Polycythaemia
Introduction
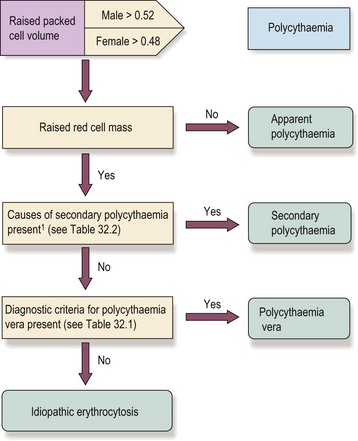
In simple terms, polycythaemia (or erythrocytosis) means an increase in red cell count, haemoglobin and packed cell volume (PCV) above the normally accepted levels. Polycythaemia due to an absolute increase in red cell mass may occur as a myeloproliferative neoplasm (polycythaemia vera (PV) ) or secondary to hypoxia or an abnormal focus of erythropoietin secretion. In ‘apparent polycythaemia’ the raised haemoglobin and PCV are not accompanied by a significantly raised red cell mass; usually the plasma volume is relatively reduced (Fig 32.1).
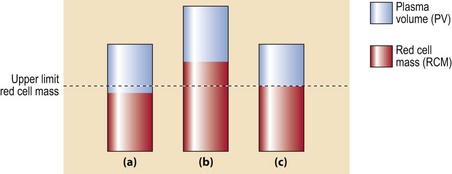
Fig 32.1 Red cell mass and plasma volume in normality, true polycythaemia and apparent polycythaemia.
(a) Normal red cell mass (RCM) and plasma volume (PV). (b) True polycythaemia: there is a significant increase in RCM and total blood volume. (c) Apparent polycythaemia: RCM and PV are at the upper and lower limits of the normal range with a resultant increased haematocrit.
An approach to the patient with polycythaemia
The initial decision to investigate further is taken on the basis of a persisting raised PCV (haematocrit) or haemoglobin level. If true polycythaemia is confirmed by measurement of red cell mass and plasma volume then the next step is to determine whether this is primary or secondary. The full sequence of investigations is not required in all cases. For example, in a patient with known respiratory disease causing chronic hypoxia, a degree of polycythaemia is predictable and does not require investigation (Fig 32.2).
Clinical syndromes
Clinical features. The raised red cell mass and total blood volume with associated hyperviscosity causes the symptoms and signs of the disease. Common complaints include headaches, dizziness, lethargy, sweating and pruritus (the latter particularly after a hot bath). Most importantly, there is an increased risk of arterial and venous thrombosis, particularly strokes. Paradoxically, a combination of hyperviscosity and platelet dysfunction may cause a bleeding tendency. The increased cell turnover can lead to gout (Fig 32.3). Patients are characteristically plethoric and may have rosacea (Fig 32.4). Palpable splenomegaly may be present.
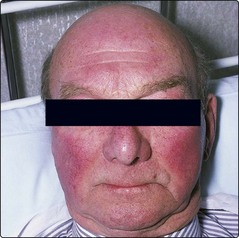
Fig 32.4 The face is a diagnostic clue in polycythaemia vera.
Patients are frequently plethoric and may have rosacea.
Diagnosis. The diagnostic challenge is to differentiate PV from a secondary polycythaemia. Splenomegaly and elevated white cell and platelet counts are suggestive of PV. Increased erythropoiesis can lead to iron deficiency. Erythropoietin estimation by radioimmunoassay is normal or low. The bone marrow aspirate and trephine in PV show hypercellularity but there may be no pathognomonic features. Testing for the JAK2 V617F mutation is now central to the diagnosis of PV (Table 32.1). Around 95% of patients with PV are positive. In the rare negative PV cases, mutations in exon 12 of JAK2 have been found. It is likely that other genetic events (e.g. MPL, TET2 mutations) are required for disease development.
Table 32.1
Diagnostic criteria for polycythaemia vera (PV)1
The diagnosis of PV requires (1) both major criteria and one minor or (2) the first major and two minor criteria.
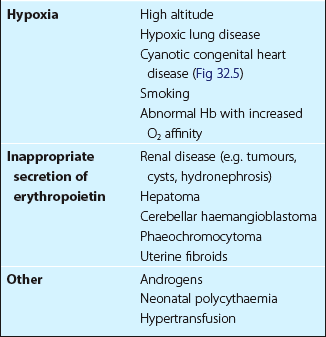
Secondary polycythaemia
This is due to either a physiological response to hypoxia or an inappropriate secretion of erythropoietin. Causes are numerous and are listed in Table 32.2 (and see Fig 32.5). Treatment is essentially that of the underlying cause, although cases with very high PCVs may benefit from venesection.
Apparent polycythaemia
This condition has accumulated several names including spurious, stress or relative polycythaemia, pseudopolycythaemia and Gaisbock’s syndrome. The usual cause is an increase in red cell mass and a decrease in plasma volume within the normally accepted limits (see Fig 32.1). Patients are most frequently male and middle-aged. Other common characteristics are excess weight, hypertension, diuretic use and significant consumption of alcohol and tobacco. The adoption of a healthier lifestyle often leads to resolution of polycythaemia. Venesection is not routine but is considered where there are thrombotic risk factors.