45 Popliteal Block
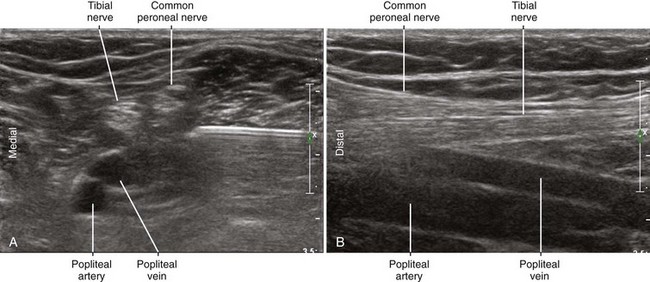
The tibial nerve visibility is best near the knee crease because of the relatively small extremity size. In that location, the typical anatomy is popliteal artery, popliteal vein, and tibial nerve (listed from deep to superficial within a parasagittal plane). The tibial nerve is about twice the size of the common peroneal nerve in terms of cross-sectional area.1 The tibial nerve has a straight course near the middle of the lower extremity, whereas the common peroneal nerve has a more oblique (lateral) course (Table 45-1).
Table 45-1 Characteristics of the Bifurcation of the Sciatic Nerve in the Popliteal Fossa
| Nerve | Common Peroneal Nerve | Tibial Nerve |
|---|---|---|
| Position | Lateral | Medial |
| Posterior (superficial) | Anterior (deep) | |
| Diameter (mm) | 4.0 | 6.5 |
| Course | Oblique | Straight |
| Associated structures | Joins conjoint tendon of biceps femoris distally | Joins popliteal artery and vein distally |
| Echotexture | Less hyperechoic | More hyperechoic |
| Fewer fascicles | More fascicles | |
| Larger fascicles | Smaller fascicles | |
| Response to foot dorsiflexion | Moves anteriorly | Moves posteriorly |
The common peroneal nerve travels distally along the posterior or medial aspect of the conjoint tendon of the biceps femoris near the knee crease. With the foot in neutral position, the common peroneal nerve usually lies slightly closer to the posterior surface of the leg than the tibial nerve.2 Because it is smaller and has fewer fascicles, the common peroneal nerve is more difficult to identify than the tibial nerve.3
Suggested Technique
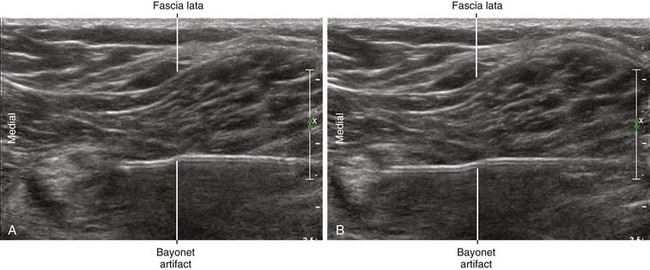
Elevation of the leg and some internal rotation allow imaging of the popliteal fossa from the posterior surface.4 A broad linear transducer (35- to 50-mm footprint, 10 MHz center frequency) is used for most adult patients. The choice of block needle (7- to 9-cm length, 20-22 gauge) is not critical.
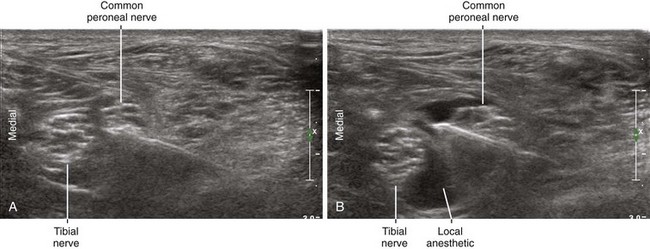
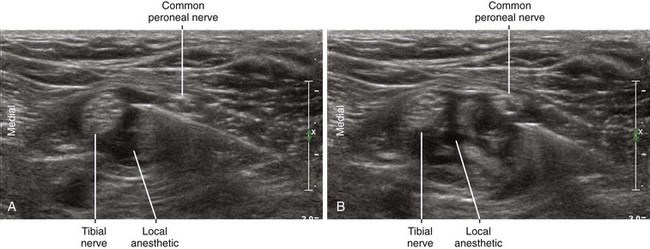
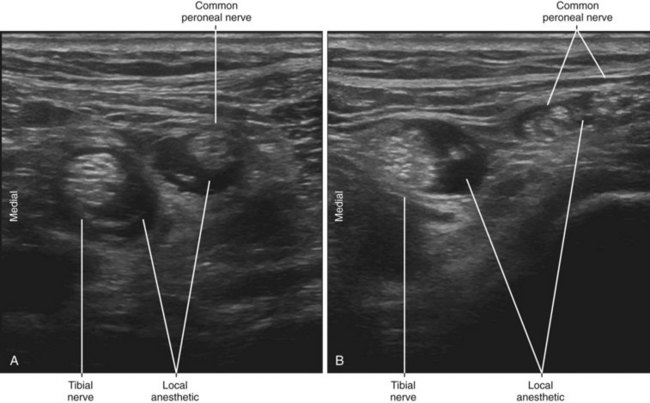
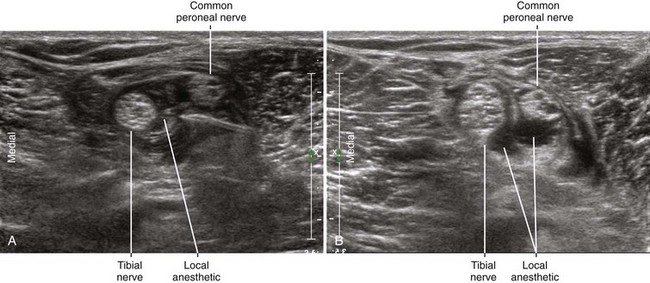
Popliteal block is usually performed just distal to the sciatic nerve bifurcation in the popliteal fossa for several reasons. First, the nerves are close to the posterior skin surface. This makes nerve imaging and positioning the needle tip easier. Second, the needle can be aimed at the connective tissue space between the tibial and common peroneal nerves (rather than directly aimed at the sciatic nerve).5 The block is performed where the tibial and common peroneal nerves are about one needle-width apart (about 1 mm). Third, there is a large amount of nerve surface area available for diffusion of local anesthetic to promote clinical block characteristics. The point of sonographic unity is closer to the knee crease than anatomic dissections would suggest because the tibial and common peroneal nerves run next to each other for some distance before visibly separating. The only potential disadvantage to this more distal popliteal block is that the popliteal vessels are closer to the nerves.
Studies have suggested a limited ability of ultrasound to correctly assess circumferential distribution of local anesthetic around peripheral nerves. The reported predictive value of the “doughnut” sign is only about 90% for sciatic nerve blocks.6 One major advantage to sciatic nerve block in the popliteal fossa is that it allows sliding assessment of the longitudinal distribution along the nerve branches (i.e., local anesthetic should not only surround the nerve but also track along the nerves).
The onset of blockade of the common peroneal nerve is usually faster than for the tibial nerve, which may reflect the smaller size of the common peroneal nerve.7
Key Points
| Popliteal Block | The Essentials |
|---|---|
| Anatomy | The TN is twice the size of the CPN. |
| The TN is approximately 7 mm in diameter. | |
| The CPN is approximately 3.5 mm in diameter. | |
| The CPN is posterior and lateral to the TN. | |
| The TN lies posterior to the popliteal artery and vein at the knee crease (AVN). | |
| The CPN lies medial to the biceps femoris tendon at the knee crease. | |
| Positioning | Supine with leg elevated |
| This allows scanning from the posterior surface of thigh. | |
| Operator | Standing at the side of the patient |
| Display | Across the table |
| Transducer | High-frequency linear, 38- to 50-mm footprint |
| Initial depth setting | 35 to 45 mm |
| Needle | 20 to 21 gauge, 70 mm in length |
| Anatomic location | Begin by scanning with the probe along the knee crease. |
| Slide the transducer proximally from the knee crease. | |
| Identify the confluence of the TN and CPN to form the common SN. | |
| Approach | SAX view, in-plane from lateral to medial |
| Place the needle tip between the TN and CPN at point of bifurcation. | |
| Sonographic assessment | The injection should track distally along the TN and CPN. |
| Anatomic variation | The nerves change position with foot motion. |
CPN, Common peroneal nerve; SAX, short axis; SN, sciatic nerve; TN, tibial nerve.
Clinical Pearls
• Leg elevation and internal rotation help ultrasound-guided popliteal blocks in supine position.
• A hip bump helps rotate the leg into favorable position for popliteal block.
• Slight reverse Trendelenburg position levels the posterior surface of the leg for imaging.
• The only major branches of the sciatic nerve in the thigh are the tibial and common peroneal nerves. The connective tissue between these two branches is the target for the block needle tip and injection.
• Movement of the foot induces characteristic nerve motion in the popliteal fossa that can improve nerve conspicuity (the “seesaw” sign).2
• Ultrasound guidance is particularly useful for locating the bifurcation of the sciatic nerve into the tibial and common peroneal nerves. Most studies have confirmed that popliteal block performed distal to the bifurcation improves clinical block characteristics.8
1 Heinemeyer O, Reimers CD. Ultrasound of radial, ulnar, median, and sciatic nerves in healthy subjects and patients with hereditary motor and sensory neuropathies. Ultrasound Med Biol. 1999;25:481–485.
2 Schafhalter-Zoppoth I, Younger SJ, Collins AB, et al. The “seesaw” sign: improved sonographic identification of the sciatic nerve. Anesthesiology. 2004;101:808–809.
3 Peeters EY, Nieboer KH, Osteaux MM. Sonography of the normal ulnar nerve at Guyon’s canal and of the common peroneal nerve dorsal to the fibular head. J Clin Ultrasound. 2004;32:375–380.
4 Gray AT, Huczko EL, Schafhalter-Zoppoth I. Lateral popliteal nerve block with ultrasound guidance. Reg Anesth Pain Med. 2004;29:507–509.
5 Vloka JD, Hadžić A, Lesser JB, et al. A common epineural sheath for the nerves in the popliteal fossa and its possible implications for sciatic nerve block. Anesth Analg. 1997;84:387–390.
6 Perlas A, Brull R, Chan VW, et al. Ultrasound guidance improves the success of sciatic nerve block at the popliteal fossa. Reg Anesth Pain Med. 2008;33:259–265.
7 Paqueron X, Bouaziz H, Macalou D, et al. The lateral approach to the sciatic nerve at the popliteal fossa: one or two injections? Anesth Analg. 1999;89:1221–1225.
8 Germain G, Lévesque S, Dion N, et al. Brief reports: a comparison of an injection cephalad or caudad to the division of the sciatic nerve for ultrasound-guided popliteal block: a prospective randomized study. Anesth Analg. 2012;114(1):233–235. Epub 2011, Oct 14