Chapter 3 Posterior Subscapular Approach to the Brachial Plexus
Patient Positioning
• The patient is initially placed in the lateral decubitus position and is then rolled into a prone position, bringing the operative side close to the edge of the operating table.
• Rolls are placed laterally under the anterolateral chest wall and transversely beneath both shoulders and the manubrium of the chest.
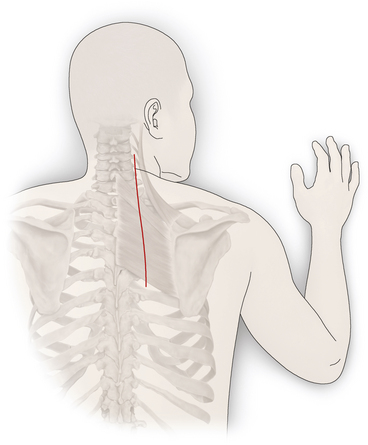
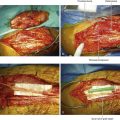
• The shoulder is abducted and the arm is flexed at the elbow. The arm and forearm are then secured to a padded Mayo stand adjacent to the operating table but at a level below it. The stand can be lowered or elevated to change the position of the scapula. The elbow, wrist, and hand are wrapped with protective pads (Figure 3-1).
• The operating table is then tilted up 15 to 20 degrees or into a reverse Trendelenburg position to allow further abduction of the shoulder and the scapula. The operating table can be raised or lowered to change the position of the scapula, as well as that of the head, the neck, and the rest of the shoulder.
• The contralateral arm is padded at the elbow and placed to the side.
• The head is usually turned partially toward the side of the dissection and placed on a well-padded donut or several folded sheets, with care taken to maintain the airway and to keep pressure off the orbits.
• Indications for this approach include tumors or injuries involving the nerve roots or proximal portion of the spinal nerves, especially the lower elements such as C7, C8, and T1.
Skin Incision
• A slightly curvilinear skin incision is made between the thoracic spinous processes and the medial edge of the scapula.
• The incision is curved around the medial edge of the scapula. It is usually placed halfway between the scapular edge and the thoracic spinous processes so that the midsection of the rhomboid muscles can be exposed.
• The incision extends to the posterolateral aspect of the lower neck. This placement tends to protect the spinal branch of the accessory nerve and the ascending branch of the transverse cervical artery, which course close to the medial border of the scapula.
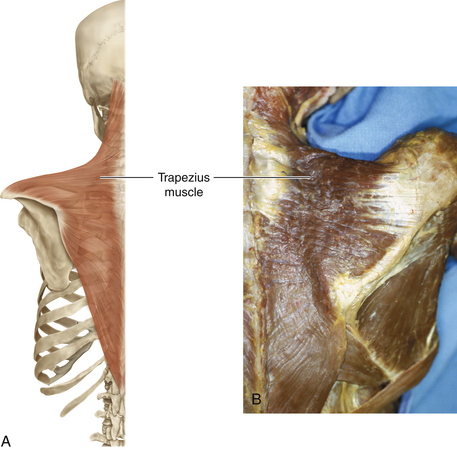
Division of the Trapezius
• The inferior spinal portion of the trapezius muscle is divided along the entire length of the skin incision, halfway between the medial edge of the scapula and the spine. The edges are marked at intervals with suture for later approximation (Figure 3-2).
• A large Kelly clamp is used to dissect beneath the trapezius midway between the scapula and the spine. Segments of muscle are clamped and sectioned between two Kelly or Sarot clamps, beginning inferiorly and proceeding superiorly.
Relevant Anatomy
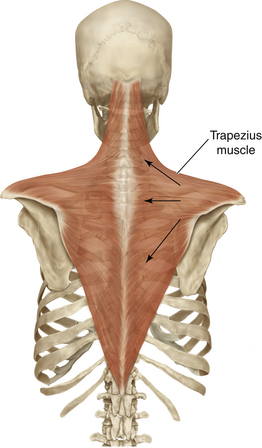
• The trapezius is a diamond-shaped muscle that arises in the midline, from the skull to the lower thorax, and converges on the outer part of the pectoral girdle. It is supplied by the spinal accessory nerve. The upper fibers of the trapezius elevate the scapula, the middle fibers retract, and the lower fibers depress the scapula and lower the shoulder. If the trapezius muscle is reflected laterally, the undersurface, where the spinal accessory nerve innervates, can be exposed (Figure 3-3).
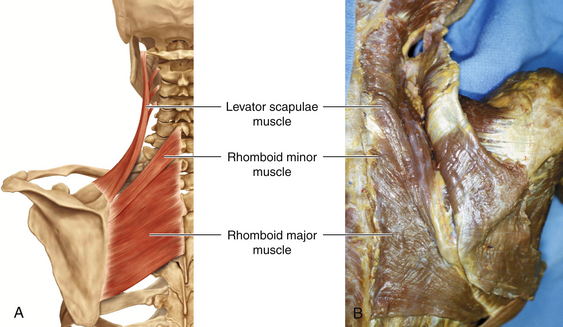
• The superficial muscles of the back can be divided into two groups; the trapezius and latissimus dorsi muscles are the most superficial. Beneath the trapezius, the levator scapulae lies superiorly, the rhomboid minor somewhat medially, and the rhomboid muscle inferiorly. All three of these muscles insert on the medial border of the scapula (Figure 3-4).
• The trapezius muscle distribution is extensive. The diagram has arrows showing the direction of the forces that are brought to bear on the scapula as this large muscle contracts.
• The levator scapulae attaches between the superior angle of the scapula and the lateral extent of the spine. This muscle has to take the strain when the trapezius is paralyzed, and action of this muscle should not be misinterpreted as trapezius function.
• The rhomboids adduct the scapula. A proximal branch of the C5 spinal nerve, the dorsal scapular nerve, supplies both the levators scapulae and the rhomboids. Absence of these functions, in the presence of deltoid paralysis, denotes a very proximal C5 injury. The electromyographer should place the electrode with care, being certain that the recording is being made from the trapezius or rhomboid (deeper); otherwise, confusing information may be obtained.
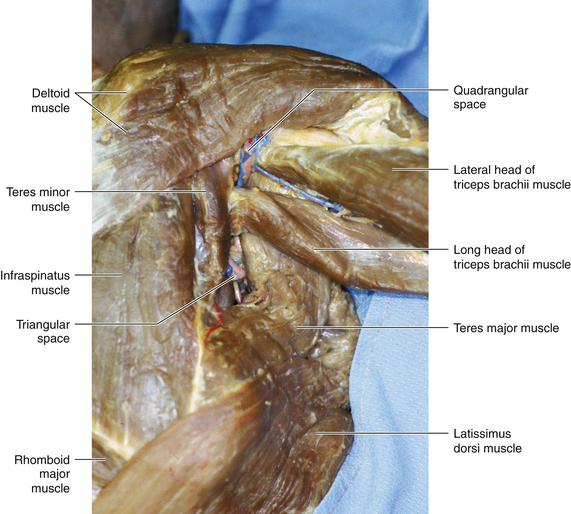
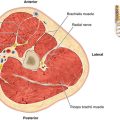
• The triangular space, which transmits the scapular circumflex artery, is formed by the teres major below, the long head of the triceps laterally, and the subscapularis and teres minor above (Figure 3-5).
• The quadrangular space, which contains the axillary nerve and the posterior circumflex humeral artery, is surrounded by the teres major below, the subscapularis and teres minor above, the long head of the triceps medially, and the surgical neck of the humerus laterally (see Figure 3-5).
• The rhomboids minor and major arise from the ligamentum nuchae, spinous processes, and intervening supraspinous ligaments of C7 to T1 and T2 to T5, respectively. The levator scapulae, which arises from the posterior tubercles of the transverse processes of C1 to C4 vertebrae, appears in the floor of the posterior triangle. The dorsal scapular nerve supplies these muscles.
• When the trapezius and rhomboid major muscles are reflected, the deep muscle layer, which includes the semispinalis capitis, splenius capitis, spinalis thoracis, and longissimus thoracis, is exposed.
Division of the Rhomboids
• After division of the trapezius, the rhomboids are sequentially clamped with large Kelly or Sarot clamps and divided.
• The muscle edges are then marked laterally and medially by heavy sutures, which are tied but not cut. This is done so that the rhomboids can be reapproximated relatively accurately during closure.
• If the rhomboid muscles are thick, they are divided in two layers. Each of the muscle edges is marked with heavy suture.
• By dividing muscle away from the edge of the scapula, the deeper dorsal scapular nerve and the ascending branch of the transverse cervical artery are protected. Paired sutures of heavy absorbable material are placed behind each clamp; the needles are left attached, and the ends are “fastened” to adjacent drapes so that subsequent approximation of divided muscle is as accurate as possible.
• As dissection approaches the neck, the thicker portion of the trapezius muscle can be split somewhat, in a medial direction. If necessary, the levator scapulae muscle can be clamped, divided, and marked by sutures as well. Occasionally, some of the serratus posterior muscle is also sectioned.
Exposure of the Posterior Chest Wall
• After division of the rhomboid muscles, the posterior chest wall is exposed.
• A chest retractor is placed with its blades near the upper thoracic spinous processes and under the scapula. As the retractor is opened, the scapula is rotated laterally to expose the posterior aspects of the upper ribs.
• The posterior scalene is detached from the superior surface of the first rib. The more medial segments of the scalenes are removed to begin the exposure of the plexus.
• The surgeon then has a relatively avascular plane beneath the scapula. Using gloved fingers, a plane can be created between the shoulder blade and chest wall.
• One blade of a medium or large self-retaining chest retractor (e.g., Finochietto) is placed beneath the scapula mass.
• A length of the paraspinal muscle mass can be split down to the posterior chest wall to permit firm placement of the other medial blade of the thoracic retractor. The retractor is opened as the limb on the Mayo stand is lowered or the operating table is elevated, so as to provide further abduction and external rotation of the scapula.
Dissection of the Ribs
• The ribs are then palpated. Running the fingers superiorly over the second rib permits palpation of the first rib.
• Sharp dissection of the intercostal muscles on the caudal side of the rib and of the scalene muscles on the cephalad side helps clear the rib of soft tissues.
• Intercostal muscle is cleared from the inferior and posterolateral aspects of the first rib using an Alexander periosteal elevator or Doyen rib dissectors.
• Sometimes a Moynihan forceps passed under the rib can also help clear its muscular attachments.
• The first rib is removed extraperiosteally, from the costotransverse articulation posteriorly to the costoclavicular ligament anteriorly. Either Leksell rongeurs or rib cutters are used to resect the rib up to and including some of its transverse process medially and to the axillary level laterally (Figure 3-6).
• The periosteum is resected along with the rib. Subperiosteal resection of the posterior portion of the second rib is sometimes useful in exposing the first rib in very large patients or for large tumors extending into the mediastinum. Bone edges should be carefully manicured and waxed to minimize injury to the pleura or surrounding tissues.
Exposure of the Brachial Plexus
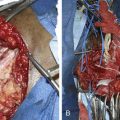
• The posterior and middle scalene muscles are released from their insertions and are resected to their origin from the transverse spinous processes.
• The spinal nerves and the trunks of the brachial plexus are exposed after removal of these muscles superiorly.
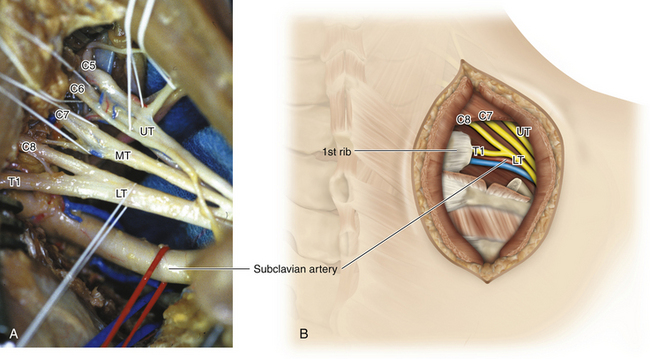
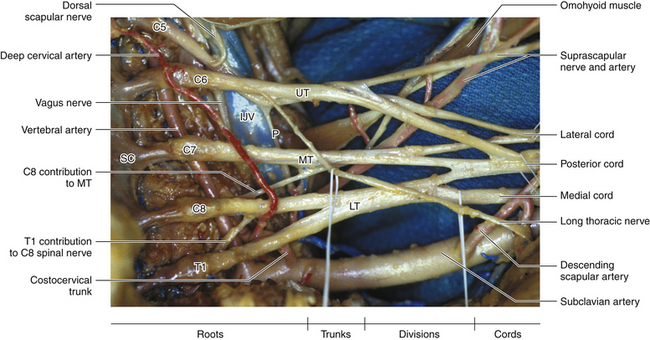
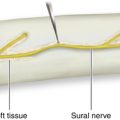
• The brachial plexus is composed of 5 spinal nerves, 3 trunks, 6 divisions, 3 cords, and 15 branches. The spinal nerves of C5 and C6 form the upper trunk. The middle trunk is a continuation of the C7 spinal nerve. The lower trunk is formed by the C8 and T1 spinal nerves. Each trunk separates into anterior and posterior divisions. The anterior divisions of the upper and middle trunks unite to form the lateral cord. The anterior division of the lower trunk forms the medial cord. The posterior divisions of all three trunks form the posterior cord (Figure 3-7).
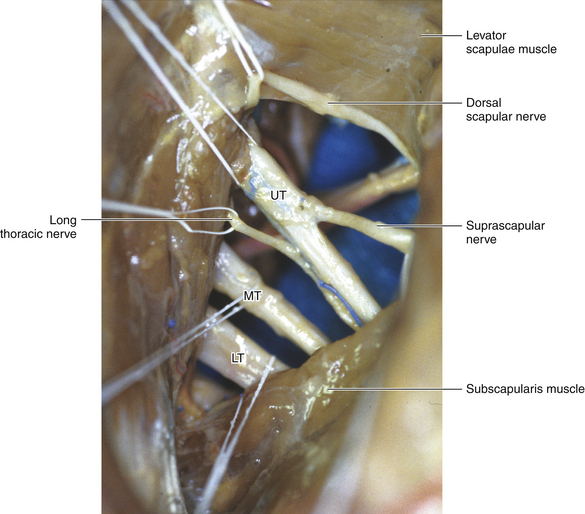
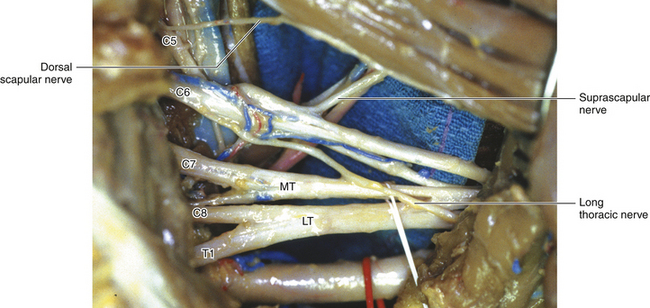
• Following dissection of the superficial layer of back muscles, all three trunks of the brachial plexus can be seen, along with a number of its branches including the long thoracic nerve, dorsal scapular nerve, and suprascapular nerve. These three supraclavicular branches of the brachial plexus arise from the proximal part of the plexus.
• The dorsal scapular nerve arises from the posterior aspect of the ventral ramus of C5, with or without the contribution from C4. The long thoracic nerve arises from the rami of C5, C6, and C7 and, on occasion, C4 and C8. The suprascapular nerve arises from the upper trunk of the brachial plexus (Figure 3-8).
• The long thoracic nerve supplies the serratus anterior muscle. The dorsal scapular nerve supplies the rhomboid muscles. The suprascapular nerve supplies the supraspinatus and infraspinatus muscles (Figure 3-9).
• A Weitlaner retractor can be placed with one set of blades on the second rib and the other on the soft tissues of the superior neck. The retractor is then opened to expose more of the thoracic outlet region.
• Another Weitlaner retractor or a rake can be used to retract the paraspinal muscle medially. Note the origin of the long thoracic nerve from the posterior aspect of the C6 and C7 spinal nerves. The position of the subclavian artery and vein deep to the plexus should also be noted.
• Following the trunks medially and laterally further exposes the spinal nerves and divisions. The extraspinal course of the spinal nerves is dissected back to the spine. Some elevation and retraction of the paraspinous muscle mass exposes the lateral posterior spine overlying the intraforaminal course of the spinal nerves.
Further Dissection into the Supraclavicular Space Posterior to the Plexus
• A Weitlaner retractor can be placed on the second rib and in the superior soft tissues of the neck to open up the supraclavicular space posterior to the plexus.
• A malleable chest retractor can be placed over the apical pleura to protect it while the posterior and medial portion of the first rib is removed between the T1 and CS spinal nerves. The lower trunk is then isolated from the underlying subclavian artery and exposed circumferentially.
• Dissection of the plexus can proceed medially along its spinal nerves of origin and laterally along its posterior and anterior divisions.
• The middle trunk is isolated next and, if necessary, the upper trunk.
• The long thoracic nerve is visible as it originates from the posterior aspect of the C6—or sometimes C5 and C7—spinal nerves, and it can be protected. With this exposure, the phrenic nerve is anterior to both the upper trunk of the brachial plexus and the scalenus anterior muscle, which is usually not divided during this procedure.
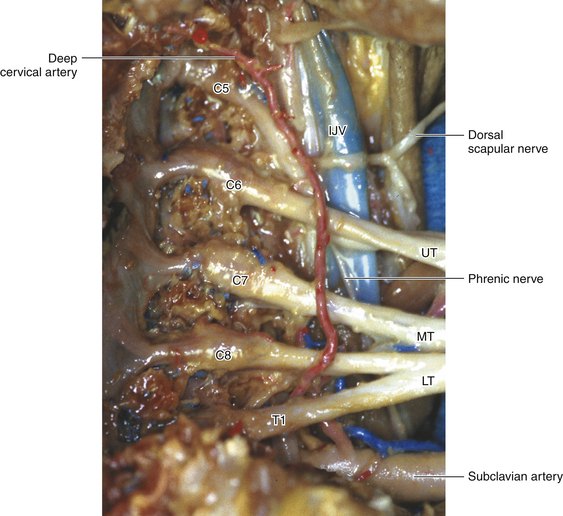
• The phrenic nerve receives a contribution from C5. The vagus nerve can be identified adjacent to the internal jugular vein (Figure 3-10).
• Nerves are dissected free in a circumferential fashion; the use of Penrose drains around the various elements, including the four spinal nerves, to gently retract them helps in the dissection.
• If indicated, intraoperative nerve action potential (NAP) recordings can be obtained.
Lateral Dissection and Identification of Vessels
• Lateral dissection can extend to the divisions, but it is difficult to gain much exposure of the cord level of the plexus with such a posterior approach.
• More laterally, the subclavian artery is anterior and inferior to the lower trunk of the brachial plexus, and the subclavian vein is anterior to both (Figure 3-11).
• Both vessels are identified early in the dissection and usually can be readily dissected away from the lower trunk and protected.
• The costocervical trunk originates from the subclavian artery, behind the scalenus anterior. It divides into the deep cervical artery and the superior intercostal artery.
• The deep cervical artery ascends in the neck, superficial to the brachial plexus, to supply the muscles of the back and neck.
Special Maneuvers: Intraforaminal Exposure of Spinal Nerves
• The extraforaminal spinal nerves of the brachial plexus can be seen lying between the intertransverse muscles in the bony troughs of their respective transverse processes, posterior to the vertebral artery.
• If necessary, the facet joint can be removed using a high-speed drill or with Kerrison and other rongeurs to expose the intraforaminal course of the spinal nerve.
• A posterior foraminotomy is accomplished with the use of a Leksell rongeur. If need be, a semihemilaminectomy can also be done from this approach.
• Angled Kerrison rongeurs are used to open the nerve root foramen. As with an anterior approach, the use of bipolar cautery, with irrigation and Oxycel packing, may help control intraforaminal bleeding. Bleeding from bone is stemmed with bone wax.
• From the posterior approach, the vertebral artery lies on the other (anterior) side of the spinal nerve (see Figure 3-11).
• In most cases, the nerve can be traced to its dural exit by careful bites with a rongeur, keeping the rongeur footplate on top of the nerve but not compressing it. The vertebral artery lies anterior to the nerves, so the nerves can be readily unroofed without fear of serious bleeding.
• Excess scar after a partial foraminectomy can then be dissected away from the spinal nerves using the scalpel or Metzenbaum scissors.
• If more than two facet joints are removed, the area of bone removal is filled in with methyl methacrylate.
Closure
• After the brachial plexus procedure, it is important to achieve meticulous closure of the wound by approximation of the divided but previously marked muscles.
• Anatomical reapproximation of the different muscle planes of the greater and lesser rhomboid muscles, as well as most of the spinal portions of the trapezius and levator scapulae muscles, is therefore necessary.
• Good hemostasis must be obtained. A Penrose drain is sometimes placed with one end deep to the muscle closure and superior to the apical pleura. The other end of the drain is brought out posteriorly through a separate stab wound.
• Any pleural rents should be repaired. The integrity of the pleural repair may be tested by filling the wound with saline and having the anesthetist perform a Valsalva maneuver on the patient. A chest tube is seldom needed.