Chapter 21 Posterior Cruciate Ligament
Diagnosis, Operative Techniques, and Clinical Outcomes
INDICATIONS
Complete ruptures to the posterior cruciate ligament (PCL) account for approximately 3% of all knee ligament injuries in the general population.160 However, in the trauma setting, the reported incidence of complete PCL ruptures has been as high as 37% of serious knee-related cases.40 These injuries are classified as either low-velocity in nature, such as those that occur from contact with another player in sports, or high-velocity, such as a dashboard injury in a motor vehicle accident.44 The mechanism of PCL rupture in athletes is usually a fall on the flexed knee with a plantar-flexed foot or hyperflexion of the knee.36 High-velocity injuries frequently involve dislocations with multiple ligament ruptures that require immediate medical attention. In this chapter, the different types of PCL reconstructive techniques are described in detail to allow the surgeon to select the procedure most suited for the specific knee injury. In addition, the initial diagnosis and management of acute PCL ruptures is addressed in the “Preoperative Planning” section.
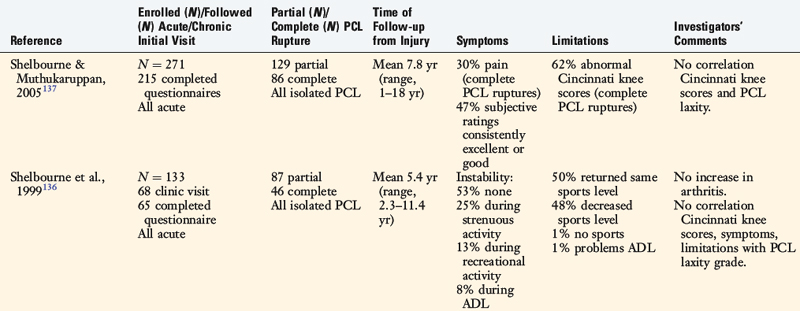
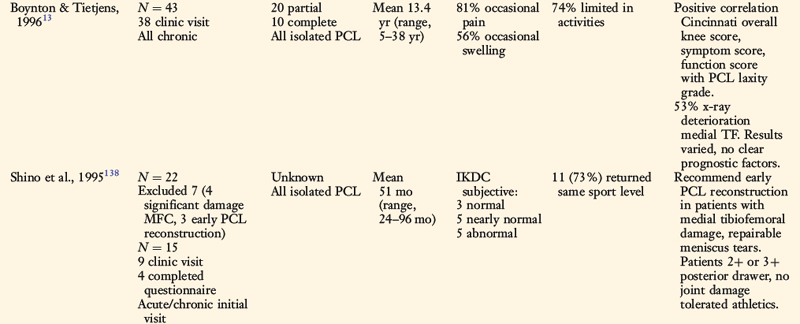
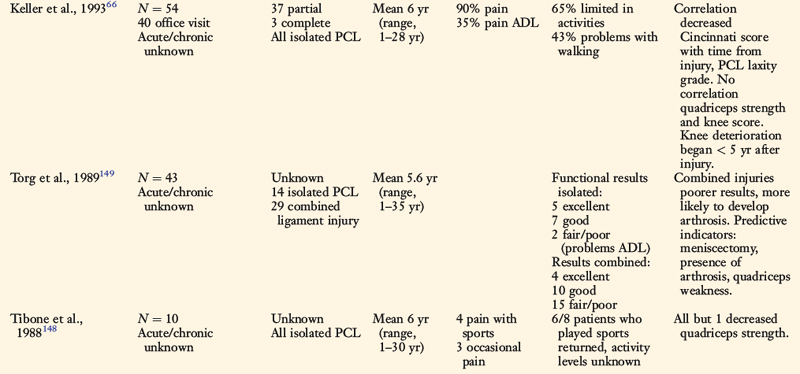
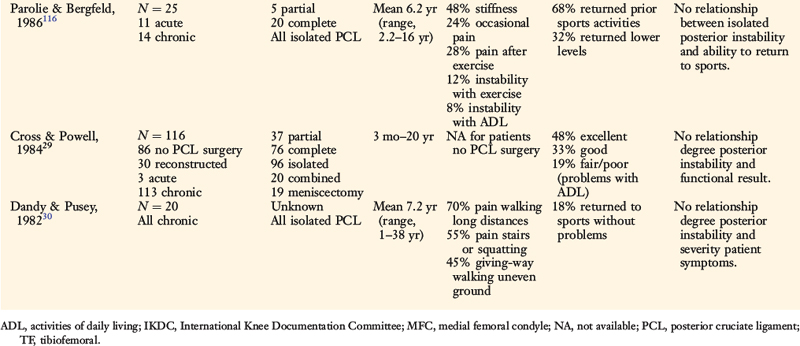
The proper management of complete ruptures to the PCL requires thorough knowledge of anatomy, diagnosis, surgical reconstruction, and rehabilitation concepts. Some aspects of the treatment of complete isolated PCL ruptures are controversial owing to the unknown natural history in regard to long-term symptoms, functional limitations, and risk of joint arthritis. Whereas some studies (that included patients with partial PCL deficiency) report that patients do well when treated conservatively,29,44,116,136–138,148,149 other investigations describe noteworthy symptoms and functional limitations years after the injury that can be disabling13,30,34,66 (Table 21-1). A high percentage of knees with complete PCL ruptures develop articular cartilage deterioration over time that usually occurs on the medial femoral condyle and patellofemoral surfaces owing to increased joint pressures.13,49,50,147 Posterior tibial subluxation after PCL rupture has a deleterious effect to the knee similar to that of a medial meniscectomy, because there is loss of medial meniscus function and increased joint contact stress. There is less of an effect to the lateral meniscus, which retains load-bearing function. Posterior tibial subluxation results in a loss of normal joint kinematics and in coupled external tibial rotation with joint loading. Accordingly, a PCL rupture would be expected to have a more deleterious effect in a varus-angulated knee with associated loss of the medial meniscus and, in particular, larger athletes desiring a return to strenuous athletics. All of these factors alone or together result in substantial medial tibiofemoral loads and risk of joint deterioration.
The indications for surgical reconstruction in knees with a chronic isolated complete PCL rupture are pain and instability with athletics or other activities, swelling, and 10 mm or more of increased posterior tibial translation at 90° flexion (Fig. 21-1). PCL reconstruction is most frequently performed in dislocated knees with gross instability due to other ligament injuries to the anterior cruciate ligament (ACL), medial collateral ligament (MCL; see Chapter 24, Medial and Posteromedial Ligament Injuries: Diagnosis, Operative Techniques, and Clinical Outcomes), or posterolateral structures (see Chapter 22, Posterolateral Ligament Injuries: Diagnosis, Operative Techniques, and Clinical Outcomes). Indications for surgery in acute isolated PCL ruptures are discussed later in this chapter.
If symptomatic meniscal tears or early patellofemoral or tibiofemoral articular cartilage damage is present, early PCL reconstruction is recommended with the goal of decreasing joint deterioration over time. The results of PCL reconstruction in knees with chronic ruptures are not as favorable as those that undergo reconstruction for acute injuries. This is because patients present with pain and swelling due to joint deterioration that often persists even though some benefit may be gained from improved knee stability obtained from the operative procedure.95
CONTRAINDICATIONS
In addition, patients with chronic PCL deficiency who have severe muscle atrophy, loss of knee motion, or hyperextension gait abnormalities require extensive rehabilitation and gait retraining (see Chapter 34, Correction of Hyperextension Gait Abnormalities: Preoperative and Postoperative Techniques) before reconstruction.107
PCL ANATOMY
The PCL arises from a depression posterior to the intra-articular upper surface of the tibia and courses anteromedially behind the ACL to the lateral surface of the medial femoral condyle and is described in detail in Chapter 2, Lateral, Posterior, and Cruciate Knee Anatomy (Fig. 21-2). The PCL has an average length of 38 mm and an average width of 13 mm.51,155 The cross-sectional area of the PCL is variable and increases from tibial to femoral insertions.58 It is approximately 50% larger than the ACL at its femoral origin and 20% larger than the ACL at its tibial insertion.
Critical Points CONTRAINDICATIONS
Critical Points POSTERIOR CRUCIATE LIGAMENT ANATOMY
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
Free nerve endings and mechanoreceptors have been identified in the femoral and tibial attachment sites and on the surface of the PCL.65,131 The mechanoreceptors resemble Golgi tendon organs and are believed to have a proprioceptive function in the knee.67
In a histologic study of the PCL in cadaveric knees, Katonis and coworkers65 reported a neural innervation similar to that of the ACL. Specifically, the PCL contains type I or Ruffini’s corpuscles, which have a slow threshold to pressure changes; type II (Vater-Pacini corpuscles), which are more rapid acting, and type IV (free nerve endings) for pain reception. The mechanoreceptors are located at each ligament bony attachment and on the surface of the PCL.
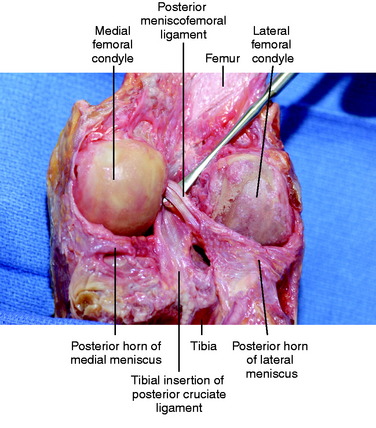
The meniscofemoral ligaments are in close proximity to the PCL. They arise from the posterior horn of the lateral meniscus and insert near the PCL insertion site on the lateral aspect of the medial femoral condyle.58 The anterior meniscofemoral ligament (ligament of Humphry) courses anterior to the PCL, and the posterior meniscofemoral ligament (ligament of Wrisberg) runs obliquely behind the PCL. Frequently, the anterior meniscofemoral ligament interdigitates with the PCL fiber attachments on the medial femoral condyle (Fig. 21-3).87 At least one of the meniscofemoral ligaments is present in 91% of knees, and both ligaments may be found in 50% of knees in young individuals.55,58,87 The biomechanical function of the meniscofemoral ligaments is discussed in detail in Chapter 28, Meniscus Tears: Diagnosis, Repair Techniques, and Clinical Outcomes.
The traditional division of the PCL into separate anterolateral and posteromedial bundles oversimplifies PCL fiber function. The PCL is a complex anatomic structure composed of a continuum of fibers of different lengths and attachment characteristics. The length-tension behaviors of the fibers that resist posterior tibial translation (with knee flexion) are controlled primarily by femoral attachment regions.28,46,54,76,77,129,135,140 The distal fibers lengthen with increasing knee flexion and the proximal fibers shorten with knee flexion.87,129 A detailed description of the length-tension behavior of the PCL appears in Chapter 20, Function of the Posterior Cruciate Ligament and Posterolateral Ligament Structures.
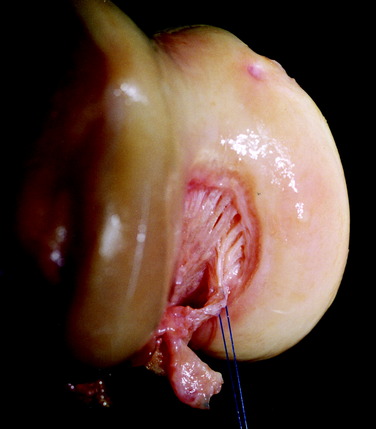
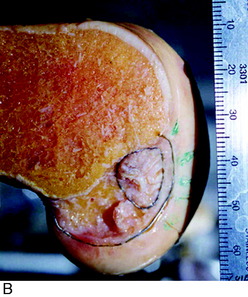
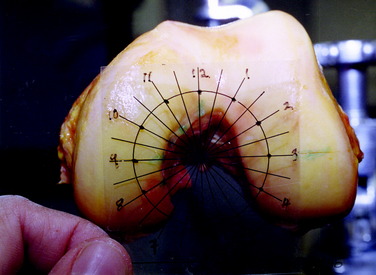
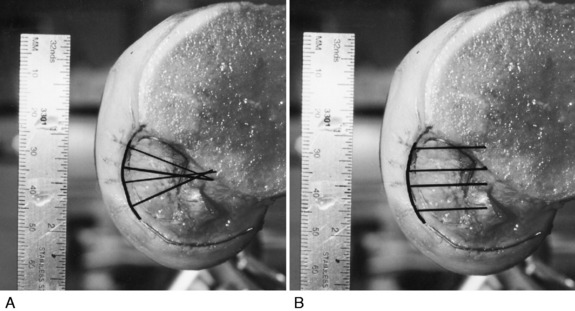
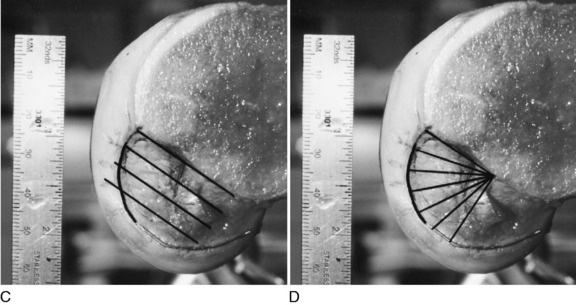
The anatomy of the PCL femoral attachment site has been studied extensively.87,129 Variation exists between knees in the shape of this attachment, from the common elliptical shape to a more rounded and thicker shape (Fig. 21-4).87 Differing measurement systems have been proposed to describe the femoral attachment site. The most accurate of these methods uses a clock reference position (Fig. 21-5), with measurement lines perpendicular to the articular cartilage edge and measurement lines parallel to the femoral shaft (Fig. 21-6).
In general, the PCL attachment extends from high in the notch (11:30 to 5 o’clock position on a right knee) along the medial femoral condyle notch. The anterior portion of the PCL attachment follows the articular cartilage within 2 to 3 mm of its edge and gradually recedes deeper with the notch until, at the 5 o’clock position, the posterior third is 5 mm from the articular margin. Therefore, the distal boundary of the PCL femoral attachment does not parallel the articular margin as reported by others51,154 but is farthest away from the cartilage margin posteriorly.
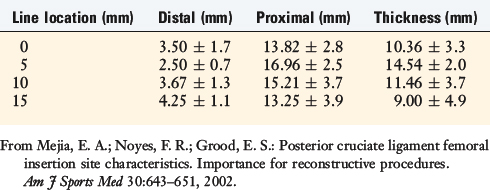
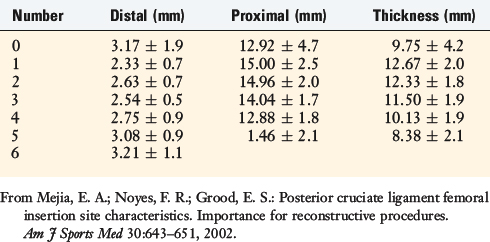
The distance of the distal edge of the attachment to the articular cartilage margin is 3.2 ± 0.8 mm at the roof, 5.8 ± 2.2 mm at its midportion, and 7.9 ± 2.2 mm at its “lowest” extent.129 The distal and proximal measurements for the PCL femoral attachment are shown in Table 21-2. The proximal edge of the PCL is usually straight or partially oval, with the attachment tapered in width along its posterior portion.
TABLE 21-2 PCL Femoral Attachment Measurements Made with the Femoral Condyle Articular Cartilage Clock System
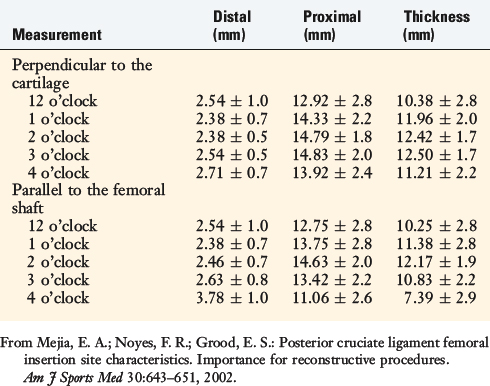
The PCL attachment measurements parallel to the intercondylar roof are shown in Table 21-3. The length of the radial measurement lines extending from the intercondylar roof is shown in Table 21-4. This method provides a means to measure the middle and lower portions of the PCL and provides information on the distance from the lowest cartilage margin to the most posterior portion of the PCL attachment.
The use of measurement lines perpendicular to the cartilage edge is preferred for describing the distal attachments of the PCL (see Fig. 21-6A). The disadvantage of this system is that the 12 o’clock and usually the 1 o’clock measurements cannot be made parallel to the femoral shaft, but must be made perpendicular to the cartilage (Fig. 21-7).
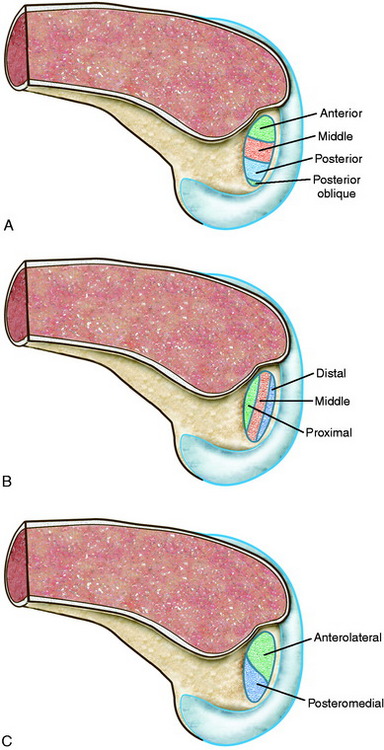
A clear understanding of the anatomy of the native PCL is critical to determining what portion of the ligament will be reconstructed. The terms “high,” “low,” “shallow,” and “deep” are only general descriptors. Because there may be considerable confusion regarding femoral graft tunnel placement during PCL reconstruction, the PCL femoral attachment is described using the rule of thirds (Fig. 21-8A and B) to define the proximal-middle-distal thirds (deep to shallow in the femoral notch) and anterior-middle-posterior thirds (high to low), with a small posterior oblique portion in the sagittal plane.87,91 This provides a grid for the identification of the tunnel locations for the graft strands and is preferred over the historical division of an anterolateral or a posteromedial bundle (see Fig. 21-8C).
It is well appreciated the PCL graft femoral attachment location strongly influences graft tension and the ability of the reconstruction to restore posterior stability.5,47,129,135 Investigations by Grood and associates53 and Sidles and colleagues140 demonstrate that the femoral attachment location determines the graft tibiofemoral separation distance with knee flexion-extension, much more so than the tibial attachment location. The proximal-distal femoral location of a graft has a greater effect on the attachment separation distance than the anteriorposterior (AP) femoral location, which is the basis for the rule of thirds (see Fig. 21-8B). A graft placed in the distal and middle thirds elongates with knee flexion, whereas a graft placed in the proximal third elongates with knee extension. These concepts are used to select PCL graft attachment locations and tensioning described in the “Operative Techniques” section.
VASCULAR ANATOMY AND VARIATIONS
The vascular supply to the cruciate ligaments is provided mostly by the middle genicular artery, which is a branch of the popliteal artery that penetrates the posterior capsule of the knee.4,130 The PCL is covered with a well-vascularized synovial sleeve that contributes to its blood supply. The distal portion of the PCL also receives some vascular supply from capsular vessels originating from the inferior genicular arteries and the popliteal artery.
Detailed knowledge of posteromedial knee anatomy, especially the vascular structures, is required to avoid complications when using a posteromedial approach to a tibial inlay PCL reconstruction (see Chapter 2, Lateral, Posterior, and Cruciate Knee Anatomy). The popliteal artery originates at the adductor hiatus and passes through the popliteal fossa. Before passing deep to the fibrous arch over the soleus muscle, it divides into the anterior and posterior tibial arteries at the distal aspect of the popliteus muscle.
Critical Points VASCULAR ANATOMY AND VARIATIONS
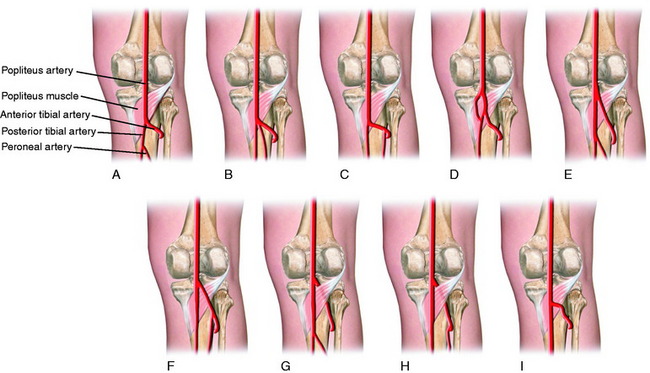
This “normal” vascular pattern has been reported to occur in approximately 88% of cases.31,84 In approximately 5% to 7% of cases, the popliteal artery will divide at least an inch or more proximal to the distal border of the popliteus muscle.26,31,84 In slightly less than half of these cases, with a high division of the popliteal artery, the anterior tibial artery passes anterior, not posterior, to the popliteus muscle belly.153 The number of variations of the anterior tibial artery according to Mauro and coworkers84 is illustrated in Figure 21-9. Therefore, with a tibial inlay approach, the dissection is always proximal to the popliteus muscle with a meticulous technique, because the anterior tibial artery is at risk for transection in approximately 3% to 4% of knees.
An unusual variation in the vascular pattern involves the popliteal artery passing medial and then beneath the medial head of the gastrocnemius. Various subtypes of this abnormal pattern have been described. An abnormal vascular pattern may manifest clinically as the popliteal artery entrapment syndrome, which is characterized by vascular claudication symptoms.70,125,143 Arterial insufficiency occurs most commonly with entrapment of the artery deep to the medial gastrocnemius muscle, but can also occur when the artery is entrapped deep to the popliteus muscle (persistence of ventral component of artery) or deep to an abnormal accessory head of the gastrocnemius. A history of pain in the lower extremity with activity and disappearance with rest, particularly in a young patient, should alert the surgeon to the possibility that an abnormal vascular pattern may exist. Further evaluation with magnetic resonance imaging (MRI) or angiography may be warranted.45,74
The anterior tibial artery arises as a branch of the popliteal artery and initially courses anterior to the popliteus muscle. In humans, the early anterior tibial artery is replaced with the superficial popliteal artery and passes posterior to the popliteus muscle, which then gives rise to the anterior tibial artery. Furthermore, during embryonic life, the medial head of the gastrocnemius migrates medially and cranially. It is with this migration that the popliteal artery can be caught and swept medially with the muscle.84,125
CLINICAL EVALUATION
Physical Examination
A comprehensive examination of the knee joint is required to detect all abnormalities. This includes assessment of (1) the patellofemoral joint and extensor mechanism malalignment, which may occur if increased external tibial rotation exists owing to posterolateral ligament injury that accompanies the PCL rupture; (2) patellofemoral and tibiofemoral crepitus, indicative of articular cartilage damage; (3) gait abnormalities (excessive hyperextension or varus thrust) during walking and jogging107; and (4) abnormal knee motion limits and subluxations compared with those of the contralateral knee.109
Experienced clinicians are aware that patients with chronic deficiency of the PCL and posterolateral structures may develop an abnormal gait pattern characterized by excessive knee hyperextension during the stance phase.107 Subjective complaints of knee instability and giving-way during routine daily activities, along with severe quadriceps atrophy, often accompany this gait abnormality. Gait analysis and retraining are required in patients who demonstrate abnormal knee hyperextension patterns before proceeding with any ligament reconstruction (see Chapter 34, Correction of Hyperextension Gait Abnormalities: Preoperative and Postoperative Techniques).107 The failure to do so may lead to failure of reconstructed ligaments if the abnormal gait pattern is resumed postoperatively.
Diagnostic Clinical Tests
The medial posterior tibiofemoral step-off on the posterior drawer test is performed at 90° of flexion. The amount of posterior tibial translation will vary between knees with isolated PCL ruptures due to physiologic laxity or injury to the secondary posterolateral or medial soft tissue restraints. Posterior tibial translation progressively increases with injury to the secondary restraints. The importance of determining abnormal medial or lateral joint opening and increases in external-internal tibial rotation cannot be overemphasized, because the failure to correct these associated subluxations places PCL graft reconstructions under high in vivo forces postoperatively and risk of graft failure. The diagnostic tests and their interpretation are discussed in Chapter 20, Function of the Posterior Cruciate Ligament and Posterolateral Ligament Structures, and are shown in Table 22-1.
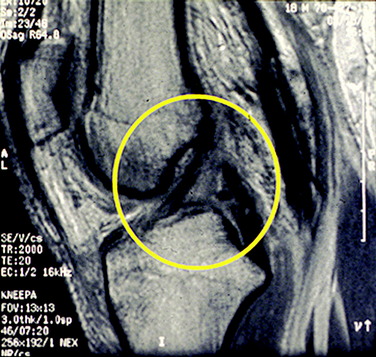
The exact determination of the extent of a PCL tear (partial vs. complete) can be difficult, but is essential from a therapeutic standpoint. The clinical posterior drawer test can be highly subjective, with the forces applied too variable to allow accurate determination of the status of the PCL. MRI is not always accurate in diagnosing partial PCL tears (Fig. 21-10). Frequently, this test may indicate that the ligament is completely ruptured; however, ligament continuity may still exist with some portions functioning to limit posterior tibial subluxation to only a few millimeters. Patten and associates117 reported only a 67% sensitivity rate of the ability of MRI to distinguish complete from partial PCL tears by identifying focal areas of ligamentous discontinuity.
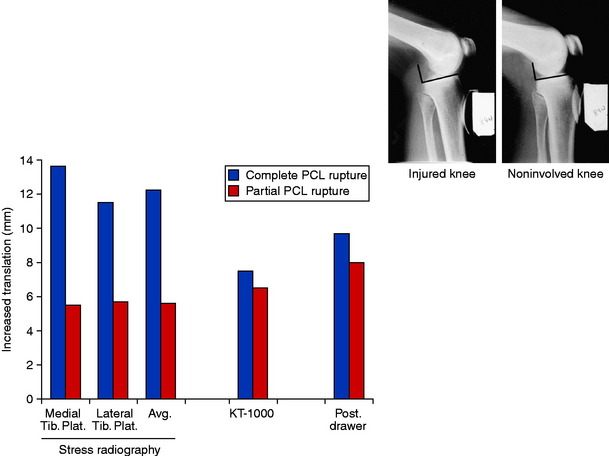
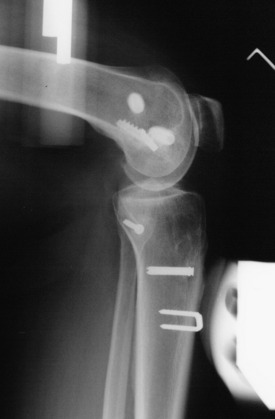
The quantitative measurement of posterior tibial subluxation in knees with PCL ruptures or reconstruction is therefore important.60 The knee arthrometer is the most frequently used device to measure posterior tibial translation after PCL injury and reconstruction. However, the knee arthrometer underestimates the true amount of posterior translation in PCL-deficient and reconstructed knees, often by several millimeters.60,78,146 Stress radiography is the most accurate and reproducible technique currently available,37,43,60,78,119,132 yet only a few studies to date have used this method to document posterior tibial translation after PCL reconstruction. The authors recommend that PCL clinical investigations incorporate stress radiography to provide a more valid measure of posterior tibial translation (Fig. 21-11). To correct for tibal rotation, which can produce errors in measurement, the radiograph should be as close to a pure lateral as possible, with the two femoral condyles superimposed upon themselves. A horizontal line is placed across the medial tibal plateau and a perpendicular line determines the posterior position of each femoral condyle. A similar measurement is made for the most posterior position of the medial and lateral tibial plateau. The amount of tibial translation is the average of both of these measurements.
The tibiofemoral rotation dial test at 30° and 90° is done to determine whether increases in external tibial rotation exist with posterior subluxation of the lateral tibial plateau (see Fig. 22-3).109 This test is described in further detail in Table 22-1.
Radiographic Assessment
Posterior stress radiographs are done with an 89-N force applied to the proximal tibia.60 A lateral radiograph is taken of each knee at 90° of flexion. The limb is placed in neutral rotation with the tibia unconstrained and the quadriceps relaxed. The difference in posterior tibial displacement between the reconstructed knee and the contralateral knee is recorded. More than 8 mm of increase in posterior tibial translation on stress testing indicates a complete PCL rupture.132
Full standing radiographs of both lower extremities, from the femoral heads to the ankle joints, are done in knees in which varus lower extremity alignment is detected on clinical examination. The mechanical axis and weight-bearing line are measured to determine whether HTO is indicated before PCL reconstruction (see Chapter 31, Primary, Double, and Triple Varus Knee Syndromes: Diagnosis, Osteotomy Techniques, and Clinical Outcomes).35,105 If the varus malalignment is not corrected, there is a risk that either a PCL or an ACL graft may fail owing to the varus thrusting forces and concurrent increased lateral joint opening producing high graft tension loads.96
Patients complete questionnaires and are interviewed for the assessment of symptoms, functional limitations, sports and occupational activity levels, and patient perception of the overall knee condition according to the Cincinnati Knee Rating System (CKRS).6
PREOPERATIVE PLANNING
Acute Ruptures of the PCL
Controversy exists in the treatment of midsubstance complete PCL ruptures, primarily owing to the lack of a scientifically-proven operative procedure that can predictably restore posterior stability and PCL function. In comparison, surgical procedures to reattach the native PCL in cases of bony avulsion injuries or peel-off injuries directly at the PCL attachment site have more predictable healing rates.12,73,151,152 Even in cases of PCL rupture directly at the attachment site, usually sufficient ligament substance remains for a direct repair. In select situations, an augmentation using the semitendinosus tendon may facilitate PCL repair.
Augmentation of partial PCL tears is controversial.3,63,156 Graft reconstruction of the so-called posteromedial portion of the PCL has been described in which the “anterolateral bundle” is still intact and functional. The authors have no experience with this technique and have not performed augmentation procedures in the acute setting. Stress radiography plays an important role in determining whether an abnormal increase of 10 mm or more exists, indicating loss of PCL function. Partial ligament tears are treated conservatively with an extension brace and posterior calf pad to allow for potential PCL healing.
Critical Points PREOPERATIVE PLANNING
Acute Ruptures
 2 wk: 0°–90° of motion maintaining anterior tibial translation load. Patient sleeps in brace, no unsupervised knee motion.
2 wk: 0°–90° of motion maintaining anterior tibial translation load. Patient sleeps in brace, no unsupervised knee motion. 4 wk: active quadriceps extension out of brace, 50% weight-bearing, crutch support, maintain brace protection.
4 wk: active quadriceps extension out of brace, 50% weight-bearing, crutch support, maintain brace protection. 5–6 wk: wean from the brace and crutch support, rehabilitation (see Chapter 23, Rehabilitation of Posterior Cruciate Ligament and Posterolateral Reconstructive Procedures).
5–6 wk: wean from the brace and crutch support, rehabilitation (see Chapter 23, Rehabilitation of Posterior Cruciate Ligament and Posterolateral Reconstructive Procedures).Chronic Injuries
MRI, magnetic resonance imaging; PCL, posterior cruciate ligament.
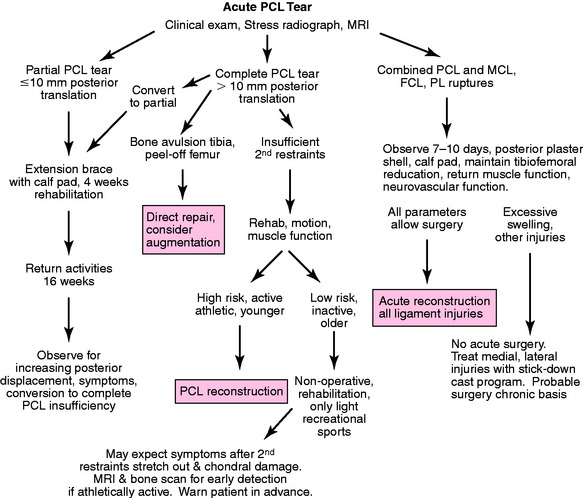
The treatment rationale for patients with acute PCL ruptures is shown in Figure 21-12. The algorithm is divided into three major sections based on the PCL tear (partial, complete, or combined with other ligament ruptures). The 10-mm division is somewhat arbitrary. As discussed, stress radiography is helpful in determining the exact increase in posterior tibial translation. The rules to treat partial or acute isolated PCL tears are
In the authors’ experience, 4 weeks of protection to allow initial healing of a complete PCL rupture will frequently restore partial PCL function, with less than 10 mm residual posterior tibial subluxation. The initial PCL healing process involves a low tensile strength and an additional 4 to 6 weeks of protection is recommended, including avoiding athletics, running, walking on downhill grades, walking down stairs, or other high knee flexion activities that load the PCL. Even in knees with a complete PCL tear and more than 10 mm of increased posterior tibial displacement, healing of the disrupted PCL fibers may still occur, although a residual posterior tibial subluxation of a few millimeters (with a hard endpoint) will remain. These knees in which partial PCL function has been restored should be followed and repeat stress radiographs obtained at 6 months and over the next few years to determine PCL function. These partial PCL tears seldom require reconstruction. However, Shelbourne and associates136,137 described that one third or more of patients in this group have abnormal knee scores and pain with athletic activities owing usually to concomitant articular cartilage damage. A repeat MRI with fast-spin-echo cartilage sequences122 helps determine the integrity of the articular cartilage and provides important information for counseling the patient on athletic activities to decrease the risk of future joint arthritis.
In cases of complete isolated midsubstance PCL ruptures that have more than 10 mm of increased posterior tibial displacement in which the patient is seen late after the injury and the previously discussed program cannot be instituted, one treatment approach in athletes and those in strenuous high-risk occupations is PCL graft reconstruction before the secondary restraints stretch out with subsequent reinjury. The authors believe that, in athletic individuals, PCL reconstructive procedures have advanced to the point at which more predictable results can be expected to restore sufficient PCL function to prevent gross posterior tibial subluxation. Studies have demonstrated, at least in the short term, that the majority of patients with acute PCL ruptures treated with reconstruction are able to return to various levels of sports activities.95 Additional factors to be weighed in the decision to perform early surgery on an isolated PCL rupture (with > 10 mm posterior displacement, 90° flexion) include athletic goals, body weight, medial meniscus or tibiofemoral joint damage, patellofemoral joint damage, and varus malalignment; these factors add to the effects of the residual posterior subluxation in increasing knee joint loads and subsequent joint deterioration. Future long-term clinical studies will confirm the importance of these factors in the operative decision of early restoration of PCL function in active younger individuals who subject their knee to high forces in sports or work activities. Sedentary patients with a complete PCL rupture and more than 10 mm of posterior translation (90° flexion) are not considered surgical candidates; however, they are followed as previously described.
Patients with a PCL disruption and other ligament injuries have an obvious posterior tibial dropback without a firm endpoint on posterior drawer testing, and 10 mm or more of posterior tibial subluxation. In almost all of these knees, some increase in medial or lateral joint opening or external tibial rotation can be detected, although the findings may be subtle. There may be physiologic laxity of other ligament structures without a true injury (see Chapter 3, The Scientific Basis for Examination and Classification of Knee Ligament Injuries) that allows for the gross posterior tibial subluxation.
In knees that present with acute disruption of the PCL and medial or posterolateral structures, reconstruction should be delayed until the neurovascular status and other injuries are resolved and major knee ligament surgery can be safely performed. In knees that have associated posterolateral ruptures, acute anatomic repair is required within 14 days before scarring occurs and the ability to anatomically restore these structures is lost (see Chapter 22, Posterolateral Ligament Injuries: Diagnosis, Operative Techniques, and Clinical Outcomes). A similar situation exists for the medial ligament structures; however, these tissues are easier to reconstruct later if surgery cannot be performed in the ideal time period for anatomic repair. There may exist a displaced meniscus tear requiring early treatment. As a word of caution, a displaced meniscus should be reduced into the tibiofemoral joint by 3 weeks to prevent meniscus shortening and scarring that compromises a future repair and results in loss of meniscus function. Even in knees that have marked soft tissue swelling and edema, and in which major ligament reconstruction is contraindicated, a meniscus repair procedure using all-inside techniques can be performed to reduce the meniscus to a normal tibiofemoral position. The mistake is to wait until 6 weeks or later, expecting that the meniscus repair can be performed at that time.
Too frequently, major ligament surgery in dislocated knees performed under acute conditions results in joint arthrofibrosis, compromising the result. Patients should be carefully selected for acute multiligament repairs, realizing that there are proven techniques for reconstruction of the ruptured ligaments performed later under more ideal conditions. When surgery is performed on acute combined PCL and posterolateral ruptures, the procedure includes the use of appropriate grafts to restore lateral stability and allow an early protected range of knee motion program, described in Chapter 22, Posterolateral Ligament Injuries: Diagnosis, Operative Techniques, and Clinical Outcomes. The majority of acute knee dislocations should be treated in a staged approach by first treating the acute injury and then determining whether a ligament reconstruction should be performed either within the 10- to 14-day envelope or delayed. When early surgery is not advisable, the knee is protected for the first 4 weeks to prevent posterior tibial subluxation, as already described for acute isolated PCL ruptures. A lateral radiograph is obtained with the knee placed in a posterior plaster shell and a soft bolster positioned beneath the calf to prevent posterior tibial subluxation. The capsular tissues heal in 7 to 10 days to provide enough stability to prevent recurrence of dislocation.
If a nonoperative approach is selected with associated MCL and posteromedial capsular disruptions, the same program is followed with the lower limb placed in a cylinder cast to allow “stick-down” of the medial soft tissues. Plaster immobilization is required because a soft hinged brace, even if maintained at 0° of extension, does not provide sufficient protection to maintain medial joint line closure to allow the disrupted medial tissues to heal. At 7 to 10 days, the cylinder cast is split into an anterior and a posterior shell and the therapist assists the patient with range of motion from 0 to 90° in a figure-four position with the hip joint externally rotated to protect the healing medial tissues. This program of “aggressive” nonoperative treatment of associated medial ligament injuries is described in further detail in Chapter 25, Rehabilitation of Medial Ligament Injuries.
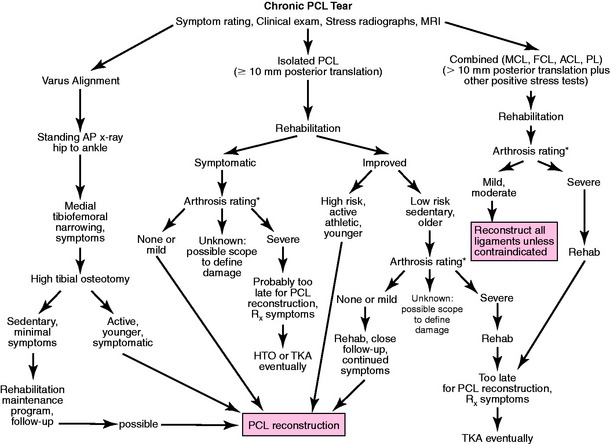
Chronic Ruptures of the PCL
The algorithm for the treatment of chronic PCL ruptures is shown in Figure 21-13. The symptoms and clinical examination determine the functional limitations, particularly the component of symptoms due to medial tibiofemoral or patellofemoral arthritis because these problems are likely to persist after surgical stabilization. Knees with chronic PCL ruptures are arbitrarily divided into three categories; those with varus osseous malalignment (and, rarely, valgus malalignment) in which an osteotomy must be considered, those with an isolated PCL rupture in which reconstruction may or may not be necessary, and those with significant combined ligament injuries that require reconstruction.
If a nonoperative approach is elected, the clinician should warn the patient that the return to athletic activities may carry an uncertain prognosis, and that although sports may be resumed in the short term, some form of joint arthritis will eventually ensue. It is therefore important to follow the patient at regular intervals. A bone scan may be used to provide some indication of abnormal blood flow dynamics; however, it is the authors’ experience that the onset of pain and swelling usually indicates more advanced joint damage and a poor prognosis after PCL reconstruction. An MRI with fast-spin-echo sequences122 provides a baseline for repeated studies at 1- to 2-year intervals. The nonoperative treatment protocol of chronic PCL injuries involves educating the patient to avoid activities such as lunges and other high knee flexion activities that increase posterior tibial subluxation.
INTRAOPERATIVE EVALUATION
Critical Points INTRAOPERATIVE EVALUATION
All knee ligament subluxation tests are performed after the induction of anesthesia in both the injured and the contralateral limbs. The amount of increased anterior tibial translation, posterior tibial translation, lateral joint opening, medial joint opening, and external tibial rotation is documented. In acute knee injuries, arthroscopic pressure is maintained at a low setting with adequate outflow at all times to prevent fluid extravasation. A thorough arthroscopic examination should be conducted, documenting articular cartilage surface abnormalities112 and the condition of the menisci.
The medial and lateral tibiofemoral gap test is done during the arthroscopic examination (see Fig. 22–2).103 The knee is flexed 30° and a varus and valgus load of approximately 89 N is applied. A calibrated nerve hook is used to measure the amount of lateral and medial tibiofemoral compartment opening. Twelve millimeters or more of joint opening at the periphery of the compartment indicates the need for a combined lateral or medial ligament reconstructive procedure to protect and unload the PCL reconstruction. The goal is to restore the function of all ligament structures to normal or nearly normal and not leave a knee with a residual ligament insufficiency. This also applies to the ACL, which is reconstructed at the time of PCL surgery, if deficient.
OPERATIVE TECHNIQUES
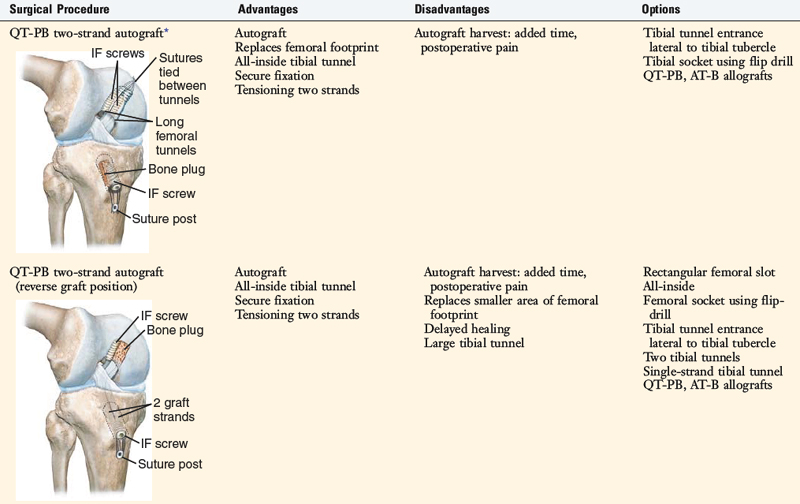
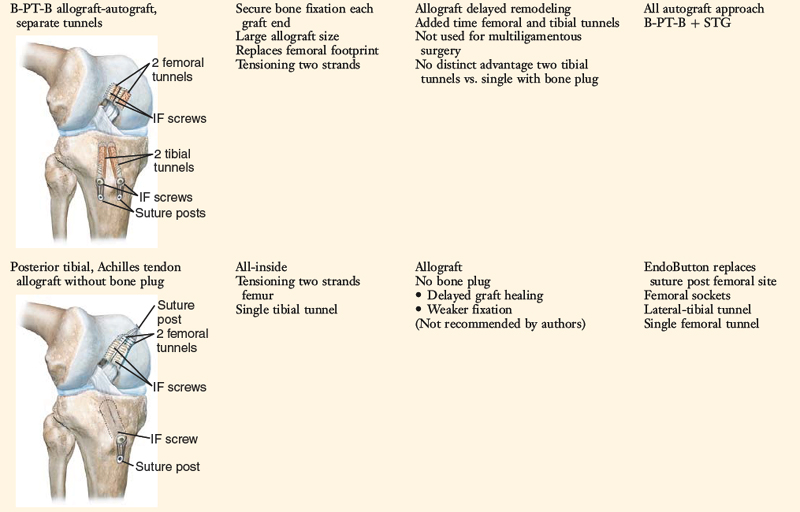
PCL operative techniques continue to evolve, and clinical outcome studies remain limited to allow precise decision making. This chapter describes the senior author’s recommended surgical approach and relative advantages and disadvantages of each procedure, realizing that this is an evolving treatment approach (Table 21-5).
| All-Inside |
| Single-Tunnel Tibial Approach |
Selection of Tibial Attachment Techniques: Arthroscopic All-Inside versus Open Tibial Inlay Approach
Combined ligament injuries, particularly those involving medial ligament and muscle tissues, have a high rate of postoperative motion problems and arthrofibrosis. In these knees, an open posterior tibial inlay procedure and popliteal dissection may be avoided by using the all-inside arthroscopic approach. One exception is a PCL avulsion fracture from the tibial attachment. Another exception is a PCL revision knee in which a prior tibial tunnel was used and a tibial inlay graft is required to bypass this tunnel. In these cases, loss of the normal bony architecture about the posterior tibial PCL attachment may exist and a tibial inlay bone graft is required. In other PCL revision cases that have enlarged tibial tunnels, a staged bone graft procedure may be indicated with the preference to use autogenous bone (limited iliac crest graft; see Chapter 31, Primary, Double, and Triple Varus Knee Syndromes: Diagnosis, Osteotomy Techniques, and Clinical Outcomes), supplemented with allograft bone when required. The bone grafting of the enlarged or misplaced tibial tunnel is first done from an anterior approach. After the tunnel has healed, either a tibial tunnel or a tibial inlay PCL reconstruction may be performed as indicated.
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
The posteromedial tibial inlay technique places a tibial inlay graft securely into the posterior PCL tibial attachment site. This approach is often selected when only the PCL requires reconstruction. The tibial inlay graft provides ideal graft fixation and early healing. A two-strand autogenous QT-PB graft with two femoral tunnels is described and results have been published.92,93
Biomechanical studies of PCL reconstructions also show the potential for graft abrasion and failure at the femoral attachment.134 Operative techniques to protect against graft failure and abrasion are necessary at both tibial and femoral attachment sites.
Selection of PCL Femoral Attachment Techniques: Two-Tunnel versus Single-Tunnel Options
It is not difficult from a technical standpoint to use two well-placed femoral tunnels within the PCL femoral footprint from outside-in, and this is the most ideal technique to master. When the tibia inlay or tibial tunnel bone plug two-strand graft procedure is selected, two femoral tunnels are created using the outside-in technique with a limited anteromedial subvastus approach, described later. This allows graft tensioning, a long femoral tunnel for graft incorporation, and graft fixation with a suture post. This is the author’s preferred technique with either an autograft or an allograft (see Table 21-5).
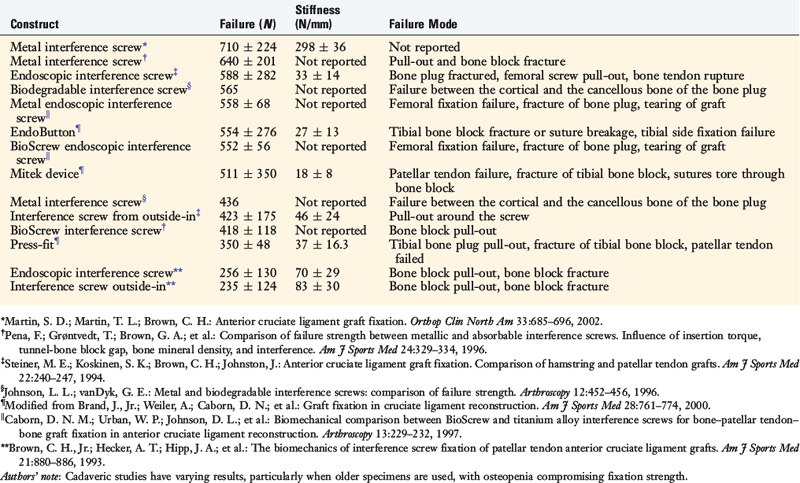
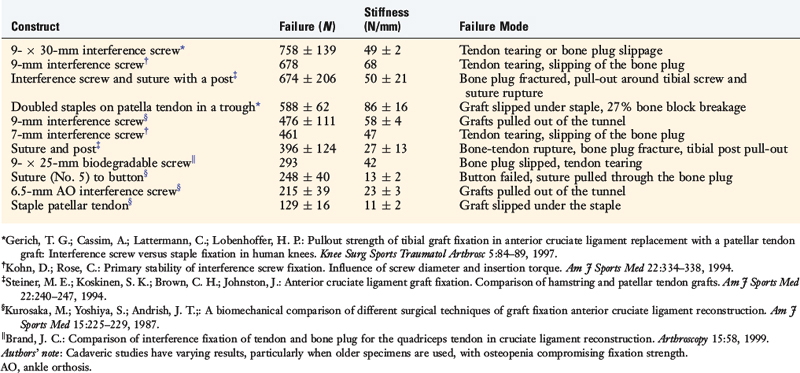
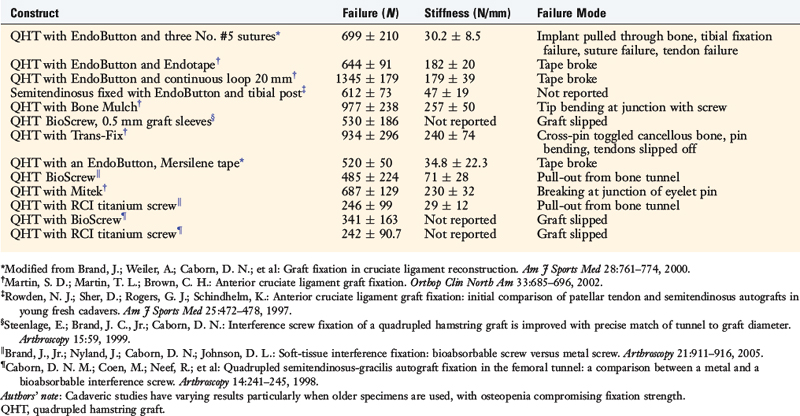
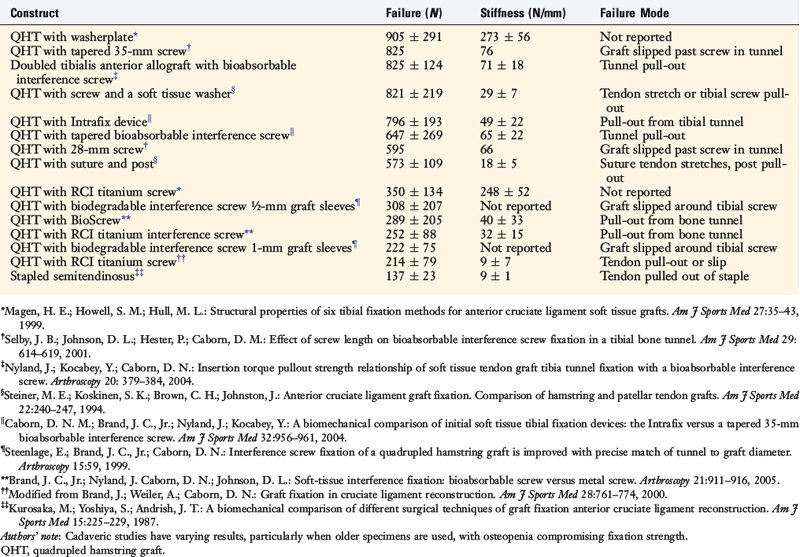
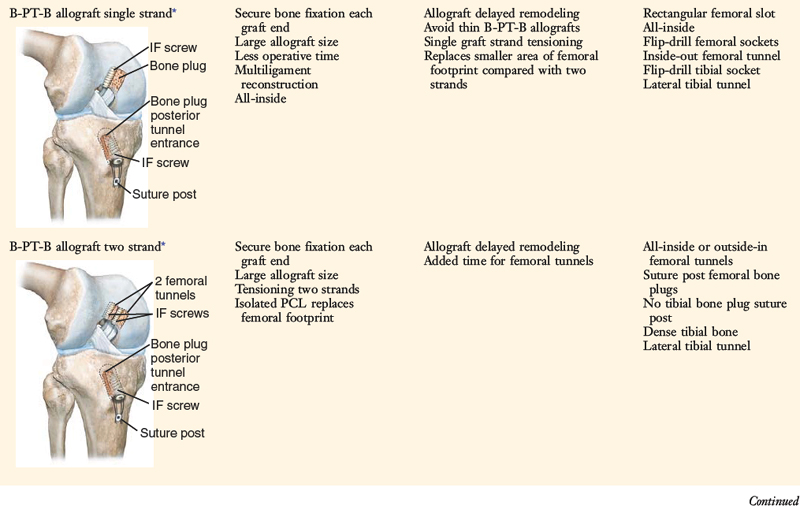
The options for femoral and tibial fixation for a bone–patellar tendon–bone (B-PT-B) graft are shown in Tables 21-6 and 21-7, respectively.14 Techniques are available for inside-out drilling of tunnels and fixation of soft tissue grafts at the femoral attachment site using interference screws (similar to that performed in ACL reconstructions).61 However, these techniques result in lower attachment strength. The outside-in approach allows graft sutures and a suture post to be incorporated (Tables 21-8 and 21-9). PCL reconstructions are under high in vivo loads (see Chapter 20, Function of the Posterior Cruciate Ligament and Posterolateral Ligament Structures) and it is advantageous to select graft fixation methods that provide for maximum tensile strength of the graft construct.17,82,142
Selection of Single-Strand versus Two-Strand PCL Graft Constructs
The advantages and disadvantages of one- and two-strand PCL graft techniques are summarized in Table 21-10. The goal of adding a second strand is to place additional collagenous tissue within the PCL footprint to increase the cross-sectional area of the graft and more closely replicate the native PCL attachment. This theoretical advantage is sometimes referred to as the mass action effect of adding additional collagen within the PCL footprint. The improved stability and clinical success of a two-strand graft construct over those of a single-strand graft have not been proved from a clinical standpoint. Some clinical studies show that a single graft strand obtains results similar to those of a two-strand procedure.
TABLE 21-10 Basis for the Selection of One- Versus Two-Strand Posterior Cruciate Ligament Reconstruction
| Single-Strand | Two-Strand | |
|---|---|---|
| Greater area | – | + |
| Load-sharing (decreased tensile forces in each graft strand) | – | + |
| Operative complexity | + | – |
| Cyclic fatigue | – | + |
| Clinical results (residual posterior tibial translation)* | Unknown | Unknown |
+ Denotes relative advantage; – denotes relative disadvantage.
* Proven by objective measurements, including stress radiography at 90° of knee flexion.
The incorporation of a second graft strand has the theoretical advantage of providing additional collagen tissue for load-sharing, which decreases stress in the collagen fibers, increases graft strength, and reduces cyclic fatigue of the graft construct.134,159 The two graft strands are tensioned at surgery to share loads, which decreases the loads compared with those of a single PCL graft construct. This has been shown in a majority, but not all,81 biomechanical studies that compared single- and two-strand graft constructs. Studies report that the two graft strands placed in the distal two thirds of the PCL femoral footprint will function to resist posterior tibial translation with increasing knee flexion (see Chapter 20, Function of the Posterior Cruciate Ligament and Posterolateral Ligament Structures). Alternatively, when two graft strands are placed in a proximal and distal (deep and shallow) portion of the PCL footprint, graft loading is in a reciprocal manner and the graft strands are under higher loads, which is less ideal. As previously noted, the length and tension changes in grafts is governed for the most part by the femoral attachment, and any graft fibers in the distal two thirds are subjected to increasing tension and elongation with knee flexion.53,140
PCL, posterior cruciate ligament; QT-PB, quadriceps tendon-patellar bone.
In Chapter 20, Function of the Posterior Cruciate Ligament and Posterolateral Ligament Structures, the function of PCL grafts is described in detail. The usual description of a posteromedial bundle that resists tension with knee extension and an anterolateral bundle that resists tension with knee flexion represents an oversimplification and an inaccurate representation of PCL fiber behaviors. In this chapter, the rule of thirds (see Fig. 21-8) is used to describe PCL fiber and graft function.
In a cadaveric study, Bergfeld and coworkers10 reported that both single- and two-strand PCL reconstruction restored translation after PCL sectioning, and suggested that the additional strand may have no benefit. The same-diameter Achilles graft was used so that additional graft material was not added by the second strand. However, the graft forces were not measured and it was not determined whether the second strand resulted in a decrease in graft tensile forces. Studies show that a single graft will restore posterior translation limits to normal after PCL sectioning11,77,135; however, commonly at the expense of high graft tensile forces. Therefore, the theoretical advantage of the second graft strand is to lower the high graft forces placed on a single graft strand and decrease graft failure from cyclic loading (see Chapter 20, Function of the Posterior Cruciate Ligament and Posterolateral Ligament Structures).
In a cadaveric study, Harner and associates56 reported that a single-strand PCL reconstruction did not restore normal posterior tibial translation or joint kinematics. These investigators found that a two-strand PCL reconstruction did restore posterior tibial translation to normal values. The difference found between the single- and the two-strand constructs may have been due to inadequate tensioning of the grafts. The single-strand grafts were tensioned to 88 N at 90° of knee flexion. The tension required to restore posterior tibial translation was not measured and would have required higher graft loads. The added 67-N tensioning of the second posterolateral graft strand provided the additional resistance to restore the tibia to a normal posterior position. Thus, the authors did not truly compare the single- and two-strand PCL graft constructs under the same loading conditions.
A justification to add a second PCL graft stand is the frequent notation in clinical studies that at high knee flexion angles, there is a residual posterior tibial drop-back in the majority of PCL reconstructions.95 There is no question that current PCL surgical procedures are not uniformly accomplishing a functional restoration of normal joint kinematics and stability postoperatively. This is further discussed in detail in the “Authors’ Clinical Studies” section of this chapter. The concern is that residual posterior tibial displacement decreases the ability of the medial meniscus, and perhaps the lateral meniscus as well, to function,118 thereby increasing tibiofemoral contact pressures.72,141 Increases in patellofemoral contact pressures have also been reported.50
In summary, there appear to be sound theoretical reasons to warrant a two-strand PCL reconstruction when clinically feasible. These conditions include isolated PCL reconstructions when the added time required to perform a two-strand PCL graft does not represent a contraindication in terms of operative time and complexity. In multiligament reconstructions, the primary goal is to repair and reconstruct all ruptured ligaments. Adding a second femoral tunnel, and tensioning and securing two graft strands, may be time-consuming in an already complex surgical reconstruction. Therefore, the surgeon should be prepared, based on the operative findings, to modify the preoperative plan when required. In certain multiligament-injured knees, a single-strand PCL graft construct may offer a reasonable opportunity to restore functional stability (Fig. 21-14).81 Given the complex PCL fiber microgeometry, either a single- or a two-strand graft construct still represents an imperfect substitution, providing only a check-rein effect in controlling joint motions and subluxations.
Selection and Preparation of PCL Grafts for Tibial Inlay and All-Inside Techniques
The mechanical properties of grafts commonly used to reconstruct the PCL are shown in Table 21-11. The goal of PCL surgery is to select a graft that matches the structural properties of the PCL as closely as possible. The problem is that the PCL is a highly complex ligament composed of fibers of different lengths that are brought into the loading configuration based on the knee flexion and tibial rotation positions. The data show initial graft mechanical properties that are expected to decline after graft implantation and in vivo remodeling. It is thus not possible to match the complex PCL microgeometry with any tendon substitute.
TABLE 21-11 Structural Properties of the Intact Anterior Cruciate Ligament, Intact Posterior Cruciate Ligament, and Various Graft Constructs
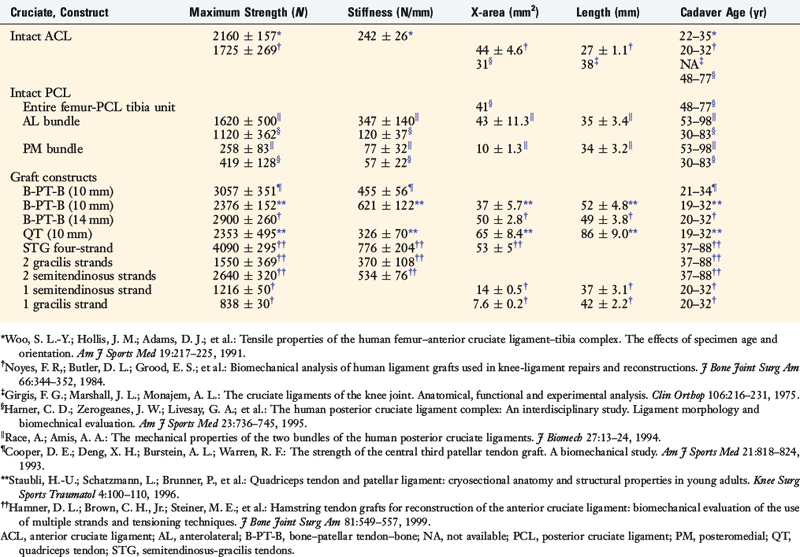
The cadaver age in the investigation by Race and Amis124 ranges from 53 to 98 years. Previous investigations by the senior author and Grood108 and others161 documented significant reductions in strength and stiffness properties of ligament units with advancing age. For instance, one study documented that whereas ultimate failure of ACL-bone grafts occurred at a mean of 1730 N in young cadavers (aged 16–26 yr), this value decreased to a mean of 734 N in older cadavers (aged 48–86 yr).108 Race and Amis124 estimated that a PCL reconstruction should be designed to match a native PCL with a strength of 4000 N, and not the approximate 2000 N shown in Table 21-11 (for both bundles combined).
In a study of 14 cadaveric PCL specimens (mean age 52 yr; range, 30–83 yr), Harner and associates58 reported a mean ultimate load to failure of the anterolateral PCL bundle of approximately 1200 N and of the posteromedial bundle of 400 N. This provides an ultimate failure load of the entire PCL in the 1600- to 1700-N range, well below that expected, which is most likely due to the advanced age of the cadaver specimens.
In a similar manner, large variations may exist in reported strength and stiffness data based on the testing apparatus and manner in which soft tissues are grasped without inducing premature failure. For example, the strength of the quadriceps tendon construct shown in Table 21-11 is 2353 N; however, the mean cross-sectional area is 65 mm2. Different methods that affect these values are used to measure cross-sectional area. The senior author and coworkers106 previously described a method that induced a low level of compressive force to compress the soft tissues into a block of defined dimensions that provided an accurate cross-sectional measurement. The data shown in Table 21-11 are derived from investigations that used different area measurement systems, making comparisons difficult.
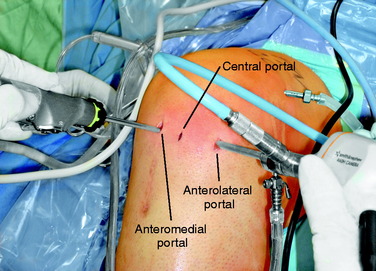
The principles for the selection of all-inside and tibial inlay grafts are summarized in Tables 21-12 and 21-13.
TABLE 21-12 All-Inside Posterior Cruciate Ligament Graft Options
| Two-Strand Grafts | Single-Strand Grafts |
|---|---|
| Preferred | Preferred |
| QT-PB autograft |
AT-B, Achilles tendon–bone; B-PT-B; bone–patellar tendon–bone; PCL, posterior cruciate ligament; QT-PB, quadriceps tendon–patellar bone.
TABLE 21-13 Tibial Inlay Posterior Cruciate Ligament Graft Options
| Two-Strand Grafts* | Single-Strand Grafts†‡ |
|---|---|
| Preferred | Preferred |
| QT-PB autograft | QT-PB autograft |
| Alternative | Alternative |
| B-PT-B allograft | B-PT-B allograft |
| QT-PB allograft | QT-PB allograft |
| AT-B allograft | AT-B allograft |
| Principles | Principles |
AT-B, Achilles tendon–bone; B-PT-B; bone–patellar tendon–bone; PCL, posterior cruciate ligament; QT-PB, quadriceps tendon–patellar bone.
* Single tibial inlay bone block, two separate femoral tunnels at 1 o’clock and 4 o’clock to maintain bone bridge between tunnels, preferred over single tunnel.
† Single tibial inlay bone block, one femoral tunnel 1 o’clock position.
‡ Preference for two-strand graft when added complexity of the tibial inlay approach is used, single strand provided for completeness.
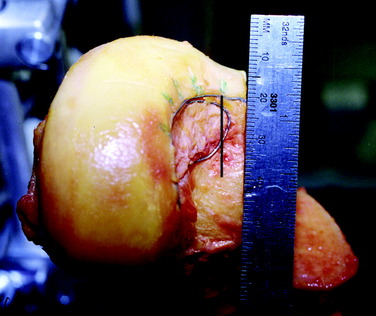
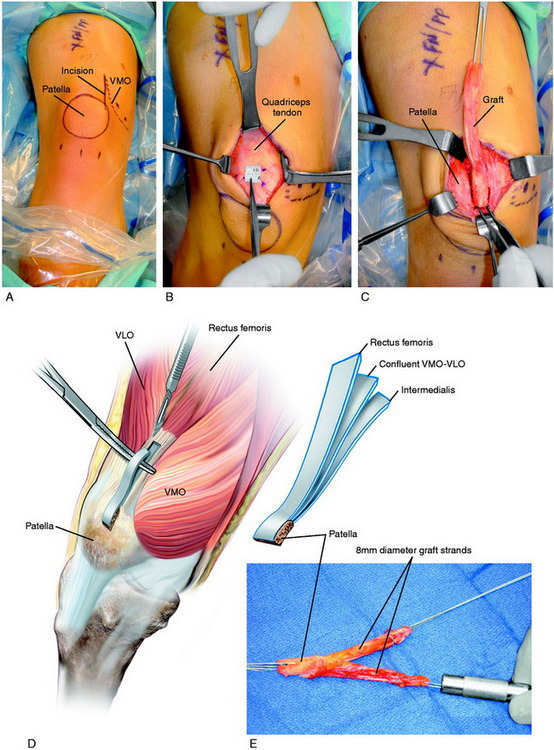
Preparation of QT-PB Autograft
A tourniquet is inflated to 275 mm of pressure. This is usually the only time the tourniquet is used in the reconstructive procedure, except when the open tibial inlay approach is selected. An incision is made just medial to the superior pole of the patella and extended proximally 5 to 6 cm (Fig. 21-15). The incision also allows access to the anteromedial aspect of the medial femoral condyle and vastus medialis obliquus (VMO) for subvastus placement of the femoral tunnels. A cosmetic approach is used with subcutaneous dissection performed circumferentially about the incision to allow the skin to be mobilized superiorly and inferiorly for the graft harvest. With this technique, no incision is required over the patella.
Critical Points PREPARATION OF QUADRICEPS TENDON–PATELLAR BONE AUTOGRAFT
Surgical Technique for Anteromedial Approach and Outside-In Femoral Tunnels
Critical Points PREPARATION OF ACHILLES TENDON–BONE ALLOGRAFT
Critical Points SURGICAL TECHNIQUE FOR ANTEROMEDIAL APPROACH AND OUTSIDE-IN FEMORAL TUNNELS
PCL, posterior cruciate ligament; VMO, vastus medialis obliquus.
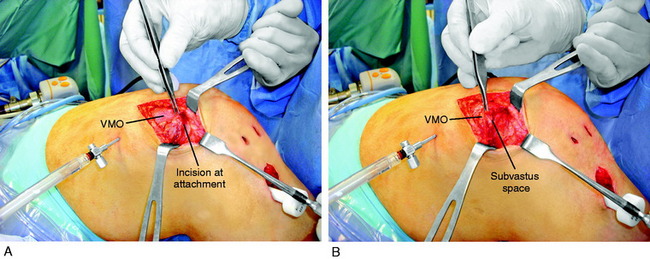
A vertical skin incision of 3 to 4 cm is made over the anteromedial vastus medialis proximal to the knee joint and just medial to the quadriceps tendon. When an ipsilateral QT-PB is harvested, the same skin incision is used (Fig. 21-16).
PCL All-Inside Technique: One- and Two-Strand Graft Reconstructions
The authors’ graft preference for an all-inside technique is a QT-PB autograft for isolated PCL reconstruction. The preference for multiligament reconstructions is a B-PT-B allograft for the PCL procedure, using two femoral tunnels and a single tibial tunnel. The bone plug is placed and fixated in a posterior tibial tunnel or socket directly at the posterior entrance under fluoroscopic control (see Table 21-13). The goal is to match the results of the tibial inlay procedure, with the bone plug placed directly at the posterior PCL attachment using an oblique tunnel instead of a tibial inlay that requires an open posteromedial approach. The operative steps for these techniques are described in the following sections. The different PCL procedures and potential options for tibial and femoral placement and tunnels, based on the graft selected, are summarized in Table 21-14.
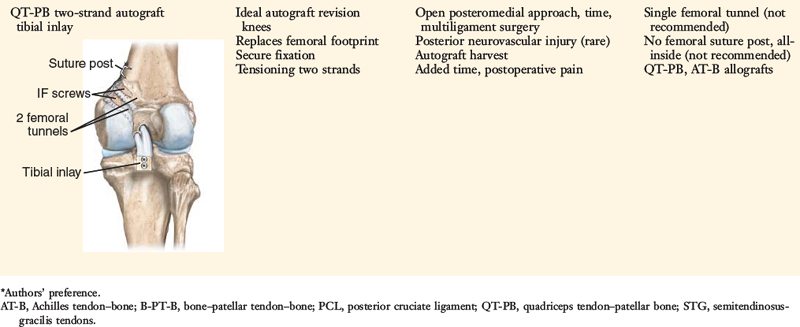
Patient Positioning and Setup
An examination under anesthesia is performed to confirm the diagnosis and carefully compare the injured knee with the opposite normal knee, as already described. It is important to palpate the medial tibiofemoral step-off at 90° of flexion in both knees. At surgery, the PCL grafts will be tensioned in knee flexion and the medial tibiofemoral step-off used as verification that the abnormal posterior translation has been corrected. In multiligament operative procedures, the patient is in a supine position with appropriate padding under all extremities with an Alverado foot and leg holder or similar device used to flex the knee joint to 60° to 70° (Fig. 21-17). This allows the lower limb to be secured and positioned throughout the operative procedures. After appropriate cruciate ligament surgery, any associated medial or lateral ligament procedure is performed with the knee flexion angle adjusted as necessary.
Critical Points POSTERIOR CRUCIATE LIGAMENT ALL-INSIDE TECHNIQUE: PATIENT POSITIONING AND SETUP
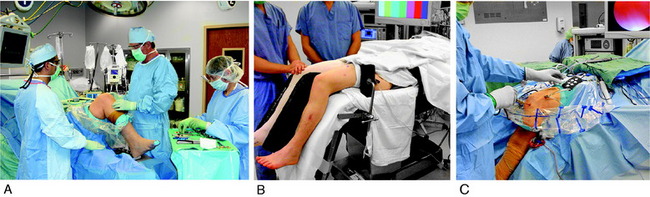
Routine arthroscopic anteromedial, anterolateral, and superolateral portals are created (Fig. 21-18). During the PCL reconstruction, a transpatellar central portal is required. The posteromedial portal to débride the PCL tibial fibers is not required and avoids inadvertent fluid extravasation into the popliteal fossa that would limit posterior capsule distention and posterior joint arthroscopic visualization.
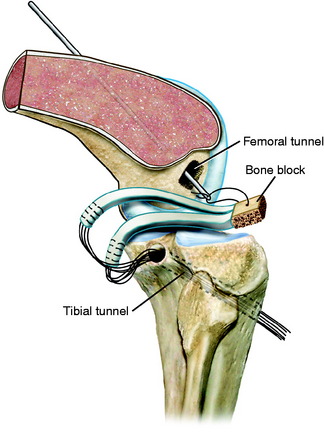
Tibial Tunnel Preparation
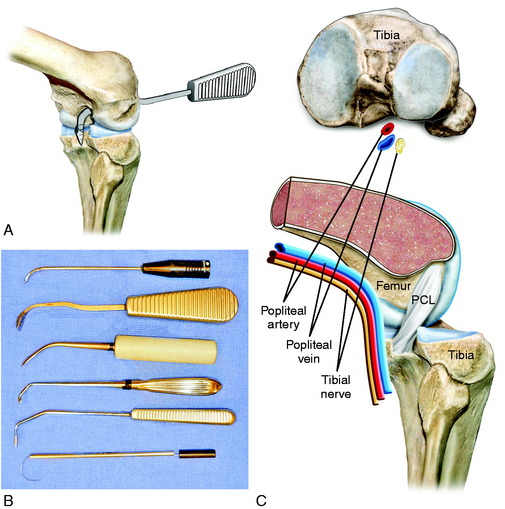
The knee is positioned at 60° of flexion as described to prevent pressure against the popliteal structures posteriorly. This allows the posterior neurovascular structures to drop away from the posterior aspect of the knee. Matava and associates83 reported that the mean distance of the PCL from the popliteal artery from 0° to 100° of flexion was 7.6 mm in the axial plane and 7.2 mm in the sagittal plane; however, individual variation may exist between knees. During the operative procedure, the surgeon is constantly aware of the joint pressure, fluid inflow and outflow, increased thigh tension, and any lack of joint distention. Intermittent palpation of the popliteal and calf region is performed during the operative procedure to detect fluid extravasation by an inadvertent puncture of the posterior capsule.111
Critical Points POSTERIOR CRUCIATE LIGAMENT ALL-INSIDE TECHNIQUE: TIBIAL TUNNEL PREPARATION
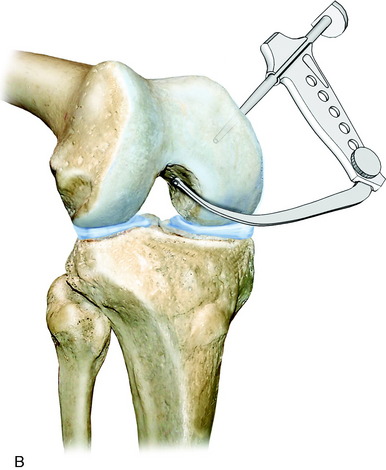
A critical step is the passage of a curved Cobb elevator or commercially available Acufex (Smith and Nephew Endoscopy, Andover, MA) PCL Elevator (Fig. 21-19), which has a 90° curve and is used to gently free up the space in front of and behind the remaining PCL fibers. In some knees, the posterior capsule becomes adherent to the PCL fibers. The PCL Elevator is used to gently tease the capsule off of the PCL fibers and avoid rupture of the posterior capsule. This step requires a gentle approach to push the posterior capsule distally to the level of the distal PCL and capsule attachments, which are at the level of the posterior tibial step-off.
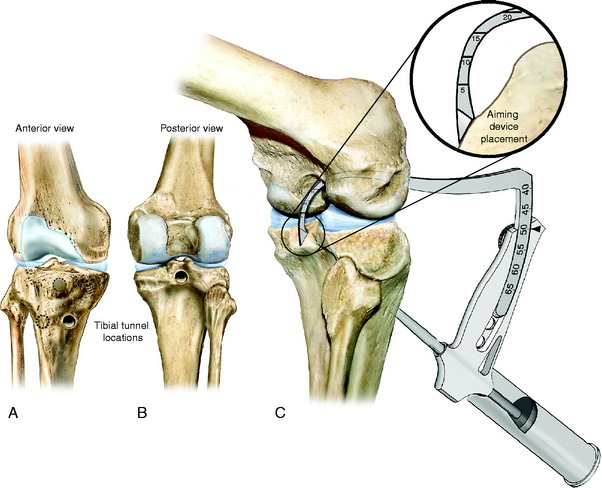
Drilling of the Tibial Tunnel
A medial skin incision 3 to 4 cm is made 1 cm medial to the tibial tubercle. The tunnel entrance is medial or lateral to the tibial tubercle (Fig. 21-20). A theoretical advantage may exist for the tunnel to be started just lateral to the tibial tubercle to produce less posterior tunnel graft angulation. However, either tunnel location is acceptable. The senior author usually prefers an entrance medial to the tibial tubercle. When an ACL reconstruction is also performed with a medial tunnel, the PCL graft is placed through a tunnel lateral to the tibial tubercle.
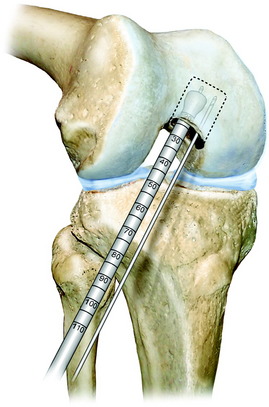
Critical Points POSTERIOR CRUCIATE LIGAMENT ALL-INSIDE TECHNIQUE: DRILLING OF TIBIAL TUNNEL
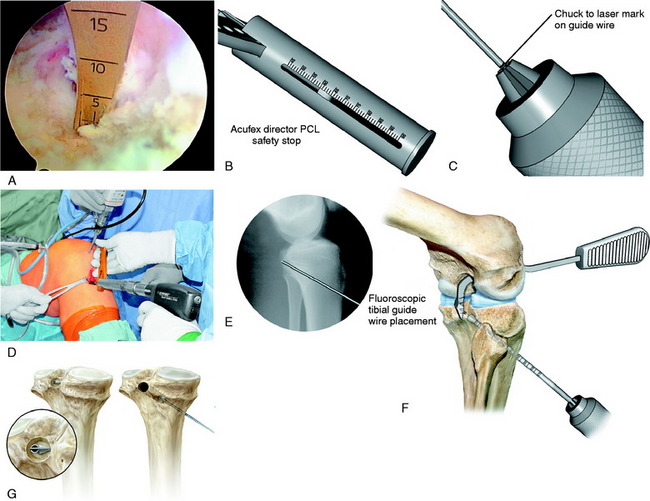
The drilling of the tibial tunnel is shown in Figure 21-21. The drill guide is placed through the transpatellar portal. The tip of the guide is placed at the desired position of the tunnel as far distal as possible, which is to the level of the posterior capsule insertion on the tibia just before the posterior tibial step-off. The distal placement of the guide pin is a critical step for success; an error is to place the guide pin too proximal in the PCL fossa, which produces a near-vertical PCL graft with limited ability to resist posterior tibial subluxation. The tip of the guide rests on the distal posterior capsule attachment with the guide pin target just 5 mm proximal to the tip. This prevents the drill from proceeding too far distally beyond the posterior tibial step-off where the drill tip would not be visualized and could penetrate neurovascular structures. The goal is to place the guide pin in the distal central portion of the PCL fossa, 20 to 25 mm from the proximal entrance of the PCL fossa. This leaves 15 mm of the posterior fossa to retain the posterior graft position and prevent a vertical PCL graft. This is a key step of the procedure. The drill guide is angled 50° to 55° to produce an oblique tibial tunnel that will decrease graft angulation effects.
When the flip-drill technique is selected, a 4-mm drill is initially used to establish the tibial tunnel. The flip-drill is then advanced under arthroscopic visualization to exit the posterior tibial tunnel. The drill is flipped and held against the posterior tibial cortex, and the tunnel is carefully drilled in a retrograde manner to the desired depth, which is determined by the measured length of the flip-drill (see Fig. 21-21). The PCL dilator remains in place posteriorly at all times to displace the posterior capsule away from the drilling procedure and prevent inadvertent capsule penetration.
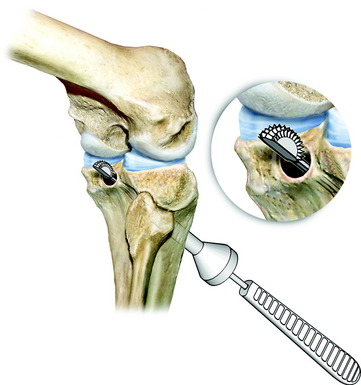
The proximal edge of the tibial tunnel is carefully chamfered with a rasp to limit graft abrasion effects (Fig. 21-22). Any remaining PCL fibers are removed so that the tibial tunnel entrance does not have soft tissue that would limit graft passage and to ensure the graft will lie flat against PCL tibial fossa. Again, it is necessary to have 15 mm of the posterior tibial fossa and an intact posterior intraspinous area proximal to the tunnel to maintain the normal angulation of the PCL tibial attachment to prevent a vertical PCL graft and to decrease graft tunnel enlargement (windshield-wiper effect). The most common technical mistake is to place the tibial tunnel at the proximal entrance of the PCL fossa, which is proximal to the native PCL tibial attachment.
PCL Femoral Graft Technique
An important aspect of a successful PCL reconstruction is to have a clear understanding of PCL anatomy and changes in fiber-length and tension with knee flexion, as already described. The anatomic rule of thirds to describe the PCL attachment assists the surgeon in defining the anterior-to-posterior plane and the proximal-to-distal plane of the native PCL (see Fig. 21-8A and B).
As described previously, the PCL attachment is elliptical in shape, extending from high in the notch over the lateral aspect of the distal medial condyle from an approximate 11:30 to 5 o’clock position (left knee). The PCL footprint follows the articular cartilage, with the anterior portion within 2 to 3 mm of its edge depending on the reference system used as previously discussed.87 At the 4 o’clock position, the PCL attachment is approximately 4 mm from the articular cartilage edge.129 However, if the aMFL is present, the footprint will appear to be 1 to 2 mm from the cartilage edge. There is anatomic variability in the normal proximal-to-distal width of the PCL, and in some knees, a more oval appearance exists owing to an increased width of the middle third of the PCL attachment. Because of anatomic variability in the PCL femoral attachment, it is necessary to map out the attachment using remaining PCL fibers to locate the desired graft position. The reference system axis used to describe the PCL attachment is distal-to-proximal and anterior-to-posterior with the knee in full extension. However, the surgeon views the PCL with the knee flexed and it is also helpful to communicate a graft position as “deep” or “shallow” and “high” or “low” in the femoral notch on the medial femoral condyle.
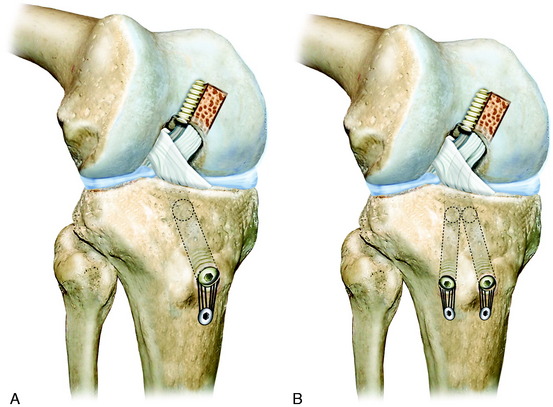
Technique for Femoral Placement of Two Tunnels and Graft Passage
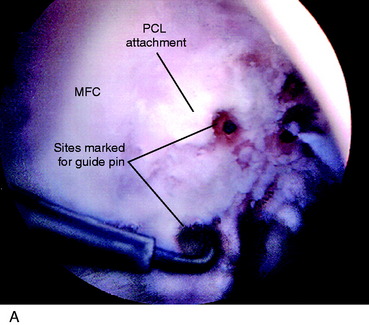
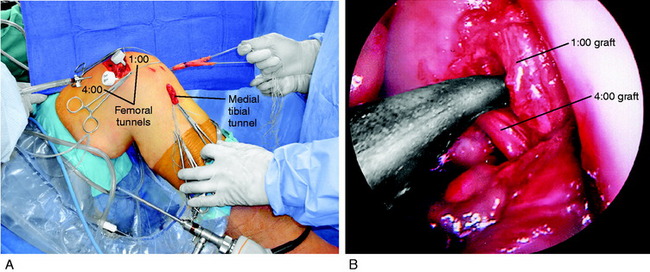
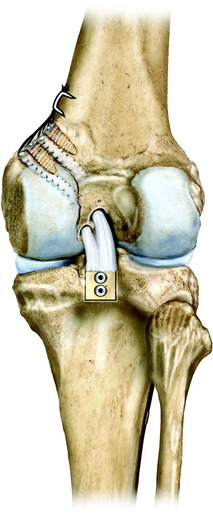
The technique for femoral placement of two tunnels and graft passage is shown in Figure 21-23. The PCL footprint is mapped with a calibrated probe and electrocoagulation. The 12 o’clock, 1 o’clock, and 4 o’clock position marks on the medial femoral condyle are made. The goal is to create two separate femoral tunnels in the distal two thirds of the native PCL attachment. This places a graft with an approximate 100 mm2 in cross-section, occupying up to 75% of the PCL attachment.
If the PCL graft is placed too distal or shallow in the notch, it will be subject to high tensile forces with knee flexion resulting in constraining flexion and probable graft failure. If the graft is placed too proximal or deep in the notch, the graft will slacken with knee flexion and allow posterior tibial subluxation. The correct placement within the PCL footprint is shown in Figure 21-23 where the graft replaces the distal two thirds of the PCL that functions in resisting posterior tibial subluxation with knee flexion.
PCL, posterior cruciate ligament; VMO, vastus medialis obliquus.
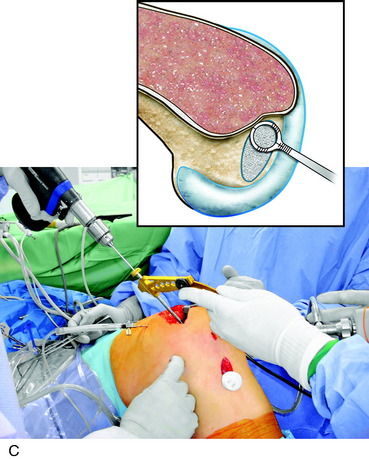
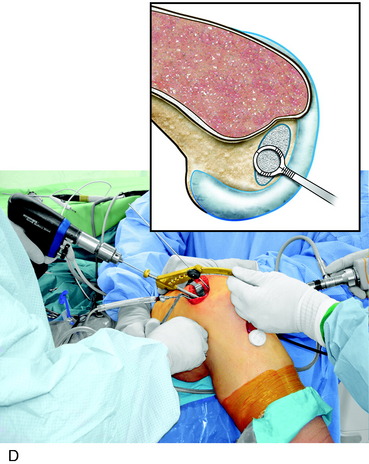
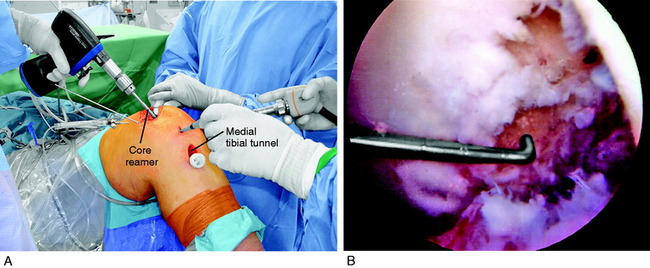
The two femoral tunnels are drilled using the outside-in (VMO-sparing approach) subvastus technique. As already described, the entrance of the 1 o’clock tunnel is 12 mm proximal to the femoral articular cartilage border and medial to the trochlea. The 4 o’clock tunnel entrance is also 12 mm proximal to the articular cartilage border and anterior to the femoral epicondyle. A core reamer is used for the 1 o’clock tunnel to obtain a bone graft for the patellar defect (QT-PB graft; Fig. 21-24). Careful chamfering of the tunnel edges is performed to decrease graft abrasion. A flexible ruler is passed through the tibial and femoral tunnels to measure the intra-articular length of the two graft strands.
The passage of the graft is performed in a stepwise fashion (Fig. 21-25). A 20-gauge wire is passed through the tibial tunnel and brought out the anterolateral portal, which is enlarged sufficiently to accept the PCL graft. A 22-gauge wire is passed through each of the two femoral tunnels and a grasper or nerve hook is used to bring the two wires out the same anterolateral portal. The 1 o’clock and 4 o’clock wires are marked.
Fluoroscopy is used to confirm final placement of the bone plug in the tibial tunnel (Fig. 21-26). The graft is marked at the collagenous fiber-bone junction and viewed arthroscopically to confirm that the bone plug is entirely within the tibial tunnel and placed directly at the posterior tibial tunnel entrance. The sutures are tied over a tibial suture post. An absorbable interference screw (1 mm less than the diameter of the tunnel) is used for bone plug fixation at the tibial tunnel, verified by fluoroscopy. The final tensioning of the graft at the femoral site is performed next. In the alternative flip-drill technique of drilling a posterior tibial socket, four high-strength sutures placed in the bone plug are tied over a suture post.

FIGURE 21-26 Fluoroscopy confirms that the patellar bone plug is directly at the posterior tibial tunnel exit.
Graft Tensioning and Fixation for All-Inside Grafts
The graft tensioning and fixation steps are the same for all grafts. For grafts with the bone block in the tibial tunnel, initial fixation is performed at the tibia (as already described) and final tensioning and fixation are performed at the femoral site. For bone blocks placed at the femoral site, fixation is first performed at the femoral site and final tensioning and fixation performed at the tibial site (Fig. 21-27).
The graft is longest at high knee flexion angles, which is the position selected for graft fixation. In most knees, the 70° flexion angle has the same graft length behavior as 90° and this position is selected. Commercial graft-tensioning devices42 are available (as used in ACL reconstructions) that provide measurable length-tension data and may be used for measurement of graft-tensioning loads. The sutures for each graft stand are tied over a femoral or tibial post, maintaining the 10 pounds of graft load and 10 pounds of anterior tibial load.
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
Alternative PCL All-Inside Techniques
Femoral Placement of Rectangular (Oval) Tunnel for Bone Plug
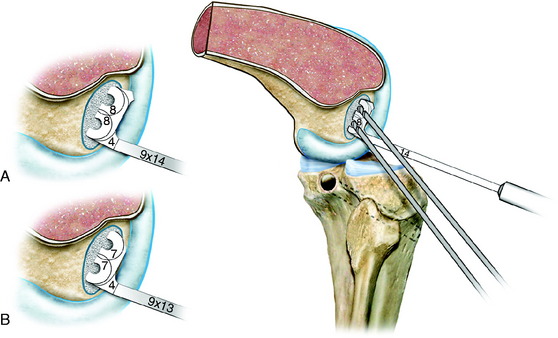
The goal is to create an 8- × 12-mm rectangular slot that extends from 1 o’clock to 4 o’clock in the distal two thirds of the PCL footprint. The 12 o’clock and 4 o’clock marks are made on the medial femoral condyle. Again, the guide pin mark is 6 and 8 mm from the articular cartilage of the medial femoral condyle for the anterior and posterior tunnels (Fig. 21-28), verified by observing the PCL footprint and that the two tunnels are in the distal two thirds of the footprint. Use a small curet or awl to penetrate and define the pilot hole for each tunnel. A 2.4-mm guide pin is placed through the anterolateral portal into the anterior tunnel location, the knee flexed to 90°, and the guide pin advanced through the medial femoral condyle approximately 25 mm in depth based on the patellar bone length.
The second guide pin is placed into the second marked position. The guide pins are over-reamed with an endoscopic drill (Fig. 21-29) to form an oblong tunnel entrance to a depth corresponding to the graft bone. Care is taken to avoid the lateral femoral condyle articular cartilage as the drill is introduced into the knee joint. The remaining central bone bridge is removed with a curet or bur.
The PCL Dilator (Fig. 21-30) dilates the attachment into an oval 9- × 13-mm shape that is approximately 1 mm larger than the bone portion of the graft. Care is taken at this point to use low forces in dilating the rectangular slot to avoid fracture of the femoral condyle. In the authors’ experience, this has not been reported; however, it is worth a cautionary note. The PCL Dilator has a graft-sizing slot on the handle for a 9- × 13-mm bone block to assist in preparation of the graft.
The passage of the graft begins with the passage of a 22-gauge wire through the tibial tunnel, which is grasped with a nerve hook and brought out through the anterolateral portal (Fig. 21-31). The tendon graft strands are passed through the enlarged anterolateral portal, which is increased 2 to 3 cm in length to prevent soft tissues from impeding graft passage. When a two-tunnel tibial technique is used, two wires are passed and the graft strands marked for the 1 o’clock graft to the lateral tunnel and the second 4 o’clock graft to the medial tibial tunnel. A towel clip or suture is used to close the anterolateral portal after graft passage to maintain joint distention.
A guide pin (with an end to carry the sutures) is passed through the anterolateral portal into the rectangular femoral slot to exit anterior and proximal to the medial femoral epicondyle. The bone block with sutures is passed into the knee joint. The arthroscope views the bone block and the orientation is controlled with the cancellous surface oriented proximal (deep) in the rectangular slot. The bone block is positioned flush (not recessed) at the femoral attachment. Fixation is performed with an interference screw passed through the anterolateral portal with the knee flexed to 110° (Fig. 21-32). The interference screw is placed anterior to the bone block and snugly secures the graft.
Two Separate Femoral and Tibial Tunnels and Two Separate Grafts
 Graft passage same order except femoral portion of graft advanced through anterolateral portal by guide pin-–suture carrier placed through the respective femoral tunnel.
Graft passage same order except femoral portion of graft advanced through anterolateral portal by guide pin-–suture carrier placed through the respective femoral tunnel.PCL Arthroscopic-Assisted Open Tibial Inlay Technique
Patient Positioning and Setup
The patient is placed in a supine position on an inflatable beanbag (Fig. 21-33). The distal end of the beanbag is placed at the gluteal crease so it does not interfere with the tourniquet and the external rotation of the lower limb during the posteromedial tibial inlay approach. The beanbag is inflated and contoured to the patient’s thorax and pelvis. A safety belt and kidney rest are placed to further secure the patient to the operating table when it is externally rotated (operative side down) during the posteromedial approach. A thigh tourniquet is placed over cast padding and used only intermittently for short periods during graft harvest and the posteromedial approach. The table is reflexed at its midpoint to decrease spine hyperextension, produce mild hip flexion, and prevent tension on the femoral nerve from a hip hyperextension position. The opposite extremity is placed in a thigh-high compression hose and posterior padded leg support to avoid hip hyperextension or abnormal pressures on the posterior thigh during the operative procedure.
The autograft harvest procedure or preparation of the allograft is completed as described.
Identification of the Femoral PCL Attachment: VMO Approach
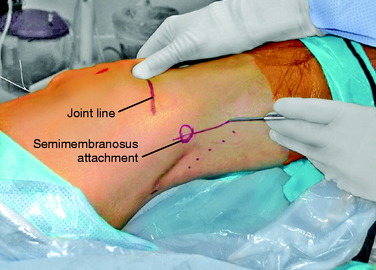
Posteromedial Approach91,102,110
Numerous surgical approaches that provide access to the popliteal fossa PCL tibial attachment have been described.1,8,9,15,86,89,152 These approaches use an S-shaped popliteal incision,8 an L-shaped popliteal incision,15,89 or a medial incision.71,90 The senior author recommends a medial incision as described to avoid the popliteal neurovascular structures.
A 7- to 8-cm longitudinal incision, beginning approximately 2 cm proximal to the flexion crease of the knee, is carried distally over the medial head of the gastrocnemius and the posterior border of the semitendinosus tendon (Fig. 21-34). The straight posteromedial incision, compared with an S-popliteal incision, avoids the horizontal popliteal skin crease with less skin retraction necessary and possible wound breakdown.89
PCL, posterior cruciate ligament; VMO, vastus medialis obliquus.
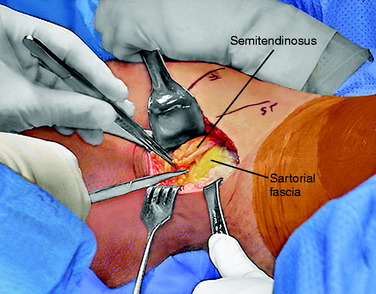
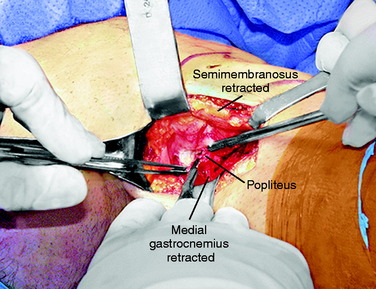
The first key to the approach is to incise the fascia157 along the posterior border of semitendinosus tendon adjacent to the medial border of the gastrocnemius muscle. The three pes tendons are then retracted anteriorly (taking the saphenous nerve) and the semimembranosus tendon is visualized (Fig. 21-35).
The second key to the procedure is the dissection between the semimembranosus muscle and the gastrocnemius tendon. Understanding the anatomy of the posteromedial corner of the knee and the semimembranosus is important to obtain good exposure by mobilization of the semimembranosus tendon for the next portion of the dissection. The dissection uses the interval between the medial border of the gastrocnemius and the posterior border of the common semimembranosus tendon. In order to mobilize the semimembranosus medially and improve exposure, the tendon sheath extensions are incised to allow full mobilization of the semimembranosus tendon (Fig. 21-36). Anterior to the semimembranosus, the posterior oblique ligament is partially incised from the attachment to the semimembranosus tendon to improve exposure. These capsular attachments are later repaired at the end of the procedure. With lateral retraction of the medial gastrocnemius, the inferolateral semimembranosus tendon sheath expansion to the popliteus is visualized and dissected from its attachment to the posterior border of the common semimembranosus tendon. In this way, the insertion of tendon directly onto the posteromedial tibia is exposed.
The neurovascular structures are not visualized and remain medial to the gastrocnemius muscle (medial head). The anterior tibial artery may lie directly on the popliteal muscle over the PCL fossa or pierce the popliteal muscle just distal to the PCL fossa as already described (see Fig. 21-9).
Identification of Posterior Tibial PCL Attachment for Inlay Procedure
The PCL tibial attachment site is palpated as a midline depression in the proximal tibial metaphysis, between the two tibial condyles. The width of the PCL is approximately 15 mm51 and the distal extent of the PCL is marked by a small ridge (posterior tibial step-off) that coincides with the proximal border of the popliteus.123
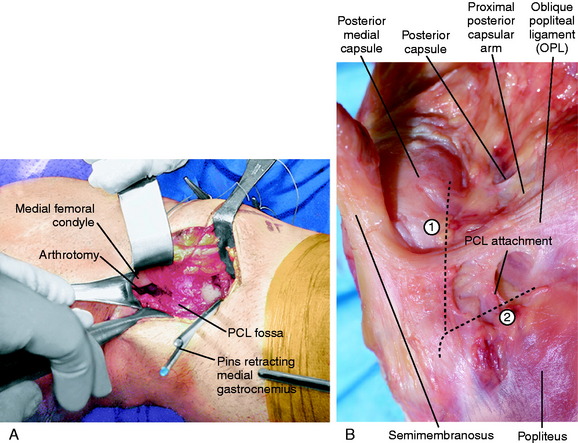
The fifth key to the exposure is to enter the joint proximal and just behind the semimembranosus tendon, avoiding the medial meniscus attachments. The posterior slope of the proximal tibia and the PCL fossa are palpated and the posterior capsule and OPL incised sharply, starting proximal and superior on the lateral aspect of the medial femoral condyle. The posterior portion of the medial femoral condyle is easily palpated. The posterior capsule just lateral to the medial femoral condyle is incised. The joint is entered directly over the inner aspect of the medial femoral condyle to establish from proximal-to-distal a safe plane of dissection (Fig. 21-37; see also Fig. 21-36). The dissection of the capsule is performed in the midline directly over the PCL fossa with care at the joint line to avoid injury to the posterior medial meniscus tibial attachment. This capsular incision is extended distally and connected to the popliteus subperiosteal exposure, which will be closed at the conclusion of the procedure. The entire PCL tibial attachment site is easily identified. The remaining PCL stump is removed.
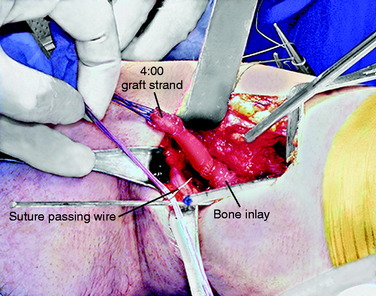
The eighth key is the placement and adjustment of the position of the PCL graft. The previously positioned guidewires are retrieved from the posteromedial capsular recess within the joint. The two strands of the sagittally split graft are identified (lateral arm, 1 o’clock tunnel; medial arm, 3 o’clock tunnel) and are passed individually starting with the 1 o’clock graft strand (Fig. 21-38). Care is taken that there is no soft tissue or native PCL fibers so the graft strands lie directly against the posterior tibia PCL fossa in a normal anatomic position.
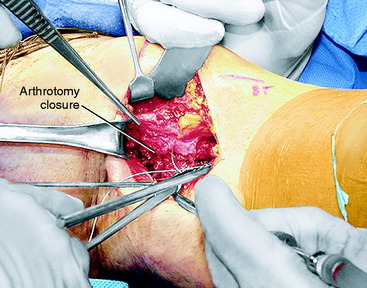
The capsulotomy is closed, the Steinmann pins removed, and the posteromedial capsule incision and oblique popliteal ligament repaired (Fig. 21-39). The tourniquet is deflated and hemostasis verified. Vascular clips are available should the inferior medial genicular artery or other bleeding sources be identified. The subcutaneous tissues and wound are not closed at this stage to allow for any extravasation of fluid during the final arthroscopic portion of the procedure. After graft fixation, the posteromedial wound is closed in a routine fashion.
Graft Conditioning, Tensioning, and Fixation
Arthroscopic visualization of the graft confirms proper placement of both strands prior to fixation. The graft tensioning and fixation steps have been previously described in detail in the “All-Inside Technique” section. A staple post is placed proximal to the femoral tunnels. Fixation is accomplished by tying each suture with approximately 10 pounds (44 N) on each graft strand, at 70° to 90° flexion, and 10 pounds (44 N) anterior tibial load to produce a normal medial tibiofemoral step-off, which is confirmed. A soft tissue absorbable interference screw is added for each tunnel (Fig. 21-40). Arthroscopic evaluation of the graft confirms tension, fixation, and return of stability.
Critical Points POSTERIOR CRUCIATE LIGAMENT AVULSION FRACTURES
PCL Avulsion Fractures
Avulsion fractures of the PCL are rare, and treatment options depend on the type and size of the fracture, displacement, comminution, and orientation of the fragment.52,88 These injuries typically occur at the tibial attachment and may encompass either a small area at the posterior region of the attachment or a large area that extends anteriorly and outside of the PCL attachment. Griffith and colleagues52 reported that the entire insertion area was avulsed in all 19 skeletally mature patients in their series of PCL avulsion fractures. The avulsion fracture is usually obvious on routine radiographs. Occasionally, a computed tomography scan is required to define the extent of the fracture pattern in major avulsion fractures extending into the joint.16,52 Clanton and coworkers25 reported on the importance of the diagnosis of ligament injuries in children and noted two PCL avulsions from the femur that underwent open operative reduction and fixation with sutures. Mayer and Micheli85 reported on one case of a PCL femoral attachment avulsion associated with posterolateral instability due to a hyperextension injury mechanism. These authors reported that avulsion or peel-off PCL injuries at the femoral site were rare in the literature.
Patients who have small, partial PCL avulsion fractures, with a negative posterior translation test at 90° knee flexion, are kept in a brace locked in full extension and remain partial weight-bearing for 4 weeks to allow healing. The brace is removed for gentle range of motion (avoiding posterior tibial translation) and quadriceps exercises as described in Chapter 23, Rehabilitation of Posterior Cruciate Ligament and Posterolateral Reconstructive Procedures. Overall, the prognosis for healing and PCL function is good to excellent in these cases.163
Complete avulsion of the PCL attachment at the tibia and, less frequently, at the femoral attachment121,127 (peel-off avulsion) with posterior tibial subluxation, is an indication for surgical repair. Numerous authors have reported favorable clinical results with the open reduction and internal fixation of PCL avulsion fractures at the tibial insertion site.62,88,150 Inoue and associates62 reported on 31 patients followed for 2 to 8 years with good results and low side-to-side differences (<5 mm, KT-2000) after surgery. The authors reported that the majority of knees showed mild residual posterior knee displacement (mean, 3.0 mm). Along with the tibial avulsion, an abnormal MRI signal intensity may be observed within the PCL fibers, indicating partial tearing.
A number of arthroscopic techniques have been reported for PCL tibial avulsion injuries.16,32,69,139 Kim and colleagues69 reported the outcome of 14 knees with an avulsion fracture of the PCL at the tibial attachment. The arthroscope was placed through the posteromedial portal and a plastic sheath with waterproof diaphragm passed through the posterolateral portal. The anteromedial portal was used as required. A large bone fragment was fixed by one or two transtibial cannulated screws placed from the anterior tibia after the bony fragment had been reduced and held by pins. Small bony fragments were fixed with multiple sutures through single or double tibial tunnels. The postoperative program involved a long-leg hinged brace locked at full extension for 3 weeks. Range of knee motion was then initiated with the brace locked in full extension for walking. The brace was removed at 8 weeks. The authors reported all avulsion fractures healed. The 12 knees that underwent operative reduction and fixation operation in the acute phase showed only a trace posterior instability with stress radiographs measuring between 1.2 to 3.5 mm of residual posterior displacement at 90° knee flexion. In 2 patients who had delayed surgery, the residual displacement was 3.3 and 4.1 mm.
Shino and coworkers139 reported on six knees that had arthroscopic fixation of a PCL tibial bone avulsion. Fixation was achieved with a single cannulated screw or by suture fixation with comminuted injuries. A pull-out button was introduced through the posteromedial portal and the sutures passed through two tibial drill holes and tied at the anterior aspect of the tibia.
In Kim and colleagues’ study,69 postoperative arthrofibrosis developed in 3 of 14 knees, which compromised the final result. The authors concluded that PCL avulsion fractures are amendable for fixation by arthroscopic methods. They speculated that an early range of motion program might be beneficial to prevent arthrofibrosis.
The concept of immediate motion is addressed in detail in Chapter 23, Rehabilitation of Posterior Cruciate Ligament and Posterolateral Reconstructive Procedures. The therapist initiates early and protected knee motion within the 1st postoperative week, applying an anteriorly directed load to protect the relatively weak suture fixation. The use of a posterior calf pad and careful positioning in the brace is required for the first 4 postoperative weeks until suitable healing has occurred. Knees with suture or pin fixation have relatively low tensile strength repairs and require expert postoperative rehabilitation.
A peel-off type of PCL rupture from the femoral attachment has been described as a hyperextension knee injury, such as that reported by Mayer and Micheli85 in a child while jumping on a trampoline or in patients suffering from trauma from a motor vehicle accident.25,115 This type of PCL rupture directly at the femoral attachment may occur at the fibrocartilagenous junction with minor associated damage to the bulk of the PCL fibers. The PCL attachment is easily repaired with sutures passed through small drill holes, avoiding the proximal physeal growth plate.
Ross and associates127 described an arthroscopic approach for repair of acute femoral peel-off tears. Three No. 2 nonabsorbable sutures are passed through the PCL substance, through a femoral tunnel at the PCL footprint, and tied over the medial cortex. Park and Kim115 reported an arthroscopic technique that used two transfemoral tunnels for the anterior strand and two posterior tunnels for suture repair of the posterior strand. These authors noted that femoral avulsion injuries were exceedingly rare.
PCL Augmentation Approaches and Techniques
Sutures are used to repair the more distal fibers to the femoral attachment as already described. The placement of a 7-mm tibial tunnel must be well chosen and not interfere with the PCL attachment site. The tunnel is placed just medial to the tibial PCL attachment, carefully avoiding the medial and lateral meniscus attachments. A lateral tibial tunnel is not used because PCL fibers attach in part to the posterolateral meniscus tibial attachment. The authors agree with Wang and colleagues156 and prefer a three- or four-strand semitendinosus-gracilis (STG) autogenous graft, although an allograft may also be considered.3,63 Suture fixation to a femoral or tibial post and an absorbable interference tibial and femoral screw in adults is required.
Critical Points POSTERIOR CRUCIATE LIGAMENT AUGMENTATION APPROACHES AND TECHNIQUES
MRI, magnetic resonance imaging; PCL, posterior cruciate ligament.