110
Porphyria cutanea tarda

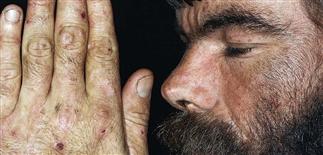
Blisters occur in sun-exposed areas such as the face and neck and the dorsa of the hands and forearms.
Clinical features: blistering in sun-exposed areas, facial hypertrichosis, hyperpigmentation, and sclerodermoid changes.

The classic representation, with erosions, vesicles, and bullae localized to the backs of hands.

Blisters formed on a non-inflamed base following sun exposure. The blisters have healed with the formation of milia.
DESCRIPTION
Most common form of porphyria, disorders of heme synthesis resulting from deficiency of hepatic uroporphyrinogen decarboxylase activity.
HISTORY
• Porphyrias represent abnormalities in heme synthesis pathway. Enzyme deficiencies result in increased formation of metabolic intermediaries (porphyrinogens) just before specific enzyme defect. Each porphyria characterized by specific enzyme deficiency, has distinct clinical characteristics. • Porphyrias divided into disorders of bone marrow heme synthesis (erythropoietic porphyrias), disorders of hepatic heme synthesis (hepatic porphyrias). Acquired and familial forms exist. • Porphyria cutanea tarda occurs when heme biosynthetic pathway is compromised by exogenous agent. Acquired ‘sporadic’ form occurs as complication of hepatic dysfunction or is induced by alcohol, drugs, hormones. • Estimated prevalence: 1 in 25 000 in North America. • Alcohol and estrogens associated with more than 80% of cases. Porphyria cutanea tarda from alcohol abuse tends to be chronic and relapsing until alcohol dependence addressed. • Autosomal dominant transmission in familial porphyria cutanea tarda.
PHYSICAL FINDINGS
• Erythema, edema, vesicles occur in sun-exposed areas such as face, neck, dorsa of hands, forearms. Blisters rupture, leaving erosions and ulcers that heal with scarring. Milia form in previously blistered sites. • Chronic changes include facial hypertrichosis, hyperpigmentation, skin fragility. Sclerotic changes develop on face, neck, hands. • Skin biopsy confirms subepidermal split and thickening of superficial dermal vascular endothelium. • Direct immunofluorescence shows deposition of IgG, IgM, and complement C3 surrounding blood vessels in papillary dermis. • Fecal analysis shows elevated coproporphyrins. • A 24-h urine collection contains uroporphyrin in a ratio of about 4 : 1 to the coproporphyrin fraction. Urine may have red-brown discoloration, so-called port-wine urine, from high levels of porphyrin pigments; may show bright-pink fluorescence under a Wood’s light. • Pseudo-porphyria usually due to non-steroidal anti-inflammatory drugs and is clinically indistinguishable from porphyria cutanea tarda. Porphyrin studies are negative.
TREATMENT
• Complete elimination of alcohol and other hepatotoxins can result in skin clearing in 2 months to 2 years. • Iron removal by phlebotomy is treatment of choice. One unit of blood should be removed every 2–4 weeks until the hemoglobin drops to 10 g/dL or until serum iron drops to 50 mg/dL. • Chloroquine in very low dosages causes release of hepatic tissue-bound uroporphyrin; subsequently, it is rapidly eliminated by the plasma and excreted in urine. • Measuring plasma uroporphyrin is effective way to monitor progress of patients. Treatment should continue until plasma uroporphyrin drops below 10 mmol/L • Sunscreens containing Parsol or physical sun blockers containing titanium dioxide or zinc oxide are moderately effective.







