Postoperative Atelectasis
After reading this chapter, you will be able to:
• List the anatomic alterations of the lungs associated with postoperative atelectasis.
• Describe the causes of postoperative atelectasis.
• List the cardiopulmonary clinical manifestations associated with postoperative atelectasis.
• Describe the general management of postoperative atelectasis.
• Describe the clinical strategies and rationales of the SOAP presented in the case study.
• Define key terms and complete self-assessment questions at the end of the chapter and on Evolve.
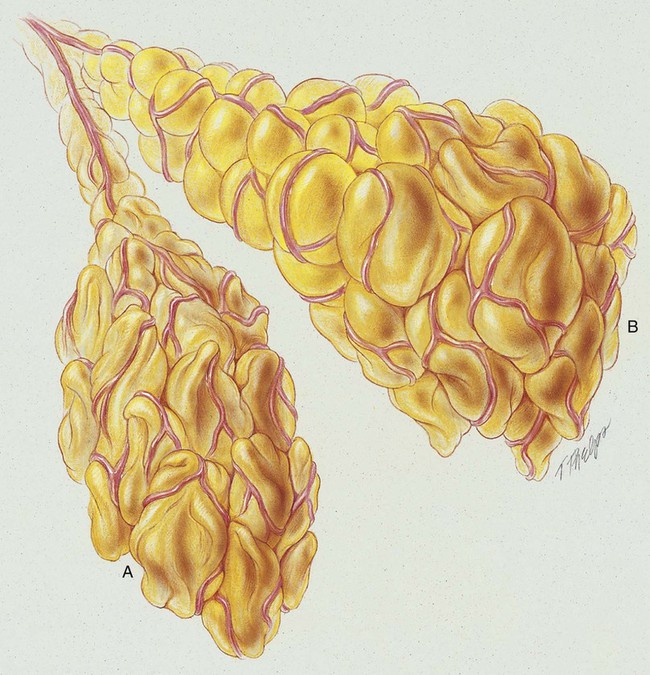
Anatomic Alterations of the Lungs
Atelectasis, in the strict sense of the term, is defined as the condition in which the lungs of the newborn remain unexpanded (airless) at birth. In the clinical setting, however, the meaning of atelectasis in all age groups generally is broadened to include partial or total collapse of previously expanded lung regions. Atelectasis may be limited to the smallest lung unit (i.e., alveolus or primary lobule*; see Figure 42-1), or it may involve an entire lung or a segment or lobe of the lung. In this chapter, postoperative atelectasis is used as a prototype of the atelectasis process.
Postoperative atelectasis commonly is seen after upper abdominal and thoracic surgical procedures.
General Management of Postoperative Atelectasis
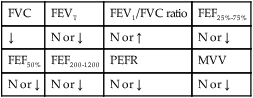
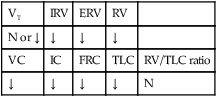
Precipitating factors for postoperative atelectasis should be identified during the preoperative and postoperative assessments (see the previous section on etiology). High-risk patients should be monitored closely. For example, bedside spirometry (vital capacity and inspiratory capacity) is useful in the early detection of atelectasis. Preventive measures often are prescribed for high-risk patients. For example, incentive spirometry frequently is prescribed to encourage good lung expansion. Chest physical therapy also may be given to the patient with mild to moderate preoperative or postoperative bronchial secretions to offset the development of mucous plugs and atelectasis. Patients who demonstrate combined obstructive and restrictive pulmonary disease preoperatively generally are thought to be at extremely high risk for atelectasis. When the diagnosis of postoperative atelectasis has been made, the following respiratory care procedures may be prescribed.
Respiratory Care Treatment Protocols
Oxygen Therapy Protocol
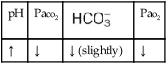
Oxygen therapy is used to treat hypoxemia, decrease the work of breathing, and decrease myocardial work. Because of the hypoxemia that may develop in atelectasis, supplemental oxygen may be required. However, the hypoxemia that develops in postoperative atelectasis is caused by capillary shunting and therefore is often refractory to oxygen therapy (see Oxygen Therapy Protocol, Protocol 9-1).
Mechanical Ventilation Protocol
Short-term mechanical ventilation often is prescribed after major surgery, especially if the patient demonstrates one or more high-risk factors for postoperative atelectasis. For example, in patients undergoing cardiac surgery, mechanical ventilation generally is maintained until the cardiopulmonary parameters are stable (see Mechanical Ventilation Protocols, Protocol 9-5, Protocol 9-6, and Protocol 9-7).
Respiratory Assessment and Plan
S N/A. Patient still sedated from anesthesia.
O RR 34/min, P 130 and regular, BP 100/60. Breath sounds decreased in left lower chest anteriorly. CXR: Left lower lobe atelectasis. On 2 L/min O2 per cannula: pH 7.29, Paco2 63,  25, and Pao2 55.
25, and Pao2 55.
P Contact physician regarding intubation and Mechanical Ventilation Protocol (SIMV mode). Oxygen Therapy Protocol (Fio2 0.5). Bronchopulmonary Hygiene Therapy Protocol (encourage cough and deep breathing, suction frequently, discuss with physician the possibility of respiratory therapist assistance with therapeutic bronchoscopy). Lung Expansion Therapy Protocol after intubation (PEEP based on titration study). Aerosolized Medication Therapy Protocol (in-line albuterol 0.5 mL in 2.0 mL 20% acetylcysteine q2h, then decrease or increase according to reassessment). Repeat ABGs in 30 minutes, and reevaluate. Monitor Spo2 for next 72 hours.
Discussion
Care of a patient with postoperative Atelectasis (see Figure 9-8) is one of the day-to-day responsibilities of the respiratory care practitioner. Accordingly, the respiratory care practitioner must be extremely adept in the assessment and management of such patients. The development of immediate postoperative atelectasis almost always is related to Excessive Bronchial Secretions (see Figure 9-12)—in this case caused by a large mucous plug obstructing the left lower lobe. Because such patients (in the immediate postoperative period) often cannot cough vigorously, particularly after thoracotomy, the decision to initiate therapeutic bronchoscopy immediately rather than to rely on physical therapy and mucolytics was certainly in order.
*A primary lobule is a cluster of alveoli that originates from a single terminal bronchiole. Each primary lobule is about 3.5 mm in diameter and contains about 2000 alveoli. Each lung contains about 150,000 primary lobules. A primary lobule also is called an acinus, terminal respiratory unit, or functional lung unit. The lung parenchyma consists of the terminal respiratory units.



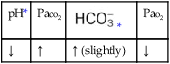
 values will be lower than expected for a particular Pa
values will be lower than expected for a particular Pa



 , Arterial-venous oxygen difference; DO2, total oxygen delivery; O2ER, oxygen extraction ratio;
, Arterial-venous oxygen difference; DO2, total oxygen delivery; O2ER, oxygen extraction ratio;  , pulmonary shunt fraction;
, pulmonary shunt fraction;  , mixed venous oxygen saturation;
, mixed venous oxygen saturation;  , oxygen consumption.
, oxygen consumption.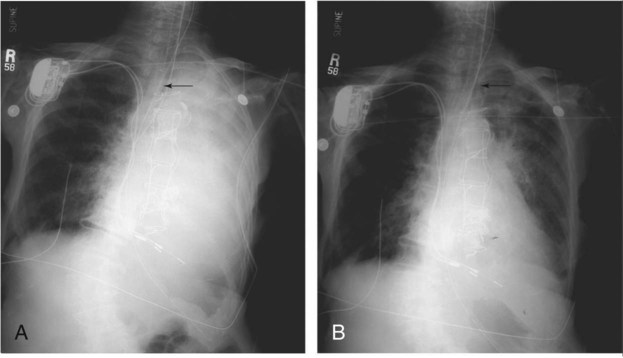
 25, and Pa
25, and Pa