequently undergo an anterior corpectomy have two halves of the spine that are connected only by soft tissues (Fig. 101–21). These patients are extremely unstable to both rotation and flexion-extension forces. We strongly believe that in the majority of cases these patients are best treated with instrumentation circumferentially, as well as adequate postoperative immobilization.
In patients who have excellent bone quality and who only require a single-level corpectomy, one can occasionally perform a single-level corpectomy at the level of retrovertebral compression and discectomies at the levels with only retrodiscal compression. If one can get four screw points above the level of the corpectomy and four to six points below, and if a rigid collar is used postoperatively, it may be possible to treat the patient with an anterior-only operation (Fig. 101–22). But for the majority of patients who have significant kyphosis and persistent stenosis requiring a cervical corpectomy, circumferential instrumentation is indicated. Because these patients have unstable cervical spines, the use of lateral mass instrumentation alone may result in failure, especially in patients with osteoporosis (Fig. 101–23).
Prior Posterior Fusion
Case Study 1
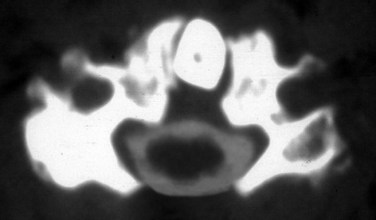
This case (Fig. 101–24) illustrates what can be done if a patient has only a solid posterior fusion mass with no fusion anteriorly. This patient had undergone a posterior cervical fusion at an outside institution using wires. She presented to us several years later, with severe neck pain, kyphosis, and persistent myeloradiculopathy. She was found to have disc protrusions at C5-6 and C6-7. She had retrovertebral compression behind C4 and retrodiscal compression at C5-6 and C6-7. We approached her posteriorly first and performed an osteotomy through the facet at C3-4. We were then able to correct most of her kyphosis posteriorly, using segmental instrumentation. We then turned her anteriorly and performed combinations of corpectomies and discectomies to restore her overall alignment and to decompress her C5-6 and C6-7 levels. She did quite well postoperatively with complete resolution of her myeloradiculopathy and her axial neck pain.
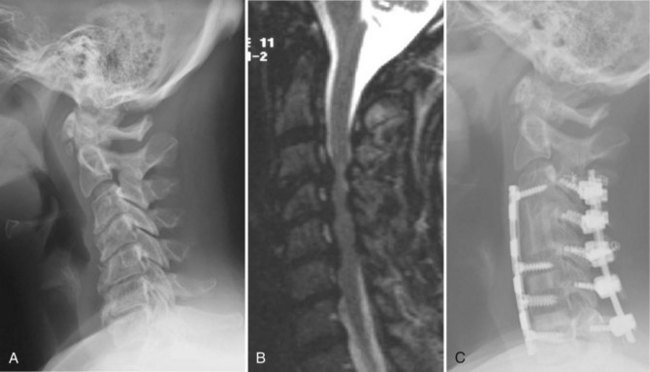
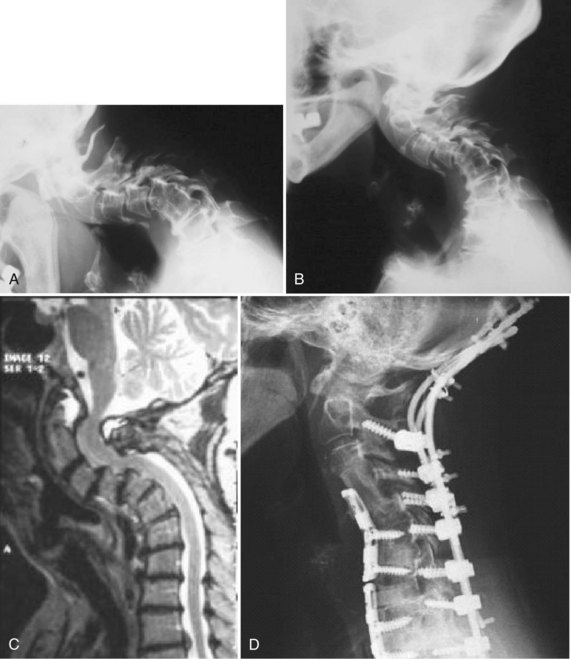
Case Study 2
This case (Fig. 101–25) illustrates the use of the fusion mass to achieve a solid fusion and obtain bony fixation points. This child was status post C1 and C2 laminectomy and occipitocervical fusion for congenital cervical anomalies. Unfortunately, the occipital fixation pulled out but the child went on to a solid fusion with the neck in kyphosis (see Fig. 101–25A). As the child continued to grow, C2 began to grow into the foramen magnum, causing compression of the pons. We performed an osteotomy of the fusion mass (see Fig. 101–25B). The bone between the foramen magnum and the fusion mass was resected, revealing the underlying thecal sac. Then the fusion mass was cut on the lateral margins down to about C3. At the caudal margin, a trough was created so that it could act as a hinge, from which the fusion mass could be lifted dorsally to decompress the proximal spinal cord. We then extended the neck and dorsally lifted up the fusion mass (see Fig. 101–25C). The dorsal aspect of the skull at the level of the foramen magnum is now in contact with the fusion mass. A small window is left centrally so that we can directly visualize the proximal cord to confirm that there is no compression. Occipitocervical instrumentation is then placed both laterally into the fusion masses and centrally into the fusion masses and the remaining spinous processes (see Fig. 101–25D). Normally such a small child would have poor fixation points. However, using any and all bony fixation points can allow for solid rigid fixation. The patient had a functional head position after surgery, and a solid fusion was obtained (see Fig. 101–25E and F).
Case Study 3
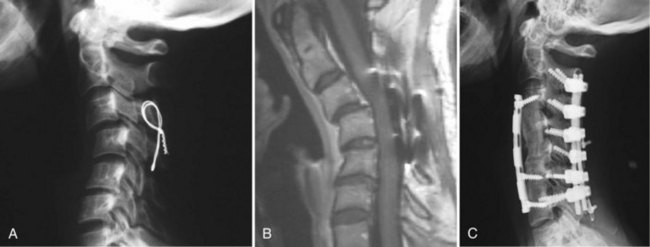
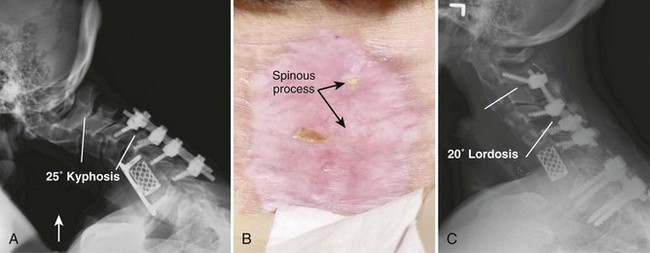
This case (Fig. 101–26) illustrates what can be done with a multiply operated patient with a problem with soft tissue coverage. In this case the patient had a C6 corpectomy and a posterior fusion from C4-7 at another institution (see Fig. 101–26A). This was complicated by a postoperative infection, which necessitated that the wound be kept open and allowed to granulate in. At the time of her presentation to us, the spinous processes were still exposed (see Fig. 102-26B) and she was complaining of intolerable neck pain. We treated her initially by placing her into a halo vest to extend the neck to decrease the tension on her wound. This allowed the wound to finish granulating in so that the spinous processes were covered. We operated on her once the erythrocyte sedimentation rate had normalized and we were sure that there was no further evidence of any infection. She was fused from C4-7 and autofused from C7-T1. We approached her posteriorly first and took down the old fusion mass at C4-5 and then reinstrumented her from C2-6. We also fused and instrumented T1-2 but did not attach the cervical and thoracic constructs because she had a solid fusion over this intervening area and because this was the area where she had the least amount of soft tissue coverage. We believed that dominoes at this level would have been too bulky in an area where she had little to no soft tissue coverage. We then turned her anteriorly and performed discectomies and fusions at C2-3, C3-4, and C4-5. Because of the titanium cage that was placed anteriorly, we elected not to perform an osteotomy through the old fusion mass. Although we certainly could have achieved a better correction by taking down the old fusion mass at the C6 corpectomy site, this would have necessitated an anterior osteotomy followed by another posterior operation. We believed that this would have unnecessarily prolonged her case. The posterior operation was performed in 4 hours, and the anterior operation was performed in 1 hour and 45 minutes, allowing us to extubate the patient immediately postoperatively. We were able to correct her from 12 degrees of kyphosis to 4 degrees of lordosis over the C4-5 segment (see Fig. 101–26C).
Prior Circumferential Fusion
A patient with solid arthrodeses anteriorly and posteriorly with a cervical deformity presents a challenge to the surgeon. In these cases, one often has to perform releases anteriorly and posteriorly before being able to correct the deformity. Although some surgeons recommend a “540-degree” procedure (anterior-posterior-anterior) for deformity correction, we have found that some patients can be treated with a two-stage (anterior then posterior) procedure with acceptable results.11 The technique uses the plasticity of the posterior fusion and the capability of modern anterior cervical plates to allow translation and angulation of the screws to achieve deformity correction in two steps.
Case Study 4
This case (Fig. 101–27) illustrates an anterior-posterior procedure to correct a postoperative kyphosis in a patient with a circumferential fusion. This patient presented to us after having had six prior operations in his hometown including an anterior cervical discectomy and fusion from C3-T1 and a posterior fusion from C3-7. Although he had achieved a solid fusion from C3-6, he had a pseudarthrosis at C6-7 and was kyphotic at C4-5 and C5-6. In addition, he had severe facet arthrosis at C2-3. We performed anterior osteotomies at C4-5 and C5-6 and repaired the pseudarthrosis at C6-7. We placed structural grafts at all levels and plated him anteriorly. The anterior operation took 3 hours and 20 minutes. We then turned him posteriorly and performed osteotomies through the posterior fusion mass. We fused and instrumented from C2 to T1. The posterior operation took 3 hours. The patient was left intubated overnight to protect his airway. Following a cuff-leak test, he was extubated.
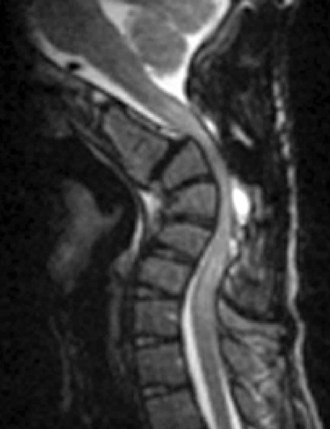
Finally, it should be remembered that not all deformities need to be completely corrected. So long as the deformity is not causing excessive amounts of axial neck pain, myelopathy, or radiculopathy, a partial correction will often suffice. Figure 101–28 demonstrates a patient with rheumatoid arthritis and occipitocervical subluxation. This is best appreciated on the flexion-extension views of the upper cervical spine where the basion is anterior to the tip of the dens inflection and posterior to it in extension. On the sagittal MRI one can see an area of increased signal in the superior posterior aspect of the dens, just below the clivus. This represents the area of subluxation when the neck is in extension as it was for this MRI. Because the patient had multilevel subluxations and an autofusion at C5-6, which was in kyphosis, we elected to expedite the operation by performing decompressions and fusion circumferentially but not correcting the focal kyphosis at C5-6. She also had numerous antibodies, which precluded the blood bank from being able to type and crossmatch her for any transfusions. We, therefore, performed a partial correction to achieve a modest improvement in the sagittal alignment. Because of the persistent kyphosis, it was not possible to contour a single plate, nor did we believe that it was absolutely necessary. Given that she had rheumatoid arthritis on corticosteroid therapy, we believed that circumferential stabilization would enhance the fusion rate. Indeed, the one area where she is not fused on the lateral radiograph is C7-T1, between the two plates. Although we did not get a perfect correction, we were able to achieve an excellent functional outcome without excessive blood loss or operative time.
Case Study 5
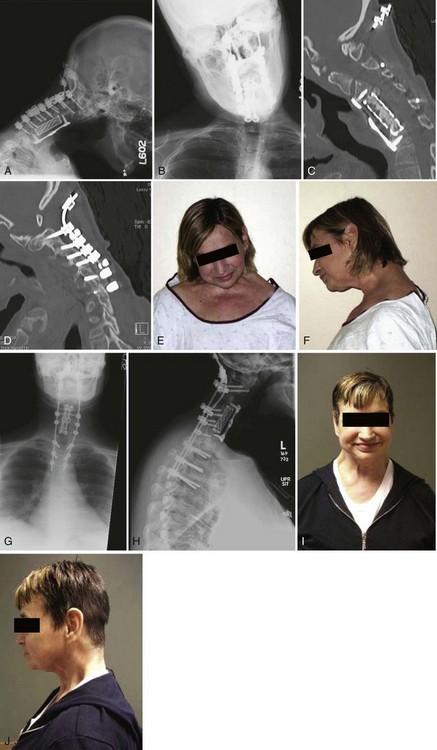
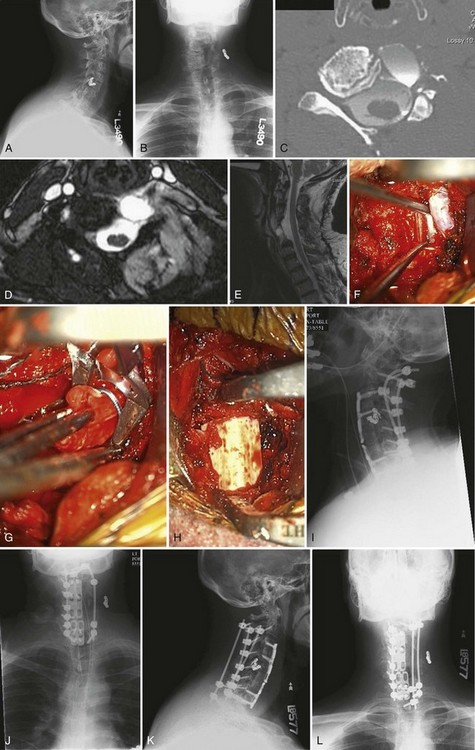
This patient underwent multiple failed anterior and posterior fusion procedures from C3-C7 at another institution. Her latest operation, an occipito-cervical fusion to C7, resulted in pseudarthrosis, skull plate pullout, cervical kyphoscoliosis, and both chin-on-chest and ear-on-shoulder deformities with resultant pain and functional disability (Fig. 101–29A-F). She underwent a posterior-only pedicle subtraction osteotomy and revision posterior spinal fusion from occiput to T4. In order to address both the coronal and sagittal plane deformities, a bigger wedge cut was made on the left side at C3-4 and C7-T1. The pedicles of C4 and T1 were taken down bilaterally and correction achieved through these osteotomies. A large laminectomy was performed at C3, C4, C7, and T1, in addition to foraminotomies at C3-4 and C7-T1. The deformity was then gently corrected by placing the neck in extension and shifting the traction weight to the extension rope from the flexion rope. At this point, permanent occipito-cervical rods were placed. Visual inspection and intraoperative radiographs demonstrated excellent deformity correction in both planes (Fig. 101–29G-J).
Case Study 6
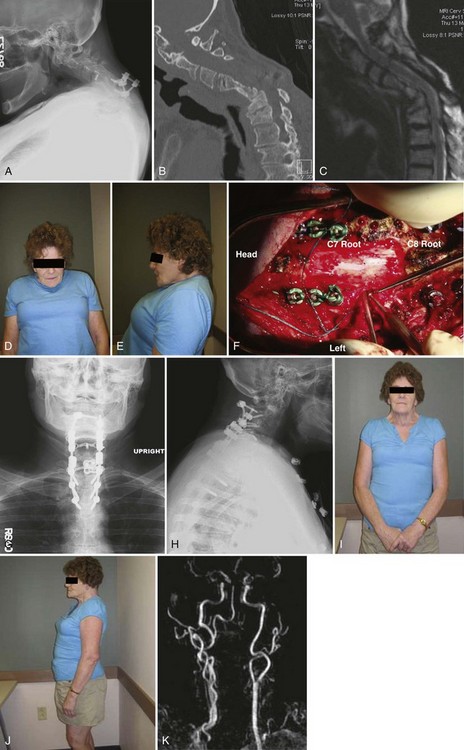
Figures 101–30A-E demonstrate the preoperative images of a patient who had undergone five previous anterior and posterior surgeries including posterior wound infection. She presented to us with postlaminectomy kyphosis and myeloradiculopathy, with obvious sagittal plane deformity adjacent to her previous distal cervical fusion. During the pedicle subtraction osteotomy at C7, after the pedicles of C7 had been completely taken down with C7 and C8 nerve roots free, an inadvertent vertebral artery injury was created and was immediately packed off (Fig. 101–30F). Bleeding was quickly controlled. Despite adequate bilateral decancellation, the neck was unable to be extended. Due to the injured vertebral artery, further left-sided decancellation would have been potentially unsafe. Therefore the decision was made to place temporary rods and close the posterior wound and perform an anterior osteotomy at C7 with C7 corpectomy. The patient was then placed in the prone position again for final correction and instrumentation, as well as arthrodesis. She achieved excellent correction and experienced no untoward sequelae from the vertebral artery injury (Fig. 101–30G-K).
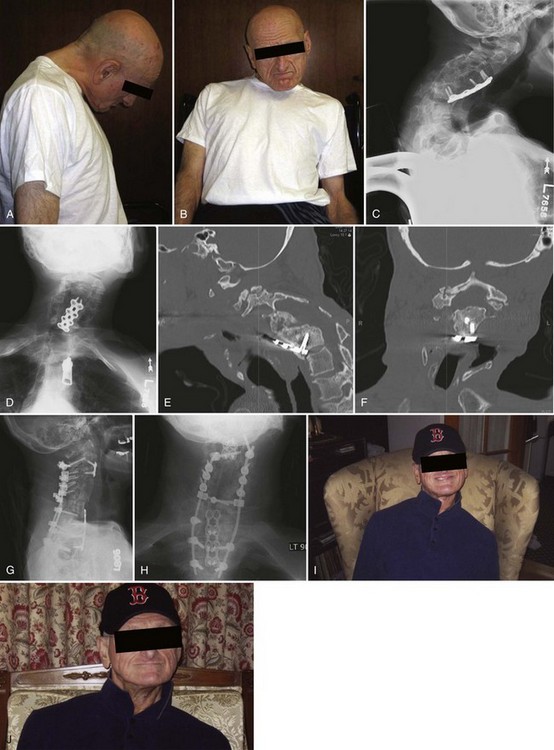
Case Study 7
Figures 101–31A-E reveal the images of a patient who in the distant past had been involved in a helicopter crash and sustained an unspecified cervical spine injury that was treated nonoperatively. He was then found to have developed a pseudomeningocele anteriorly but then subsequently failed attempt at anterior surgical correction at another institution (the patient developed excessive bleeding and an arteriovenous [AV] fistula and the procedure was aborted), and the pseudomeningocele continued to enlarge. He then underwent laminectomies on the left side from C3-C7. On presentation to us, he had severe radicular symptoms, worsening pain, an enlarging pseudomeningocele, and rotational and coronal plane deformities. The patient underwent a corpectomy at C6, ACDF at C3-4 and C7-T1, and repair of pseudomeningocele (Fig. 101–31F-H). Following the anterior procedure, the patient was placed in the prone position for posterior cervical fusion from C2-T1. Copious amounts of bleeding were encountered, despite the fact that the AV fistula had been embolized preoperatively. C2 laminar screws were used bilaterally, followed by placement of lateral mass screws from C3 bilaterally and from C4-C7 on the right side and pedicle screws at T1. The lateral masses on the left could not accept screws due to the bone deficiency from his surgeries in the past (Fig 101–31I-J). The patient did fine and motor examination was normal until postoperative day 3 when the patient developed significant weakness of his left deltoid, biceps, and triceps, presumably from stretch injury related to correction of the coronal plane deformity. He was taken back to the operating room. Upon inspection of his construct, it was clear that the C2 screws had loosened and the left C3 screw had completely pulled out. The rods were removed and were contoured into a less corrected (i.e., more scoliotic) position to reduce the stretch on the nerve roots. A third supplemental rod was placed to secure the tenuous posterior fixation using spinous process screws at C2, C7, and T1. We achieved further fixation of C2 using a short pedicle screw on one side and a pars screw on the other side (Fig. 101–31K-L). Allowing the cervical spine to relax back into a more scoliotic position enabled return of deltoid function on the basis of the intraoperative spinal cord monitoring data, so no further correction was attempted. The patient experienced dramatic improvement in his pain, made a complete neurologic and functional recovery, and was satisfied with his neck position.
Case Study 8
This patient with cerebral palsy had undergone numerous spinal operations before presenting to us including multiple posterior and anterior procedures that were complicated by infections, wound dehiscence, instrumentation removal, myelopathy, and myelomalacia. He presented to us with significant ear-on-shoulder and chin-on-chest deformities in a wheelchair, with inability to achieve a horizontal gaze (Fig. 101–32A-B). He had collapse at C6-7 following anterior C3-6 fusion (Fig. 101–32C-F). We performed an osteotomy through C6 and C7 anteriorly, corpectomy of C7, with ACDF at T1-2, T2-3, and C2-3. Using distraction on the Caspar pins, we were able to correct part of the kyphosis via plastic deformation of the posterior facets and lamina that had been fused. Following placement of the trapezoidal grafts and buttress plates anteriorly to prevent graft extrusion, the patient was placed prone for posterior cervical fusion. C2 received a laminar screw on one side and a pedicle screw on the other. We performed a laminectomy at C6 and a Smith-Peterson osteotomy at C6-C7 following decompression. Next, the neck was corrected into a more neutral sagittal alignment, and the instrumentation was locked in place. An incomplete correction of his scoliosis was intentional in order to not put additional strain on the implants given the patient’s extremely poor bone quality. His gaze, sagittal alignment, and to some extent his coronal alignment, although not perfect, were dramatically improved from baseline (Fig. 101–32G-J). When correcting coronal malalignment, root palsy on the concave side is common, increasing with greater correction. It may be advisable to correct the alignment in stages or accept some degree of undercorrection. Fortunately, in all of our cases, the root palsies have been transient.
Pearls
Key Points
1 Hilibrand AS, Fye MA, Emery SE, et al. Increased rate of arthrodesis with strut grafting after multilevel anterior cervical decompression. Spine. 2002;27:146-151.
2 Kaiser MG, Haid RWJ, Subach BR, et al. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002;50:229-238.
3 Riew KD, Hilibrand AS, Palumbo MA, et al. Anterior cervical corpectomy in patients previously managed with a laminectomy: Short-term complications. J Bone Joint Surg Am. 1999;81:950-957.
4 Zdeblick TA, Abitol JJ, Kunz DN, et al. Cervical stability after sequential capsule resection. Spine. 1993;18:2005-2008.
1 Kaiser MG, Haid RWJ, Subach BR, et al. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002;50:229-238.
2 Wang JC, McDonough PW, Endow KK, et al. Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine. 2000;25:41-45.
3 Vaccaro AR, Chiba K, Heller JG, et al. Bone grafting alternatives in spinal surgery. Spine J. 2002;2:206-215.
4 Park JB, Cho YS, Riew KD. Adjacent level ossification development in patients with anterior cervical plates. J Bone Joint Surg. 2004. Accepted for publication September 2004
5 Hilibrand AS, Fye MA, Emery SE, et al. Increased rate of arthrodesis with strut grafting after multilevel anterior cervical decompression. Spine. 2002;27:146-151.
6 Vaccaro AR, Falatyn SP, Scuderi GJ, et al. Early failure of long segment anterior cervical plate fixation. J Spinal Disord. 1998;11:410-415.
7 Phillips FM, Phillips CS, Wetzel FT, et al. Occipitocervical neutral position: Possible surgical implications. Spine. 1999;24:775-778.
8 Zdeblick TA, Abitol JJ, Kunz DN, et al. Cervical stability after sequential capsule resection. Spine. 1993;18:2005-2008.
9 Bell DF, Walker JL, O’Connor G, et al. Spinal deformity after multiple-level cervical laminectomy in children. Spine. 1994;19:406-411.
10 Riew KD, Hilibrand AS, Palumbo MA, et al. Anterior cervical corpectomy in patients previously managed with a laminectomy: Short-term complications. J Bone Joint Surg Am. 1999;81:950-957.
11 Sin AH, Acharya R, Smith DR, et al. Adopting 540-degree fusion to correct cervical kyphosis. Surg Neurol. 2004;61:515-522.