CHAPTER 12 Posterior Instability of the Shoulder
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. government.
PREOPERATIVE CONSIDERATIONS
The diagnosis and management of posterior instability of the shoulder can be challenging. Posterior instability may be easily overlooked because the initial patient presentation can be confusing; patients present relatively infrequently, and are often referred with a diagnosis other than shoulder instability.1 As always, obtaining an accurate history and diagnosis and accounting for intraoperative pathology are prerequisites for a successful outcome in the treatment of posterior instability of the shoulder.
ANATOMY AND PATHOANATOMY
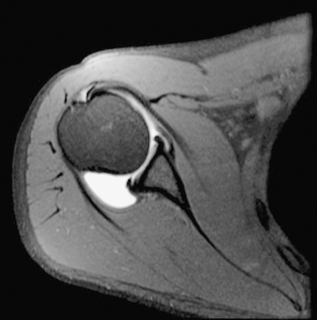
Recent improvements in understanding the anatomy and biomechanics of posterior instability have led to an improvement in clinical diagnosis and recognition of pathology. Posterior shoulder instability can be associated with bony glenoid retroversion, chondrolabral retroversion,2 and decreased posteroinferior capsular size.3 Studies have determined that the quality of the posteroinferior capsule is not as robust as that of the anterior capsule (Fig. 12-1).4
Stabilizers
Dynamic Stabilizers
It should be noted that just as in anterior instability, the rotator cuff muscles are the most important stabilizers in posterior shoulder instability. The subscapularis has been identified as the primary dynamic stabilizer preventing posterior translation,5–7 but all the rotator cuff muscles have been shown to be important in providing concavity-compression of the shoulder joint.6–8 Dynamic inferior stability of the shoulder joint is maintained by the supraspinatus and, some believe, by the long head of the biceps.9 The infraspinatus and teres minor serve as posterior compressors.10 A critical component of the examination of a patient who presents with posterior instability is scapular rhythm and control, paying particular attention to the individual rotator cuff muscles, especially the subscapularis (Fig. 12-2).
Static Stabilizers
The primary static stabilizers of the glenohumeral joint are the bony anatomy and capsulolabral ligamentous complex.5,7,10 The most important posterior ligamentous stabilizer in the provocative posterior loading position of internal rotation and forward flexion is the posterior band of the inferior glenohumeral ligament (IGHL) complex. This positions the posterior band of the IGHL (PIGHL) in an anterior-posterior orientation, enabling resistance to posterior subluxation.6 Stretch of the capsule and PIGHL beyond the initial resting length has been implicated as a cause of posterior and multidirectional instability, and is present even without a labral tear.11
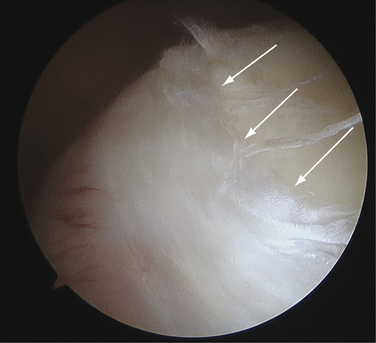
The attachment site of the IGHL is usually well visualized arthroscopically and ranges from 2 to 4 o’clock for the anterior band and 7 to 9 o’clock for the posterior band (Fig. 12-3). In normal shoulder mechanics, the anterosuperior capsule is under tension and there is an obligate simultaneous laxity in the posteroinferior capsule, and vice versa.7 This principle is known as the circle concept of glenohumeral instability. It states that to have shoulder instability, both sides of the capsular mechanism must be disrupted to some extent, although this concept has been questioned by some.12
The labrum influences glenohumeral stability by increasing the concavity-compression mechanism of the humeral head in the glenoid socket.7,8,13 The posterior capsule and PIGHL are much less robust and able to sustain much less tensile force than the anterior capsular structures, which underscores the principle that posterior instability is much different from anterior instability.4 A loss of chondrolabral containment (both an increase in bony retroversion and loss of posteroinferior labral height) has been demonstrated in patients with clinically documented posterior instability.2 The principle of chondrolabral containment is important, given the shallow depth of the bony glenoid, which is augmented by the fibrous ring of the glenoid labrum (Fig. 12-4).
Excessive glenoid or humeral retroversion, glenoid hypoplasia, and loss of chondrolabral containment can all contribute to posterior instability.2,7,8,14,15 However, it has not been shown whether glenoid bony changes, such as retroversion, precede or follow the development of posterior instability. In addition, if the ability to maintain negative intra-articular pressure is compromised (effusion, hematoma, repetitive trauma, and loss of capsular constraint), the humeral head will subluxate and also assume a more inferior position with the arm at the side.16
Pathoanatomy
Three broad causative factors have been defined in posterior instability17–19: traumatic, atraumatic, and cumulative microtrauma.
The most frequent cause of posterior shoulder instability is repetitive microtrauma to the posteroinferior shoulder complex. Sporting activities that involve repetitive loading of the shoulder in front of the body, such as repetitive bench press lifting, overhead weight lifting, rowing, swimming, and blocking linemen in football, are commonly implicated. In these activities, the shoulder is placed in a flexed, adducted, internally rotated position, with a concomitant posterior load resulting in stretch and injury of the posterior band of the IGHL17,18,20,21 and the posterior labrum. The labrum and capsule are repetitively injured, often present in conjunction with a dynamic dysfunction of the shoulder (poor scapulothoracic mechanics).
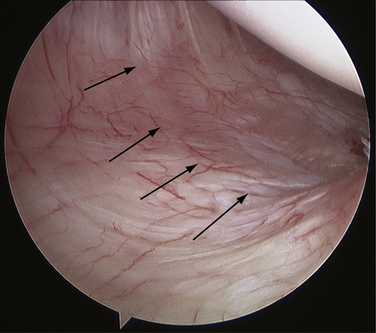
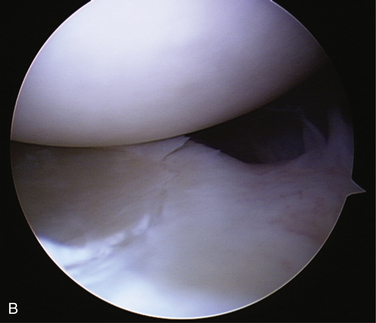
Tears of the labrum, which can develop after acute trauma or repetitive microtrauma, are important to recognize, because those with labral pathology have demonstrated uniformly good results with surgical treatment.20–23 In the cumulative microtrauma model, a Kim lesion may develop. This is thought to occur with cumulative rim loading secondary to persistent shoulder subluxation or microtrauma. This pathologic process leads to a loss of chondrolabral containment, with subsequent development of posterior labral marginal cracks and undermining of the labrum or partial avulsions of the glenoid labrum (Fig. 12-5).24
HISTORY AND PHYSICAL EXAMINATION
The most frequent complaint in patients with posterior shoulder instability is shoulder pain that is often accompanied by decreased athletic performance and loss of strength.17,20,23,25 Pain is often described as generalized throughout the shoulder or at the deep posterior aspect of the shoulder. Subjective apprehension in posterior instability is uncommon.19 When questioned, patients will describe a dramatic reduction in the amount of their bench press weight, inability to do push-ups, and overall poorer athletic performance. In the relatively young patient (younger than 35 years) who presents with multiple vague complaints of shoulder pain in the absence of other diagnoses, the diagnosis of posterior instability is often present.
A unique finding in posterior instability is that patients may be able to subluxate “voluntarily” their glenohumeral joint posteriorly. There are two types of voluntary glenohumeral instability—voluntary positional and voluntary muscular.26 Voluntary positional instability is common in posterior instability and is defined by subluxation in a provocative position (flexion, adduction, and internal rotation). Voluntary muscular instability occurs with the arm in an adducted (non–position-dependent) position. Patients with voluntary positional instability who can positionally reproduce their instability should not be excluded from surgical treatment27 and should not be associated with voluntary willful instability.
A comprehensive physical examination is essential for a patient with suspected posterior instability of the shoulder. Both shoulders should be examined, observing any obvious dislocation, asymmetry, abnormal motion, muscle atrophy, swelling, and scapular winging and tracking. The asymptomatic shoulder may be examined first to gain patient confidence and relaxation. The mainstay of diagnosis remains a finding of symptomatic posterior instability in the office setting, which may be confirmed by a translation examination under anesthesia.28
Although an increase in external rotation and mild loss of internal rotation may be observed, range of motion testing in patients with posterior is usually normal and symmetrical.18 Tenderness to palpation at the posterior glenohumeral joint line is common.26
Provocative maneuvers allow a determination of the direction and degree of instability. Common posterior instability tests include the jerk test,29 posterior stress test,30 Kim test,31 and load and shift test.32 The jerk test is performed while the examiner stands next to the affected shoulder. The elbow is grasped in one hand, and the distal clavicle and scapular spine in the other. With the arm in flexion and internal rotation, the flexed elbow is pushed posteriorly while the shoulder girdle is pushed anteriorly. While these forces are applied, the shoulder is abducted. A sudden jerk associated with pain occurs as the subluxated humeral head relocates into the glenoid fossa (Fig. 12-6).
The Kim test is also helpful for diagnosing posterior instability.31 This test is performed with the patient seated and the arm in 90 degrees of abduction. As the arm is passively elevated to 45 degrees of forward flexion, the examiner applies an axial load to the elbow while a downward and posterior force is applied to the upper arm. Pain and posterior subluxation signify a positive test. Combining the Kim and jerk tests has been shown to have 97% sensitivity for posterior instability.
Excessive inferior translation of the humerus on the glenoid is often associated with posterior subluxation33,34 and may indicate bidirectional or multidirectional instability if the inferior sulcus test reproduces the patient’s symptoms. Inferior instability may be demonstrated with the arm in 90 degrees abduction and the application of a downward force on the proximal humerus to cause inferior displacement. If the patient’s symptoms are reproduced, then the diagnosis of multidirectional instability with an inferior instability component should be made (Fig. 12-7).
DIAGNOSTIC IMAGING
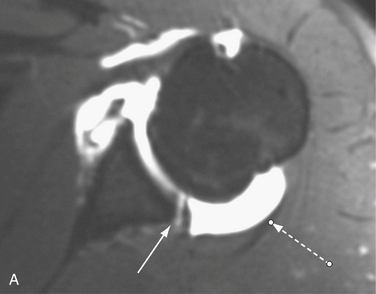
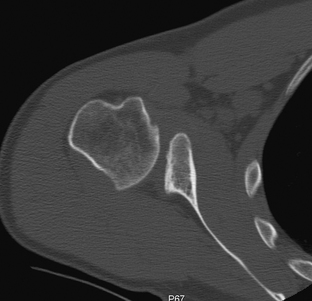
Computed tomography (CT) is useful to evaluate glenoid hypoplasia, glenoid bone loss, and glenoid retroversion. Magnetic resonance imaging (MRI) and magnetic resonance arthrography (MRA) provide visualization of the inferior and posterior capsulolabral structures, biceps anchor, rotator cuff, and rotator interval. Incomplete avulsion of the posterior labrum, a Kim lesion, can be seen as a marginal labral crack on MRA. Findings include a loss of posterior labral height, with incomplete extrusion of contrast into the posterior chondrolabral junction. As in anterior instability, posterior instability may be rarely associated with injury to the capsular insertion on the humerus (a posterior humeral avulsion of the glenohumeral ligament [PHAGL]). In addition, it has been shown that the posterior capsule is enlarged on MRA in patients with posterior instability (Fig. 12-8).3
INDICATIONS AND CONTRAINDICATIONS
Patients with limited function secondary to symptoms of pain and/or instability and who have failed an adequate trial of conservative therapy may be candidates for surgical treatment.18,19 Voluntary instability may not necessarily be a contraindication to surgical treatment.
TREATMENT OPTIONS
Conservative Management
Physical therapy and rehabilitation remain the initial treatment of choice for posterior instability.18,35 Strengthening programs have been shown to diminish pain and/or improve stability in approximately two thirds of patients with posterior and multidirectional instability, and may be particularly beneficial for patients with generalized ligamentous laxity and repetitive microtrauma.19 Nonoperative treatment is less likely to be successful in patients with a history of a traumatic event. Studies have shown a success rate of 70% to 89% for rehabilitation in atraumatic subluxators, with only 16% success in traumatic sublaxators.35
Arthroscopic Treatment
Symptomatic patients who have failed nonoperative treatment are candidates for surgical intervention. Although open procedures are traditionally viewed as the gold standard for anterior instability, open treatment of posterior instability has not fared as well, with a 30% to 70% failure rate. This is likely caused by the larger surgical dissection and biomechanical properties of the posteroinferior capsule and labrum different from those of the anterior structures of the shoulder.33,36–38
Positioning
Although the beach chair and lateral decubitus positions are both effective, the lateral decubitus position more effectively opens up the inferior and posterior quadrants of the shoulder,39 providing ease of access to the entire glenohumeral joint. In the lateral decubitus position, the arm is abducted approximately 50 degrees and flexed 15 degrees by means of balanced suspension with an axillary pillow bump to open the posteroinferior aspect of the shoulder further (Fig. 12-9).
Portal Placement
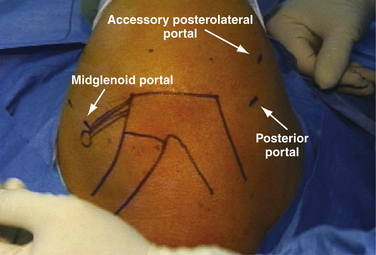
Ease of access to the posteroinferior aspect of the glenohumeral joint is essential to a successful outcome. After diagnostic arthroscopy from the posterior portal, an anterosuperior portal is made for the arthroscopic camera in the superior aspect of the rotator interval.40 A midglenoid portal is also made just above the subscapularis and a 5- to 6-mm cannula inserted (Fig. 12-10). The midglenoid portal is important for ease of labral tear elevation and preparation. Two posterior portals are used to address the posteroinferior pathology, one from the original arthroscopic posterior portal and a second posterolateral portal. The posterolateral accessory portal, also known as the 7 o’clock portal is 2 cm lateral and 1 cm anterior to the original posterior portal or just 2 cm directly lateral to the posterior corner of the acromion. The posterolateral portal is essential for anchor insertion and instrumentation through a cannula to facilitate capsulolabral repair.41
Techniques
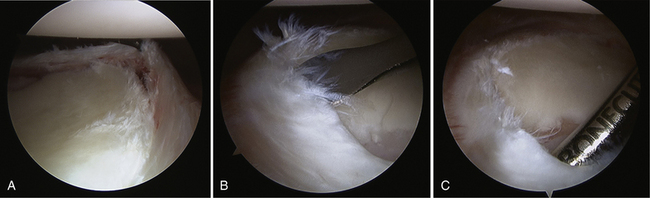
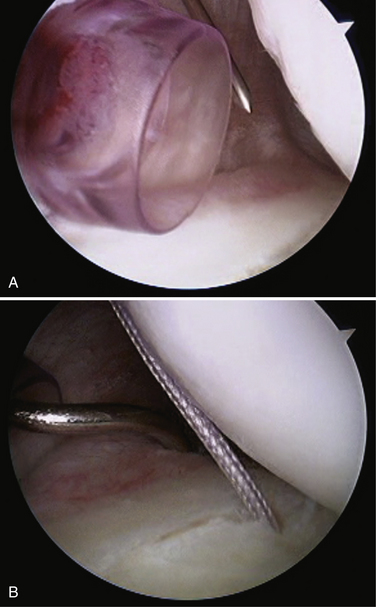
With the arthroscope in the original posterior viewing portal, the posteroinferior labral tear is prepared with an elevator device inserted anteriorly from the midglenoid portal. Although this is not necessarily intuitive, it is much easier to prepare the posterior labrum with an instrument inserted from the anterior midglenoid portal for two reasons. First, the posterior labrum is attached on the glenoid face and can be elevated from the front; using sharp elevator instruments from the posterior can easily tear the labrum.40 Second, the midglenoid portal affords a flat trajectory relative to the glenoid so that the instruments may be easily passed without damaging the glenohumeral chondral surfaces. A shaver or burr and capsular rasp may also be introduced from the anterior midglenoid portal to complete the capsulolabral and bony preparation prior to posterior labral repair (Fig. 12-11).
A capsular plication39 imbricates and closes down the patulous pouch of the shoulder with a suture (absorbable or nonabsorbable) and generally uses an intact glenoid labrum as the fixation point. A capsulolabral repair with anchors uses the glenoid anchor as the fixation point. Patients with an intact labrum are amenable to capsular plication without anchors if the posteroinferior glenoid labrum is completely intact, although this has not been clearly determined. Whereas the labrum has been shown to be a solid fixation point,42 concerns of an unrecognized Kim Lesion,24 suture breakage, small labral tear propagation, and shear stress may serve as indications for anchor fixation. In patients with posterior instability, one should have a low threshold for anchor repair given the high frequency of labral injury and pathology present, which may compromise capsular repair strength.
Determining the amount of capsular plication is one of the biggest challenges in surgical management of posterior instability. Although there is no universally accepted amount, it is generally though that a 1-cm plication results in adequate correction of the underlying pathology.43 The important areas to address with a posterior instability repair are the posteroinferior aspects of the glenohumeral joint, with most of the repair within the posteroinferior quadrant (Fig. 12-12).
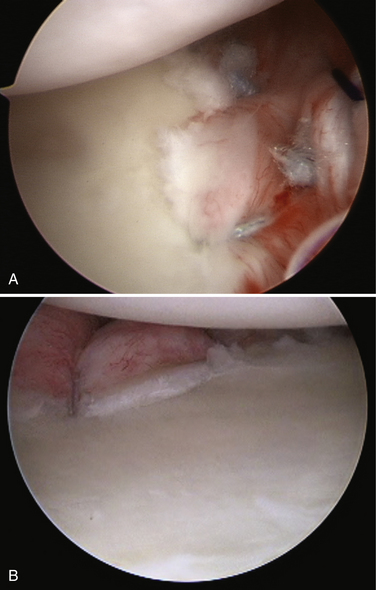
Once the labrum, capsule, and bony glenoid interface are prepared for capsulolabral repair, the arthroscope is introduced into the anterosuperior portal. This allows excellent visualization of the posteroinferior glenohumeral joint and allows maximal working space in the posterior shoulder by freeing up cannula space. The posterior repair is now accomplished with the original posterior portal, which is replaced with an 8.25-mm clear cannula. Although a cannula may be placed in the posterolateral portal, a percutaneous incision for the anchor insertion device is all that is required. The capsulolabral repair is then performed from the posterior portal through the 8.25-mm clear cannula.
The first anchor is inserted through the posterolateral portal via a percutaneous insertion of the sharp anchor guide device. This anchor is positioned at 6 o’clock and placed on the glenoid rim. The capsulolabral repair, of approximately 1 cm of tissue, including the labrum, is then performed and the sutures appropriately shuttled. There are a variety of capsular repair devices and shuttling techniques with which the surgeon should be familiar prior to attempting this in vivo. This process is repeated until three or four anchors have been placed or until the labral tear and capsular pathology have been adequately addressed (Fig. 12-13).
When repairing the posteroinferior capsule, care must be taken to avoid injury to the axillary nerve. The closest point between the glenoid rim and the axillary nerve is approximately 12.5 to 15 mm at the 6 o’clock position.44 Placing the arm in abduction and external rotation with balanced suspension increases the zone of safety during arthroscopic plication.45 The use of thermal devices should be avoided; injuries to the axillary nerve caused by these devices have been described.46
Although closure of the rotator interval has been frequently suggested as a useful adjunct in posterior instability, arthroscopic closure of the rotator interval may not be as biomechanically robust as its open counterpart. Many surgeons have not closed the rotator interval in posterior instability and have obtained excellent results. 20,21,37 The main issue with an arthroscopic rotator interval closure lies in the fact that arthroscopic closure imbricates different structures than in the open technique described by Harryman and coworkers.47 Arthroscopic techniques shift the middle glenohumeral ligament to the superior rotator interval capsule (superior glenohumeral ligament), and do not necessarily imbricate the coracohumeral ligament as described for an open approach. Recent biomechanical evidence48,49 has suggested that arthroscopic rotator interval closure is not very beneficial for improving posterior stability of the shoulder and is not routinely performed on our cases.
PEARLS& PITFALLS
OUTCOMES
In 1998, Wolf and Eakin reported results of arthroscopic capsular plication with suture anchors in 14 patients, of which only 1 patient had continued instability.37 Since then, other authors have published similarly encouraging results. In a series of 33 patients by Provencher and colleagues,21 stability was achieved in 88% of patients, with a mean follow-up of 39 months. Bradley and associates20 have published successful results in 100 athletes, with 89% return to full sports activity and no recurrence of instability.
SUMMARY AND CONCLUSIONS
Posterior instability of the shoulder presents a diagnostic and clinical challenge for orthopedic surgeons because of the relative infrequency of the condition, few reports in the literature, and lack of clear superiority of surgical techniques. It is critical to understand the pathoanatomy, perform careful patient selection, and adhere to techniques designed to address the pathology to obtain a successful outcome. One should carefully assess for posterior shoulder instability in the relatively young athlete who presents with vague complaints of shoulder pain and decreased athletic performance. As arthroscopic stabilization procedures and techniques are refined, improved results for this challenging problem will be forthcoming.
1. Neer CS2nd Involuntary inferior and multidirectional instability of the shoulder: etiology, recognition, and treatment. Instr Course Lect, 34; 1985:232-238.
2. Kim S, Noh K, Park J, et al. Loss of chondrolabral containment of the glenohumeral joint in atraumatic posteroinferior multidirectional instability. J Bone Joint Surg Am. 2005;87:92-98.
3. Dewing C, McCormick F, Bell S, et al. An analysis of capsular area in patients with anterior, posterior, and multidirectional shoulder instability. Am J Sports Med. 2008;36:515-522.
4. Bey MJ, Hunter SA, Kilambi N, et al. Structural and mechanical properties of the glenohumeral joint posterior capsule. J Shoulder Elbow Surg. 2005;14:201-206.
5. Turkel SJ, Panio MW, Marshall JL, Girgis FG. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am. 1981;63:1208-1217.
6. Blasier R, Soslowsky L, Malicky D, Palmer M Posterior glenohumeral subluxation: active and passive stabilization in a biomechanical model. J Bone Joint Surg Am, 79; 1997:433-440.
7. Matsen FA3rd, Chebli C, Lippitt S. Principles for the evaluation and management of shoulder instability. J Bone Joint Surg Am. 2006;88:648-659.
8. Lippitt S, Matsen F Mechanisms of glenohumeral joint stability. Clin Orthop Relat Res (291); 1993:20-28.
9. Soslowsky LJ, Malicky DM, Blasier RB Active and passive factors in inferior glenohumeral stabilization: a biomechanical model. J Shoulder Elbow Surg, 6; 1997:371-379.
10. Ovesen J, Nielsen S. Posterior instability of the shoulder. A cadaver study. Acta Orthop Scand. 1986;57:436-439.
11. Pollock RG, Bigliani LU Recurrent posterior shoulder instability. Diagnosis and treatment. Clin Orthop Relat Res (291); 1993:85-96.
12. Weber SC, Caspari RB. A biomechanical evaluation of the restraints to posterior shoulder dislocation. Arthroscopy. 1989;5:115-121.
13. Lazarus MD, Sidles JA, Harryman DT2nd, Matsen FA3rd. Effect of a chondral-labral defect on glenoid concavity and glenohumeral stability. A cadaveric model. J Bone Joint Surg Am. 1996;78:94-102.
14. Inui H, Sugamoto K, Miyamoto T, et al Glenoid shape in atraumatic posterior instability of the shoulder. Clin Orthop Relat Res (403); 2002:87-92.
15. Metcalf M, Duckworth D, Lee S, et al. Posteroinferior glenoplasty can change glenoid shape and increase the mechanical stability of the shoulder. J Shoulder Elbow Surg. 1999;8:205-213.
16. Itoi E, Motzkin NE, Browne AO, et al. Intraarticular pressure of the shoulder. Arthroscopy. 1993;9:406-413.
17. Robinson CM, Aderinto J, et al. Recurrent posterior shoulder instability. Recurrent posterior shoulder instability. 2005;87:883-892.
18. Fronek J, Warren RF, Bowen M. Posterior subluxation of the glenohumeral joint. J Bone Joint Surg Am. 1989;71-A:205-216.
19. Schwartz E, Warren RF, O’Brien SJ, Fronek J. Posterior shoulder instability. Orthop Clin North Am. 1987;18:409-419.
20. Bradley JP, Baker CL3rd, Kline AJ, et al Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 100 shoulders. Am J Sports Med, 34; 2006:1061-1071.
21. Provencher M, Bell S, Menzel K, Mologne T Arthroscopic treatment of posterior shoulder instability: results in 33 patients. Am J Sports Med, 33; 2005:1463-1471.
22. Bottoni CR, Franks BR, Moore JH, et al. Operative stabilization of posterior shoulder instability. Am J Sports Med. 2005;33:996-1002.
23. Kim S, Ha K, Park J, et al. Arthroscopic posterior labral repair and capsular shift for traumatic unidirectional recurrent posterior subluxation of the shoulder. J Bone Joint Surg Am. 2003;85:1479-1487.
24. Kim SH, Ha KI, Yoo JC, Noh KC Kim’s lesion: an incomplete and concealed avulsion of the posteroinferior labrum in posterior or multidirectional posteroinferior instability of the shoulder. Arthroscopy, 20; 2004:712-720.
25. Vidal L, Bradley JP. Management of posterior shoulder instability in the athlete. Curr Opin Orthop. 2006;17:164-171.
26. Millett PJ, Clavert P, Hatch GF3rd, Warner JJ. Recurrent posterior shoulder instability. J Am Acad Orthop Surg. 2006;14:464-476.
27. Fuchs B, Jost B, Gerber C. Posterior-inferior capsular shift for the treatment of recurrent, voluntary posterior subluxation of the shoulder. J Bone Joint Surg Am. 2000;82:16-25.
28. Cofield R, Irving J. Evaluation and classification of sholder instability. Clin Orthop. 1985;223:32-43.
29. Blasier RB, Soslowsky LJ, Malicky DM, Palmer ML Posterior glenohumeral subluxation: active and passive stabilization in a biomechanical model. J Bone Joint Surg Am, 79; 1997:433-440.
30. Pollock RG, Bigliani LU. Recurrent posterior shoulder instability. Diagnosis and treatment. Clin Orthop Rel Res. 1993;291:85-96.
31. Kim S, Park J, Jeong W, Shin S The Kim test: A novel test for posteroinferior labral lesion of the shoulder—a comparison to the jerk test. Am J Sports Med, 33; 2005:1188-1192.
32. Gerber C, Ganz R. Clinical assessment of instability of the shoulder with special reference to anterior and posterior drawer tests. J Bone Joint Surg Br. 1984;66:551-556.
33. Hawkins R, Koppert G, Johnston G. Recurrent posterior instability (subluxation) of the shoulder. J Bone Joint Surg Am. 1984;66:169-174.
34. Hawkins RH Glenoid osteotomy for recurrent posterior subluxation of the shoulder: assessment by computed axial tomography. J Shoulder Elbow Surg, 5; 1996:393-400.
35. Burkhead W, Rockwood C. Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am. 1992;74:890-896.
36. Tibone JE, Prietto C, Jobe FW, et al. Staple capsulorrhaphy for recurrent posterior shoulder dislocation. Am J Sports Med. 1981;9:135-139.
37. Wolf EM, Eakin CL. Arthroscopic capsular plication for posterior shoulder instability. Arthroscopy. 1998;14:153-163.
38. Hawkins RJ, Janda DH. Posterior instability of the glenohumeral joint. A technique of repair. Am J Sports Med. 1996;24:275-278.
39. Hewitt M, Getelman MH, Snyder SJ Arthroscopic management of multidirectional instability: pancapsular plication. Orthop Clin North Am, 34; 2003:549-557.
40. Provencher M, Romeo A, Solomon D, et al. Arthroscopic preparation of the posterior and posteroinferior glenoid labrum. Orthopedics. 2007;30:904-905.
41. Goubier JN, Iserin A, Duranthon LD, et al. A 4-portal arthroscopic stabilization in posterior shoulder instability. J Shoulder Elbow Surg. 2003;12:337-341.
42. Provencher M, Verma N, Obopilwe E, et al A biomechanical analysis of capsular plication versus anchor repair of the shoulder: can the labrum be used as a suture anchor. Arthroscopy, 24; 2008:210-216.
43. Schneider DJ, Tibone JE, McGarry MH, et al. Biomechanical evaluation after five and ten millimeter anterior glenohumeral capsulorrhaphy using a novel shoulder model of increased laxity. J Shoulder Elbow Surg. 2005;14:318-323.
44. Price MR, Tillett ED, Acland RD, Nettleton GS. Determining the relationship of the axillary nerve to the shoulder joint capsule from an arthroscopic perspective. J Bone Joint Surg Am. 2004;86-A:2135-2142.
45. Uno A, Bain GI, Mehta JA Arthroscopic relationship of the axillary nerve to the shoulder joint capsule: an anatomic study. J Shoulder Elbow Surg, 8; 1999:226-230.
46. Greis PE, Burks RT, Schickendantz MS, Sandmeier R. Axillary nerve injury after thermal capsular shrinkage of the shoulder. J Shoulder Elbow Surg. 2001;10:231-235.
47. Harryman DT2nd, Sidles JA, Harris SL, Matsen FA3rd. The role of the rotator interval capsule in passive motion and stability of the shoulder. J Bone Joint Surg Am. 1992;74:53-66.
48. Plausinis D, Bravman JT, Heywood C, et al Arthroscopic rotator interval closure: effect of sutures on glenohumeral motion and anterior-posterior translation. Am J Sports Med, 34; 2006:1656-1661.
49. Provencher MT, Mologne TS, Hongo M, et al Arthroscopic versus open rotator interval closure: impact on glenohumeral stability and range of motion. Arthroscopy, 23; 2007:583-592.
50. Antoniou J, Duckworth DT, Harryman DT2nd. Capsulolabral augmentation for the management of posteroinferior instability of the shoulder. J Bone Joint Surg Am. 2000;82:1220-1230.