CHAPTER 30 Popliteal block
Clinical anatomy
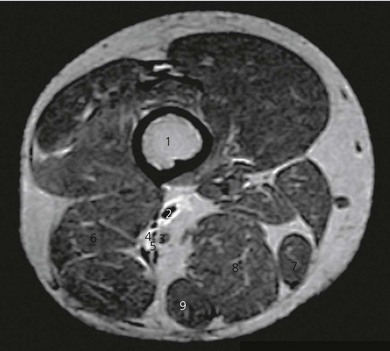
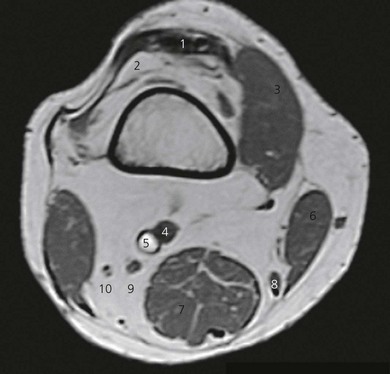
The popliteal fossa is defined as the space between the skin, the femur anteriorly and the biceps femoris muscle laterally, the semitendinosus and semimembranosus muscles medially, and inferiorly by both heads of the gastrocnemius (Figs 30.1 and 30.2). The space is mostly filled with fat and contains in its anterolateral aspect the popliteal vessels and nerves. The sciatic nerve is formed from roots L4 to S2 (and occasionally S3) and consists of two distinct divisions – the tibial and common peroneal nerves – which share a common epineural sheath from their origin to the popliteal fossa. The two nerves innervate the entire leg below the knee except for the anteromedial leg and foot, which are innervated by the saphenous nerve (L2, 3, 4).
The sciatic nerve branches in the region of the distal thigh (Fig. 30.3), anywhere between 4 and 13 cm above the popliteal crease, although occasionally they can run as two separate nerves from the sciatic foramen. The tibial nerve is the larger of the two branches and runs parallel and slightly lateral to the midline. Inferiorly, it passes between the heads of the gastrocnemius muscle. The common peroneal nerve runs laterally along the medial aspect of the biceps femoris muscle. After bifurcation, the tibial nerve immediately gives off the sural nerve, which innervates the lateral aspect of the foot. The common peroneal nerve also gives off a sural communicating nerve (Fig. 30.4), and once it is below the head of the fibula it divides into superficial and deep peroneal nerves. The nerves lie more superficial and lateral to the popliteal vessels in the popliteal fossa and about midway between the skin and the posterior aspect of the femur.
Surface anatomy
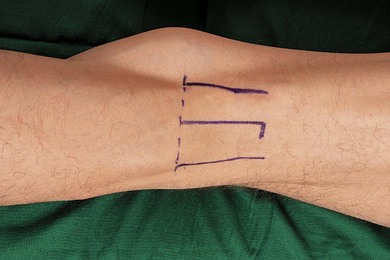
The main landmarks for the lateral popliteal block include the superior aspect of the patella and a muscular groove between the biceps femoris and vastus lateralis muscles (Fig. 30.5). Identification of this groove is difficult in obese patients and should be mastered prior to procedure. This is easily felt when patients flex their leg against resistance.
The main landmarks for the posterior popliteal block include skin crease of the knee joint and biceps femoris muscle laterally, and semimembranosus muscle medially (Fig. 30.6). The patient can be asked to flex the leg to identify the margins of the popliteal fossa. Absence of bony landmarks with the posterior approach increases the learning curve with this approach.
Sononatomy
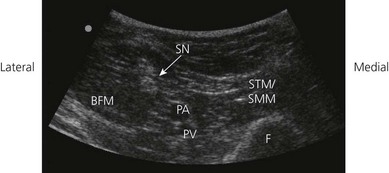
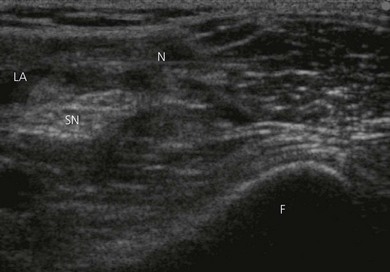
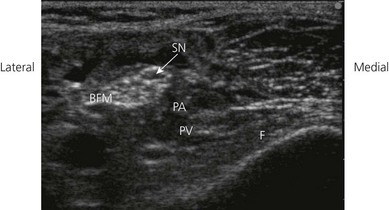
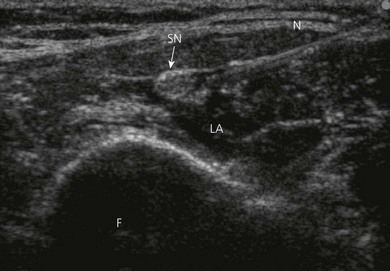
Using a transverse transducer orientation, perform a systematic anatomical survey of structures from superficial (skin) to deep and from medial to lateral in the popliteal fossa (Fig. 30.7). First identify the femur, which is deep and casts a bony shadow. Next, identify the pulsatile popliteal artery that is superficial to the femur (Fig. 30.8). If it is not visible, scan distally towards the popliteal crease where the popliteal artery is more superficial. The popliteal vein may or may not be visible (collapsed by transducer pressure). Note the muscle groups medially (semitendinosus and semimembranosus muscles) and laterally (biceps femoris muscle; Fig. 30.8). The hyperechoic sciatic nerve in this location is always superficial to the femur and lateral to the popliteal artery (Fig. 30.8). If the sciatic nerve is not easily visible, angle the transducer and aim the beam caudally towards the foot (Fig. 30.9). This will bring the nerve into view once the angle of incidence is approximately 90° to the nerve. Scan the region proximally and distally to assess nerve anatomy. Position the transducer in a location where the sciatic nerve is clearly visualized as a single nerve before its bifurcation. Nerve visualization is significantly improved once local anesthetic is injected, due to enhanced contrast between the hyperechoic nerve and the hypoechoic fluid collection.

Figure 30.7 The ultrasound transducer is positioned in the popliteal fossa with a transverse orientation.
Technique
Landmark-based approach
Lateral approach
The patient is placed supine, with the lower limb in the neutral position. The feet should be extended beyond the edge of the table in order to better discern the response to nerve stimulation (Fig. 30.10). A small sandbag underneath the knee or a pillow under the thigh facilitates the technique. The upper border of the patella is identified and a line is drawn vertically downward to the patient trolley. The groove between the lateral border of vastus lateralis and the biceps femoris tendon is identified. The intersection of the two lines is the needle insertion point.
Having outlined landmarks, the needle insertion point is infiltrated with local anesthetic using a 25-G needle. A 50–100-mm 21-G insulated needle is inserted at 30° to the horizontal plane, ensuring that the needle is directed away from the popliteal vessels (Fig. 30.11). The stimulating current is set at 1.0 mA, 2 Hz, and 0.1 ms. The needle is advanced slowly until the appropriate muscle response is obtained. The needle position is adjusted while decreasing the current to 0.35 mA with maintenance of the muscle response.
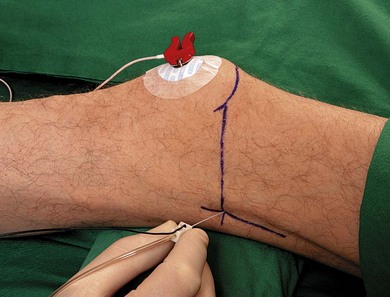
Figure 30.11 Lateral popliteal block technique. The needle is inserted at 30° to the horizontal plane.
The common peroneal nerve is usually found first because it is located more laterally (Fig. 30.12). After the first nerve is stimulated, at less than 0.5 mA, 10 mL of local anesthetic is injected slowly after careful aspiration. Then the amplitude of the nerve stimulator is increased to 2 mA and the needle is advanced slightly. The tibial nerve is located approximately 1–3 cm more medially, and a further 10 mL of local anesthetic is injected. With prior injection of local anesthetic, the second nerve should be found in a short time if possible, because there is a theoretical risk of nerve damage when the surrounding area becomes anesthetized.
Posterior approach
The patient is placed in the prone or lateral position. The feet should be extended beyond the edge of the table in order to better discern the response to nerve stimulation (Fig. 30.13). The patient is asked to flex the leg to identify the margins of the popliteal fossa. The fossa is divided into lateral and medial triangles, with the crease at the base of these triangles. The site of needle insertion is 5 cm above the popliteal crease and 1 cm lateral to the midline of the triangle.
After raising a skin wheal of local anesthetic, a 50–100-mm 21-G insulated needle is inserted in a 45° cephalad orientation (Fig. 30.14). The stimulating current is set at 1.0 mA, 2 Hz, and 0.1 ms. The needle is advanced slowly until the appropriate muscle response is obtained. The needle position is adjusted while decreasing the current to 0.35 mA with maintenance of the muscle response.

Figure 30.14 Posterior popliteal block technique. The needle is inserted in a 45° cephalad orientation.
Usually the nerves are located at a depth of 1.5–2 cm, resulting in either plantar flexion and inversion (tibial nerve) or dorsiflexion and eversion (common peroneal nerve) of the foot. When the described responses are not obtained on the first needle pass, the needle is withdrawn and redirected slightly laterally using the same insertion site. Then 30–40 mL of local anesthetic is injected (Fig. 30.15). A single injection technique is usually sufficient with the posterior approach, because the nerves lie in close proximity.
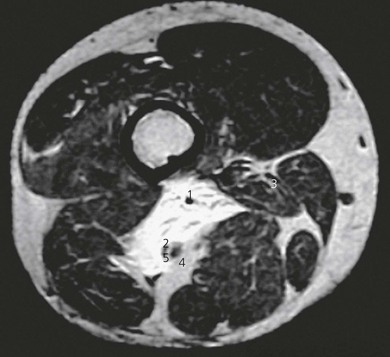
Figure 30.15 Axial T1-weighted MR image showing spread of 20 mL of contrast injected at same level as in Figure 30.3. The common peroneal nerve was stimulated prior to injection. Note the wide spread of contrast in the intermuscular plane, which is significantly widened by the volume of contrast. Note also the apparent movement of the nerves medially and also that contrast does not completely surround the tibial nerve but spreads to areas unnecessary for sciatic nerve block. 1: profunda femoris artery; 2: femoral vessels; 3: common peroneal nerve; 4: tibial nerve; 5: sural communicating nerve.
Ultrasound-guided approach
Intravenous access, electrocardiogram (ECG), pulse oximetry and blood pressure monitoring are established. Maximized comfort for the operator and patient is an important step in pre-procedure preparation. For the ultrasound-guided popliteal sciatic block, the patient is placed in the prone, lateral or supine positions. The operator stands on the side to be blocked, with the ultrasound screen on the opposite side (Fig. 30.16).

Figure 30.16 Global view of the block field for the ultrasound-guided popliteal sciatic nerve block (prone patient position).
In the prone position, the patient is asked to flex their knee to identify the upper border of the popliteal fossa by defining the biceps femoris, and semitendinosus and semimembranosus muscles. Maintaining the knee in a fixed semi-flexed position facilitates block placement. At the apex of the popliteal triangle, the ultrasound transducer is oriented perpendicular to the long axis of the leg, with the ultrasound beam perpendicular to the nerve (Fig. 30.7). The bodies of the semimembranosus and biceps femoris, as well the popliteal artery, vein, and the sciatic nerve, should be identified. The sciatic nerve will appear as a large hyperechoic structure surrounded by a white (hyperechoic) ring and it will lie lateral and superficial to the pulsatile popliteal artery (Fig. 30.8). The target sciatic nerve is placed within the centre of the imaging field of view.
A skin wheal of local anesthetic is raised at a distance from the ultrasound transducer to facilitate sterility and allow a shallow angle of approach to improve needle visualization. The needle bevel should face the active face of the transducer to improve visibility of the needle tip. A freehand technique rather than the use of a needle guide is preferred. A 21-GA × 50–100-mm insulated regional block needle (B. Braun, Bethlehem PA) or 17-GA Tuohy needle (Arrow Intl. reading PA, USA) is inserted within the plane of imaging to visualize the entire shaft and bevel along the path of the ultrasonic beam (Fig. 30.17). The needle is attached to sterile extension tubing, which is connected to a 20-mL syringe and flushed with local anesthetic solution to remove all air from the system. The operator can slide and tilt the transducer to maintain the needle tip within the plane of imaging as much as possible. The needle tip should be clearly identified within the plane of imaging before advancing the needle.
The needle is brought in contact with the nerve, taking care not to puncture it (Fig. 30.18). If an electrical nerve stimulation technique is used, characteristic motor activity of either dorsi- or plantar-flexion is elicited in the foot. After negative aspiration, one mL local anesthetic is injected. If spread of local anesthetic is satisfactory, then a further 3–4 mL of local anesthetic is injected. The needle tip is readjusted posterior to the nerve and another aliquot of local anesthetic is deposited around it. The needle tip is manipulated to deposit anesthetic on all sides of the sciatic nerve. A total of 20 mL of local anesthetic is sufficient to block the sciatic nerve or its terminal branches. The two large branches, posterior tibial nerve and common peroneal nerve, can be individually blocked just below the bifurcation of the sciatic nerve. A larger surface area available for diffusion, and a shorter distance for local anesthetic to reach core fibers hasten the onset of surgical anesthesia.
With the supine patient, a lateral or posterior transducer position can be used. In the lateral transducer position (Fig. 30.19), a transverse image is obtained proximal to the knee joint (Fig. 30.20). A 17-G 3.5-inch needle is used. The needle is introduced through the fleshy part of biceps femoris muscle between its tendon and the iliotibial tract (avoiding the tendon, as tendon injuries heal slowly; Fig. 30.21). The larger bulk of the muscle minimizes peri-catheter leaks. The needle is followed under real-time imaging and the local anesthetic is deposited on all sides of the nerve by repositioning the needle tip as previously described. In the posterior transducer position, a transverse image is obtained proximal to the knee joint (Fig. 30.8). This ultrasound image will be the same as the transverse ultrasound image produced in the prone patient position. The difference in this technique is the needle entry site, which here is from the lateral aspect of the lower limb (Fig. 30.22).
Adverse effects
Clinical pearls
Chan VW, Nova H, Abbas S, et al. Ultrasound examination and localization of the sciatic nerve: a volunteer study. Anesthesiology. 2006;104(2):309-314.
Hadzic A, Vloka JD. A comparison of the posterior versus lateral approaches to the block of the sciatic nerve in the popliteal fossa. Anesthesiology. 1998;88:1480-1486.
Hadzic A, Vloka JD, Singson R, et al. A comparison of intertendinous and classical approaches to popliteal nerve block using magnetic resonance imaging simulation. Anesth Analg. 2002;94:1321-1324.
Schwemmer U, Markus CK, Greim CA, et al. Sonographic imaging of the sciatic nerve and its division in the popliteal fossa in children. Pediatric Anesthesia. 2004;14:1005-1008.
Singelyn FJ, Aye F, Gouverneur JM. Continuous popliteal sciatic nerve block: an original technique to provide postoperative analgesia after foot surgery. Anesth Analg. 1997;84:383-386.
Sinha A, Chan VW. Ultrasound imaging for popliteal sciatic nerve block. Reg Anesth Pain Med. 2004;29:130-134.
Vloka JD, Hadzic A, April E, et al. The division of the sciatic nerve in the popliteal fossa: anatomical implications for popliteal nerve blockade. Anesth Analg. 2001;92:215-217.
Zetlaoui PJ, Bouaziz H. Lateral approach to the sciatic nerve in the popliteal fossa. Anesth Analg. 1998;87:79-82.