Chapter 9 Polar Medicine
For online-only figures, please go to www.expertconsult.com ![]()
Medical practice in isolated settings is paradigmatic of wilderness medicine: the patient population is essentially, if not literally, a small demographic island. A provisional definition of polar medicine, then, could be “the practice of medicine in isolated settings within an extreme cold environment.” It is the cold, remoteness, hostility, and unforgiving nature of the environment in which humans struggle to survive, let alone work, that make medicine in polar areas, and in particular Antarctica, so challenging.66
The Distinction Between Arctic and Antarctic Medicine
The differences in population patterns mark an important north–south disjunction in polar studies in general and in polar medicine in particular. The northern polar or frigid areas above 66° latitude comprise a frozen sea that is surrounded by eight countries, each with its unique set of populations and medical care services. The countries of the Arctic are Canada, Finland, Greenland (Denmark), Iceland, Norway, Russia, Sweden, and the United States. Together, they make up approximately 8% of the earth’s surface. Human population is scattered throughout the Arctic, with several relatively large urban areas, but for the most part the Arctic is sparsely populated, totaling less than 1% of the world’s population.124 The overall estimated population of the Arctic as defined by the Antarctic Monitoring and Assessment Programme (AMAP) is approximately 4 million; indigenous peoples make up 10% of that population, and constitute the majority of the total population in Greenland and in sparsely settled areas of northern Alaska and Canada.62,123 Within the Arctic, there are 8 major indigenous peoples and more than 30 minority groups. Some of these peoples have separate governments, languages, and socioeconomic possibilities.
There are no indigenous peoples in Antarctica, which is regulated by the Antarctic Treaty, with 12 original and currently a total of 47 signatory countries.4 This complex treaty helps delineate the relationships of the countries that are active in Antarctica and how the continent is to be best preserved and used for peaceful purposes. Seven countries claim territorial rights.4 Of the 79 stations in Antarctica, 39 are operated year-round.22 The total population living in Antarctica, all seasonal, now exceeds 4400 persons in the summer and well over 1100 in the winter.18
In the Arctic, there are two overlapping but distinct spectra of medical problems—those of indigenous Arctic people and those of visitors and immigrants to the polar region. Many of the medical problems among the Inuit, Sami, Chukchi, Nenet, and other northern groups are those of populations making the often Faustian demographic and cultural transition to a Western industrialized society. Thus medical practice among these groups is similar to that among many other displaced indigenous populations. In a sense, the current illnesses and health risks of the indigenous Arctic populations are the results of contamination from distant sources and too much contact with other cultures.14 In contrast, medical problems in Antarctica among the usually young and fit scientific, commercial, tourist, and expedition support personnel are often related to trauma and the environment and thus fall more appropriately under the purview of travel or expedition medicine. Furthermore, tourist cruise ships often bring older adults, whose complex medical problems can create logistic dilemmas. It makes sense to focus not only on the health of elite visitors to these remote areas but also on the health of the local population and the effects caused by visitors.
Importance of Polar Medicine
Increases in Tourism and Expeditions
The combined geographic polar regions cover about one-sixth of the earth’s surface, and their territory in the imagination has been enlarged by several remarkable expeditions and recent popular magazine articles and books on polar tourism. In the past decade, there has been a veritable explosion of tourist activities in both the Arctic and the Antarctic. Despite or because of the forbidding environment, tourism of various sorts is increasing.77 The Arctic is a trendy destination. An estimated 1.5 million tourists visit the Arctic each year, up from 1 million in the prior decade.122 In 1980, it was estimated that a total of 31,000 paying tourists, adventurers, or guests of national scientific expeditions had ever visited Antarctica, but its increasing lure has led to explosive growth. According to International Association of Antarctica Tour Operators (IAATO) statistics, more than 62,000 tourist, staff, and crew visited Antarctica by air or ship in 2009. Since 1989, tourists have visited approximately 200 sites, including 20 research stations in the Antarctic Peninsula region, the most common site for tourists. About 50 of these sites have received more than 100 visitors in any one season, and about the same number have been visited only once. Most visits are to one of 35 sites. Fewer than 10 sites receive around 10,000 visitors each season. The British Antarctic Survey (BAS) monitors Port Lockroy and maintains an ongoing program on the effects the 10,000 visitors per year have on wildlife and ecology of the area.49 Although the bulk of tourists visit aboard cruise ships, there is an increasing number of overland participants who engage in camping, kayaking, diving, skydiving, mountaineering, Arctic or Antarctic traverses, polar challenges, and adventure tourism.50,77
Concerns about the dramatic increase in tourism and its effect on the ecosystem have led to a movement to limit the total number of tourist visits per year. The World Wildlife Fund and the United Nations have proposed guidelines to developing ecofriendly tourism in the Arctic. The guidelines cover its impact on the environment as well as on local populations. In April 2009 the consultative countries of the Antarctic Treaty endorsed a proposal to limit the size of cruise ships and the number of tourists who can go ashore at any one time and to eventually make it binding to all parties.122
This increasing number of visitors and expeditioners has created interest in polar medicine, in particular as it relates to land-based and extreme expeditions. Wilderness medicine courses specific to polar medicine are now offered. Tourist vessels generally carry a physician and sometimes a nurse. Although facilities vary in level of care, all have preparations for the most frequently encountered medical problems. Most illnesses are upper respiratory infections, gastrointestinal (GI) problems, motion sickness, and mild bruises or strains. As might be expected given the ages of many visitors, an occasional cardiac event or serious fracture occurs. The occasional expeditioner who needs rescue or assistance from a scientific station uses scarce resources.23,77 One peculiar phenomenon is that when patients and medical/rescue/evacuation resources are from different countries, a complex flurry of high-level diplomatic interchange must often occur before help can be rendered.
Perhaps the most notable tourist fatalities were associated with the ill-fated skydiving venture at the South Pole, which resulted in the death of three of the four participants,45 and the Air New Zealand flight that crashed into Mt Erebus with the death of all 257 people aboard.83
Hazards are inherent in any expedition and may well be the attraction for some participants. To be allowed to participate in risky activities, some tourists may fail to declare serious medical problems that later precipitate emergency medical evacuation. Thus one real concern is increased risk taking and the consequences thereof, or the dilemma between what is reasonable and what is foolhardy. From a medical perspective, making a risk assessment is multifactorial and differs for people, places, and goals. Hazards of an evacuation need to be assessed for both the patient and rescuers. Setting guidelines and anticipating needs in pre-event preparation are the keys to successful evacuation.46 Because of the occasional tourist in need of expeditious medical evacuation, IAATO and other governmental groups have suggested requiring insurance to defray the costs associated with these evacuations. There is also discussion of the ethical versus medicolegal implications of whether to render aid. The overriding issue should be care of the patient. Polar Challenges and expeditions are discussed later (see Medical Aspects of Arctic Racing).
Increases in Research Activities
Scientific research has been a part of polar exploration throughout this century. There are scientific and medical journals devoted to the polar regions, and thousands of articles are indexed each year in the Antarctic Bibliography (http://www.coldregions.org/antinfo.htm). The International Journal of Circumpolar Health (http://ijch.fi/Issues.htm) is a richer source for health issues in polar regions. Antarctic research continues to expand. All the continent’s permanent stations are primarily there to support research. The biggest study is the IceCube project at the South Pole station, which uses a series of downward-looking detectors spread over a square kilometer to look for traces of the notoriously elusive neutrinos, invisible particles churned out by nuclear reactions. The detectors seek particles that have already passed through the earth. The South Pole also hosts two large telescopes.
Another huge project involving multiple countries is ice core drilling, designed to catalog climate changes of tens of thousands of years. Other scientific endeavors include marine biology and ocean dynamics research; atmospheric and climatologic research, including air cleanliness monitoring and ice sheet movements; medical research (primarily at Japanese and Chinese stations)80; biologic research (ecosystems, penguins, seals, bacteria, lichen); seismic monitoring; aerial and sea floor mapping with unmanned vehicles in the harsh environment; paleontology; meteorite searches; and demonstrations of alternative power in extreme circumstances (e.g., wind generators at New Zealand’s Scott Base).
Some observers have discerned a north–south split, perceiving research in Antarctica as having more of a political motivation and that in the Arctic as being more practical. For both scientific and political reasons, an important part of scientific research in polar regions concerns environmental issues. The remoteness of these regions enhances their value as benchmarks for studies of pollution. Indeed, several worrisome facts have been revealed about the contamination of formerly pristine wilderness, such as widespread radioactive contamination, the prolonged effective half-life of radioactive fallout deposits,115,125 and increased chemical contamination, particularly in animals high on the food chain, with persistent organic compounds, heavy metals, and other contaminants affecting the environment and food supply.68,125 Widening of the ozone hole carries implications of increased ultraviolet (UV) radiation. As occupational and environmental health issues draw more attention, this aspect of polar medicine assumes greater importance.27,28
Brief History of Human Habitation in Polar Regions
A perspective on the contrasts between Arctic and Antarctic medicine may be sharpened by a brief summary of human habitation in polar areas. Humans are known to have inhabited Arctic regions for at least 4500 years. Anthropologists have uncovered evidence for several waves of population migration from Siberia through northern Canada to Greenland. Each of these migrations was probably linked to climatic conditions, and each resulted in a distinct set of cultures. The general pattern was of a nomadic life with population densities of approximately one person per 400 km2 (154.4 square miles).52,118 In more recent times, this long-established and remarkable adaptation to a hostile environment has been disturbed. The pace of cultural change increased dramatically during the second half of the 19th century, when the whaling industry moved into Hudson Bay, leading to sustained contact between Europeans and the Inuit. In the early part of the 20th century, religious missions, trading company posts, government stations, church missions, and eventually medical clinics and schools began to encourage permanent settlements, roughly quadrupling the population density.52 In some areas, such as Eurasia, large industrial and mining cities arose. This change in population distribution has at times led to conflict between indigenous and European cultures, and it has had significant environmental and medical consequences.126
The known history of human exploration of Antarctica, unlike that of the Arctic, is quite recent. Recorded sightings of the continent date only to around 1800, and “winter-over” sojourns did not occur for another century. Waves of settlement can also be observed to have occurred in Antarctica; there was sealing in the early 19th century and whaling in the early 20th, and there has been scientific exploration since the mid-20th century.118 The heroic era of Antarctic exploration occupied the early years of the 20th century, with exploits such as the highly publicized race for the South Pole between Roald Amundsen and Robert Scott in 1911, the extraordinary survival of the crew of the 1914 Endurance expedition, led by Ernest Shackleton,61 and the heroic survival of Douglas Mawson, an Australian geologist who wintered alone after his other expedition members perished.72 Perhaps because of these and other dramatic events, and perhaps because of the absence of an indigenous population and a scarcity of easily exploited resources, human activities in the Antarctic have retained a somewhat more expeditionary flavor than in the Arctic. This has helped shape the contrasts in medical practice between the northern and southern polar regions.
Arctic Medical Problems
Effects of Cultural and Demographic Transition
The Arctic is not a homogeneous region. Although the population is only approximately 4 million, it is very diverse, with few features in common except the latitude of residence and hours of daylight. Medical problems among indigenous populations in the Arctic, approximately 10% of the total population, are characteristic of displaced aboriginal people elsewhere in the world. There is a wide range of interrelated factors, including demographics; the social, economic, and physical environments; personal health practices; and availability of good-quality and culturally appropriate health care services.12,53 Although increased contact with industrialized cultures has brought benefits, it has also brought many problems. Some of the benefits include greatly improved life expectancy, largely due to a decrease in morbidity and mortality from infectious diseases and diseases of childhood (prevented by vaccines). Nevertheless, in indigenous Arctic peoples of the United States, Canada, and Greenland, infant mortality is higher and life expectancy is lower when compared with Arctic dwellers in Nordic countries.98 For many years, health care has lagged behind national norms in the Canadian Arctic, with infant mortality 2 to 3.5 times the national average.113 Age-adjusted death rates are also telling, with 8.4 per 1000 Northern Canadian people, compared with 5.8 per 1000 for the Canadian national average; 14.3 per 1000 in Greenland and up to 29.2 per 1000 in parts of Russia. Other striking statistics reveal a suicide rate in Nunavik six times that of the southern provinces of Canada,60,119 and an unintentional accidental death rate three to four times higher than the national average. Tuberculosis has decreased but is still unacceptably prevalent at 47 versus 7.1 per 100,000 persons. Diabetes mellitus has increased to 5% of the population of 30- to 39-year-olds, compared with 1% in the general Canadian population. In a population in which dental caries were previously almost unknown, the need for restorative dental work is up to 60%. Widely prevalent alcoholism and tobacco use greatly contribute to these problems.10,42,113 As the Arctic environment and indigenous Arctic populations make the cultural and demographic transitions to a Western industrialized way of life, the spectrum of medical problems has shifted. Changing social patterns have resulted in disturbing trends: increasing numbers of young adolescent mothers, rising prevalence of gonorrhea and syphilis among Greenlanders, and concerns about other transmissible diseases, such as viral hepatitis and acquired immunodeficiency syndrome (AIDS).76,130 Changes from the traditional diet and lifestyle have led to increased obesity, diabetes, cardiovascular disease, and mental health problems, including depression, binge drinking, alcoholism, and higher suicide rate.12,113,119
Environmental and Occupational Health Problems
Transboundary pollutants, primarily from Eurasia and the North American continent, have made deep and lasting changes.10 The Arctic, once viewed as pristine, is now considered a pollutant sink. Even so, promising new data reflect that strict environmental control (e.g., bans/restrictions on uses and emissions of persistent organic pollutants [POPs]) is working.123 The nuclear accident at Chernobyl in April 1986 led to cesium-134 and cesium-137 levels in reindeer meat 50 to 100 times those considered safe, forcing destruction of the Sami reindeer herds. During that same time, lake fishing and berry picking were curtailed because of contamination.37,126 Fortunately, research 20 years since this accident demonstrates thriving flora and fauna even in the most contaminated areas, demonstrating a rebounding environment. Nevertheless, the young people exposed to the nuclear accident have shown an impressive increase in thyroid cancers, and those exposed to the highest doses of radiation show an increase in leukemias, solid cancers, and circulatory system diseases.114 Industrial emissions from neighboring regions, including an estimated 100 million tons of sulfur dioxide, have led to the “Arctic haze” phenomenon, a gradual whitening of the historically deep-blue Arctic sky.37
Environmental impacts have had direct health consequences.10,42 During the last 500 years, industrial pollution has led to a sevenfold increase in lead levels in human tissues in the Arctic.37 Another survey found blood mercury levels above the normative limit in over 10% of Sami reindeer herders in northern Finland. In North Greenland, a study revealed that in 84% of human mothers, blood mercury levels were above the World Health Organization provisional limit.39 Oceans, rivers, and lakes reveal contamination and concentration of heavy metals in fish.126 Further contamination of the food chain with long-lasting POPs, including polychlorinated biphenyls (PCBs) and many organic pesticides, is increasingly identified.28,126 Long-term consequences of environmental pollutants on the health of the Arctic dwellers continue to be studied.27,28 Recent work suggests that the endocrine-disrupting effects of PCBs may have changed the normal ratio of male-to-female births from 1.05 to 1.02 in the past 30 years.12 It has been documented that the concentrations of PCBs in breast milk are seven times higher in the Arctic than in Quebec.113 As previously noted, fallout from radioactive testing has caused river pollution, and other environmental degradations have affected the food chain, such that it is estimated that an increase in certain cancers has been noted in both animals and humans.132 Fear of the effect of pollutants has caused many to abandon or significantly limit their consumption of traditional foods (e.g., marine mammals, fish, terrestrial mammals, and birds). Unfortunately, this can have negative nutritional effects, such as obesity, diabetes, and increased cardiovascular disease, and in some instances relative malnutrition.38 Tragically, POPs, even in low concentrations, have been shown to cause increased risk for diabetes, so both consumption of traditional foods and changes in diet to processed foods have contributed to the increased rate of diabetes in these regions.123 In some areas, consumption of traditional marine foods has led to blood levels of mercury exceeding current recommendations. Local health departments have to weigh overall nutritional benefits of traditional land and marine food sources against the potential long-term risks of neuropsychological and other potential health problems, particularly in newborns and infants.68 Fortunately, new trends show human exposure to pollutants in the Arctic is decreasing. For example, the number of Arctic childbearing-age women with excessive levels of PCBs, mercury, and lead is decreasing. This is believed to be due to dietary changes and increased awareness of the problem. However, new research is demonstrating many additional chemicals, some newly developed, that have the potential to collect in the Arctic food chain, so ongoing research, identification of these chemicals, and regulation of them are essential to continue improving the health of indigenous peoples.123
Nontoxicologic factors also make important contributions to Arctic morbidity and mortality. Accidents are more prevalent in the Arctic. In younger (up to age 35) Inuit groups, injuries account for approximately one-third of all deaths.15 It is striking that Alaska’s occupational death rate is three to four times that of the U.S. national average deaths per 100,000 workers, but this is markedly improved from five times the national average in the 1990s.85 With establishment of the Alaska surveillance system in 1991, there has been a 50% reduction in work-related deaths, including a significant reduction in commercial fishing deaths and very sharp decline in helicopter logging–related deaths.21 These data reflect in part the inherently hazardous working conditions and occupations and possible demographic biases of a young population. Other factors, however, may play a role. Because aircraft are a predominant mode of transportation in polar regions, it is not surprising that Alaska accounted for greater than one-third of all air crashes in the United States and 20% of the fatalities from 1990 to 2008.84 Nonscheduled or commuter plane (less than 30 seats) flights, commonly used in isolated areas, pose a risk for fatal crash six times that of scheduled airline flights, a figure not surprising given the often extremely challenging flying conditions (terrain, weather, and isolated landing sites with limited navigational aids and operator error). In recent years, the pilot occupational fatality rate has fallen from 298 to 148 per 100,000 (less than twice the rate for all U.S. pilots), felt to be due largely to increased awareness and proactive intervention in the industry.84 Overall, the mortality rate for Alaska natives is 939 per 100,000 per year as compared with the overall U.S. rate of 698.9 per 100,000 per year.123
Psychosocial Health Problems
With social disruption and increased environmental and occupational health risks, psychological problems in the Arctic have achieved greater visibility in recent years. For a variety of reasons, stress seems to be higher in winter. One survey of over 7000 adults living north of the Arctic Circle found a prevalence of midwinter mental distress of 14% in men and 19% in women.40 Most other studies suggest that this figure may be low. One study among Inuit found that 22%, or one in five, experience depression during the winter months, and 7% appeared to have seasonal affective disorder (SAD).36 Cultural stress, erosion of traditional lifestyles, and substance abuse are all contributory factors.12 Studies investigating scientific staff at Arctic research stations are relatively uncommon, but they show patterns of sleep disturbances, depression, and alcohol use reminiscent of those in Antarctic stations. The double apparent risk factors of high latitude and displaced indigenous populations have made alcohol abuse and concomitant violence a serious problem in the Arctic. In Greenland, one in three Inuit dies a violent death, and roughly 25,000 adults consume 28 million cans of beer a year, one of the highest per capita consumptions of alcohol in the world. Prevalence of “binge drinking” among Arctic peoples ranges from 12% to 39%, with male rates being greater than female rates. Fetal alcohol syndrome is 13% higher in Alaska than in the continental United States.12 One study compared alcohol consumption by the Greenland Inuit with nonindigenous local inhabitants and found that alcohol consumption was less among the Inuit. However, other studies found the reverse.60 Accidents are the leading cause of death in the Arctic, and one-third of these are estimated to be alcohol related. In the Canadian Arctic, alcohol consumption is one and a half times the national average, and Inuit and Indians between 15 and 24 years of age have a suicide rate up to 11 times the national average. In some communities, for boys and men ages 15 to 29, suicides are the most common form of injury leading to death.60,82
Current and Future Trends
In summary, indigenous populations of the Arctic show lower life expectancy, higher rates of infectious diseases, higher infant mortality, and higher rates of injuries and suicides when compared with norms in their respective countries.123 Fortunately, there are encouraging signs related to Arctic health care. The incidence of low birth weight, 5.5% in the central Canadian Arctic, has decreased, although it is still higher than that among non-Arctic dwellers.12 Tuberculosis, which incapacitated up to 20% of the Canadian Inuit by 1950, has largely been brought under control, although the rate of occurrence is still as much as 10 times the national average.15 Trends in environmental and occupational health problems show increased monitoring, intervention, and improvement. Unfortunately, the age-adjusted incidence of diabetes mellitus is dramatically rising among First Nations populations.25
An important development in recent years has been the institution of trauma registries to track and target significant causes of morbidity and mortality. Recent research emphasizes that injury prevention is not solely a function of safer design of equipment but is a complex interplay of environment, activity, and people, notably including personal risk-taking behavior. If current trends continue toward greater economic independence and education of Arctic peoples, such potentially modifiable adverse health behaviors may recede in importance in coming years.58,59
Antarctic Medical Practice
Medical practice, problems, and their study in the Antarctic are somewhat different from those in the Arctic. Extreme isolation makes Antarctic medicine unique. Because of the remoteness, it may not be possible to medically evacuate (medevac) a patient for weeks or even months. It might be easier to medevac from the international space station than from some of the more remote Antarctic stations.35 In general, the population is adult and is physically and mentally healthy, although at least the U.S. Antarctic Program grants health waivers to some individuals with certain chronic diseases so that they can visit or work for a limited time. Winter-over personnel, including those spending a year or more at a time in Antarctica, are required to pass medical screening that varies in intensity with the various national programs. Most stations only house adults. There are two exceptions: Chile and Argentina have families living at their principal bases and have even had children born on them. All stations have some form of medical care, usually a station physician. The more temporary camps have varied medical support, ranging from first-aid wilderness responders to paramedics or midlevel providers with limited medical supplies. In general, the permanent year-round bases have more sophisticated facilities, with radiograph, laboratory, surgical, and dental provisions and a reasonably well-stocked pharmacy for expected emergencies. There is at least one physician and sometimes nurses and ancillary medical personnel.
Medical Stations in Antarctica
What type of physician is needed? To paraphrase Grant, the physician cannot be too specialized in approach; broad knowledge and a wide range of practical skills are necessary to provide good Antarctic medical care.35 Specialization in emergency medicine or the equivalent seems to be a suitable choice, especially to deal with emergencies. In nearly all bases, there is no room for the luxury of anesthetists and surgeons, dermatologists, and psychiatrists. These roles reside within the same person. However, modern communication, including video teleconferencing (VTC), help the polar physician be less isolated from advice, counsel, and guidance. For a significant proportion of the Antarctic population, it is still extremely difficult and costly to evacuate patients.35
The following is a description of the personnel and facilities in the U.S. Antarctic Program; other nations maintain similar facilities. McMurdo Station (MCM) has the largest population—around 200 in the winter and 1200 in the summer. Whereas the winter MCM and South Pole populations are isolated, their summer populations constantly have an influx of rotating personnel that bring new diseases. In the summer season, the medical component is staffed with two physicians, a physician’s assistant or nurse practitioner, an Air Force flight surgeon, a dentist, a radiograph technician, a laboratory technician, and a physical therapist. In the winter, the staff is composed of one physician, a physician’s assistant, and a physical therapist. All are cross trained on site. (Other large national stations provide necessary additional training in advance.) In addition, MCM has a full fire department with paramedics who respond to emergencies on station. The South Pole population peaks at 250-plus in summers and reaches a nadir of around 50 in the winter. There is one physician, a physician’s assistant or nurse practitioner, and a volunteer trauma team trained on station. Palmer Station is the smallest, with a population of 45 in the summer and a low of 10 to 20 persons in the winter. There is one physician, and volunteers are trained on site to provide assistance. How well these volunteers can function was demonstrated in 2009 when the station’s physician developed a peritonsillar abscess. She had one of the station emergency medical technicians needle drain and then incise it under topical and local anesthesia. She then used VTC and an intraoral camera to consult with an otolaryngologist based in the United States. She improved within a few days.26
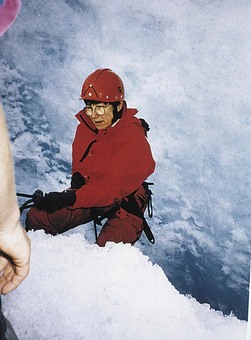
The Australian stations have one physician. Before deployment, there is a 2-week training course for two of the crew in operating-theater nursing skills and for two persons in anesthesia assisting. The predeployment training has proved very valuable, as was clearly demonstrated in the case of a scientist who fell into a crevasse and suffered serious injuries, including internal bleeding, that required on-site surgery (Figure 9-1).102
The South Pole does not have 24-hour satellite coverage, but year-round stations have facilities for telemedicine, including live camera, still photos, fax, and digital radiography for transmission and consultation via satellite and the Internet. VTC, used for many years in Antarctica by multiple programs,35 came of age at the South Pole in 2002 with a midwinter repair of a patellar tendon rupture. The tendon was surgically reattached by the base physician under the direction of consultants at major medical centers via live video and voice connection. Various physicians at Antarctic stations are also able to consult with colleagues via VTC, such as with the South Pole medical staff’s successful management of a severely hypotensive tourist in 2009 with VTC input from MCM clinicians. In addition, telemedicine has been used for diagnosis and consultation in the treatment of a wide variety of ailments, including acute cholecystitis, ophthalmologic lesions, pancreatitis, pericarditis, fracture treatment, psychological consultations, radiologic reports, and many other situations. Telemedicine has improved the quality and availability of sophisticated care in these and other remote, hostile environments.
Medevacs are frequently dangerous and costly. Summer is the only season during which some stations can be reached for an evacuation. Winter evacuations are infrequent, very dangerous, and costly. Logistically it may be 2 or more weeks before a rescue can take place, and for some stations it may not even be possible. A historic medical evacuation from the South Pole was undertaken in the winter of 2001 with the first successful landing of a twin Otter aircraft in full darkness at a temperature of −68.9° C (−92° F) (Figure 9-2). This event, while fraught with danger, has opened new possibilities and has been repeated.16,19
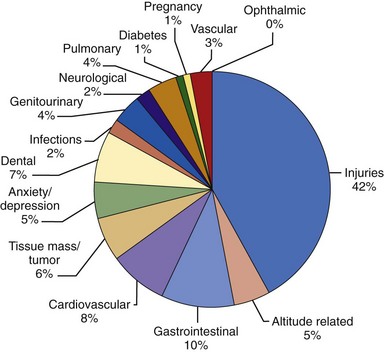
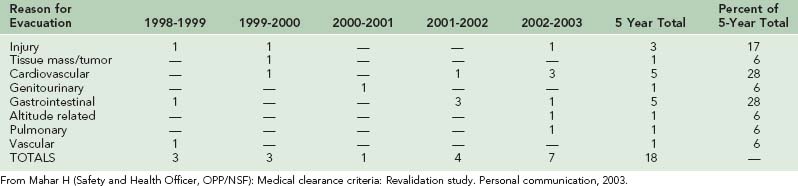
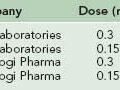
To reduce the number of medical crises and need for urgent medical evacuations, all participants must pass a “physical qualification test.” Medical clearance criteria are used as a screening tool. To establish appropriate guidelines, evidence-based criteria from the medical literature, historical data of the Antarctic Program, and guidelines from other programs, such as the National Aeronautics and Space Administration (NASA), the Peace Corps, and the Navy, that have activities in remote areas were used. What appears to be lacking is screening for body mass index and alcoholism. However, up to 30% of all medical evacuations (both emergent and urgent) have been for trauma—that is, they were not related to the evaluation criteria. Of emergent and urgent evacuations, 10% were for GI and 8% for cardiovascular reasons (Figure 9-3). Considering only truly emergent medical evacuations, 28% were for cardiovascular and 28% were for GI reasons (Table 9-1). Figure 9-4, online is a chart showing the number of medevacs from MCM and the South Pole station.
Somatic Health Problems
Many of the primarily somatic health problems in Antarctica have to do with cold, altitude, and trauma and are thoroughly covered in the chapters on those topics. In a midwinter setting where a tossed mug of coffee freezes before the liquid hits the ground, the dangers of frostbite are clear. Anyone gasping for breath after climbing the six flights of stairs with 92 steps from the tunnel to the living area of the South Pole’s elevated station, or who has lost 5 kg (11 lb) in the first 2 weeks merely from resting tachycardia and tachypnea, can appreciate the physiologic stresses of rapid ascent to an equivalent of 3200 m (10,499 feet). Likewise, the dangers of UV exposure at altitude with an ozone hole and snow surface reflectance of 80% to 90% can become painfully evident to the unwary visitor.20,112
Cold-Related Problems
Cold is a dominant factor in polar medicine. It can be a source of humor, such as the infamous “300 Degree Club” at the South Pole. Membership requires sprinting, while somewhat less than completely clothed, from a 93.3° C (200° F) sauna to the Pole outside at an ambient temperature of −73.3° C (−100° F) or lower. Similarly, the quintessential polar first-aid story involves creative solutions to the problem of finding warm fluids,2 but it would be reckless to forget the ever-present danger of such a hostile environment. Windchill commonly drops the effective temperature far below −73° C (−100° F). It has been estimated that under the most severe winter conditions, an inactive person in full polar clothing could undergo a life-threatening drop in core temperature in only 20 minutes. Airplane refueling crews and others working with liquids at polar ambient temperatures are constantly reminded that even a small splash can mean instant frostbite.31
Rescue and treatment are complicated by the additional need for both victim and rescuer to avoid hypothermia and frostbite.52,54 Disorientation and confusion from hypothermia, clumsiness from bulky clothing, and degraded performance characteristics of equipment and intravenous (IV) fluids can complicate otherwise straightforward procedures. A recent case report describes almost immediate freezing of fluid in IV lines and shattering of the plastic IV tubing despite vigorous attempts to warm them.54 Simple devices commonly used in warmer settings, such as air splints and pneumatic antishock garments, would be similarly unusable. In more sophisticated equipment, batteries rapidly fail, unwinterized mechanical moving parts seize up, and metal objects become dangerous sources of frostbite.
Clothing, not normally considered a medical topic, assumes special importance in the polar environment (Figure 9-5).73,100 Although the clothing used for many polar research programs in the summer seems adequate, a strong argument can be made for specialized winter gear, possibly adapted from the space program, that would allow relatively delicate manipulation of scientific equipment while offering protection from the cold. In fact, at temperatures below those of most military specifications, material properties of equipment, including plastic electrical insulation, create unexpected hazards, such as splitting of insulation and other plastics, and extreme rigidity of cables and hoses such that they cannot be used. Fortunately, the importance of ergonomic issues in the design of machinery and clothing for polar conditions is receiving increased attention.44,128 There is new research on use of personal heaters, which are particularly effective for extreme cold and for sedentary work in the cold.106 Phase-change material can store latent heat and then release it during periods of low activity.100 These newer materials will allow thinner gloves with high thermal protection to be worn for work in the cold that requires dexterity, and they will be particularly effective for persons whose efforts alternate between heavy work that can produce sweating and light work with associated cooling (Figure 9-6, online). In addition, as phase-change material clothing becomes readily available, clothing will be lighter and less bulky, particularly advantageous when doing intricate work in the cold as well as alternating active with sedentary work in the cold.
Altitude Illnesses
Because medication use was voluntary, complications seen from not taking it included high-altitude pulmonary edema requiring use of a Gamow bag before urgent evacuation, relative hypoxemia, and decreased work tolerance. Complications from taking acetazolamide included dehydration and electrolyte abnormalities in patients who were already ill or had severe underlying diseases.51 Please see Chapter 1 for current recommendations for prophylaxis and treatment of high-altitude related illnesses.
Nutritional Studies
Nutrition occupies a key niche throughout the history of polar expeditions. Early expeditions in both polar regions provided several examples of nutritional illnesses, including scurvy and possible hypervitaminosis A and lead poisoning. More sophisticated nutritional analyses have been possible during recent expeditions,112,116 and advances continue to be made in development of lightweight but nutritionally dense rations. When participants in endurance events are well trained, it is possible to compete without loss of lean body mass.70 Although many prolonged unsupported expeditions include an element of malnutrition or even starvation, protein synthesis is still active.116,117
During a Canadian-Soviet transpolar ski trek, participants skiing approximately 20 km/day (12.4 miles/day) at a speed of about 3.5 km/hr (2.2 miles/hr) while carrying 37- to 45-kg (81.6- to 99.2-lb) packs showed increased strength, decreased body fat, and increased high-density lipoprotein cholesterol. A paradoxical drop in aerobic power was noticed, perhaps because of intensive pretraining and conditioning, as well as increased efficiency of skiing as the trip progressed. More recently in a nonsupported, two-man, 86-day trans-Greenland trip, well-trained and experienced skiers eating an adequate caloric diet had little if any significant impairment. Their average energy intake in rugged terrain was 28 to 34 kJ/day (6688 to 8121 cal/day) and in level terrain 14 to 16 kJ/day (3344 to 3822 cal/day).31 Although applicability of these figures to more sedentary polar sojourners is probably limited, work is being done to alter the diets of more sedentary expeditions to improve the lipid profile of participants.71 Better availability of common foods and fresh fruits and vegetables during the summer, and frozen foods in the winter at the permanent stations allow participants to choose a healthier diet. However, frequent fried and high-fat food intake leads to elevation of lipid profiles and the associated increase in cardiovascular risks. Some studies have demonstrated that it is possible to make simple and acceptable changes in food preparation that have a significant impact on lowering cardiovascular risk factors of winter-over personnel.6,71
An area that has received increased attention involves the possibility that the prolonged low dose of sunlight may have long-term effects on bone metabolism and immune and cardiovascular systems. One study showed a decrease in the 25-hydroxy metabolite of vitamin D (25OHD) as UV radiation ceased. However, the active metabolite 1,25-dihydroxyvitamin D (1,25[OH]2D) did not show such variation.101 A few studies have demonstrated significant decreases in serum vitamin D as measured by 1,25(OH)2D and associated increases in serum osteocalcin during the dark period, possibly indicating bone remodeling.133 Another study in which low doses of vitamin D were given showed increased bone mass in lumbar vertebrae and leg bones, but no bone mass increase in the pelvis or upper extremities. This was felt to be the result of vigorous activity over the winter. The study also showed a decrease in serum calcium and 25OHD levels during the winter.86 A study was undertaken in the 2003-2004 Antarctic summer and followed 53 Australian expeditioners for 2 years. It showed that they became vitamin D deficient after just a few months; after 12 months, this began to result in loss of bone density. Further study is planned to identify the minimal dose of supplementation needed to prevent deficiency and whether these expeditioners have greater risk for developing osteoporosis in later life.55 Because many participants return for successive winters, further studies are needed to delineate possible long-term effects of bone mass after redeployment.
Infection and Epidemiology
With particular reference to the space station analogy, a number of studies have taken advantage of the physical isolation of Antarctic stations as a natural laboratory for infectious disease epidemiology. Because microorganisms are believed not to survive the extreme cold long enough to be carried in by winds, midwinter respiratory tract infection outbreaks in the absence of outside contacts have suggested that such organisms could persist in clothing or other fomites.97
Despite a widely reported leukopenia, decrease in cell-mediated immunity, and decreases in salivary IgA and IgM during the isolation of wintering over, it is not clear whether persons emerging from Antarctic stations are more susceptible to infection,30 or whether the changes in immunity are related to the stress associated with a winter over.
Circadian Rhythms, Endocrine Studies, and Sleep Research
Pioneering studies of Natani and colleagues79 and Shurley and co-workers on sleep electroencephalograms at the old South Pole station demonstrated clear patterns of sleep disturbances and “free cycling” of the sleep–activity cycle. Some of these findings have been extended in more recent studies. For example, among four subjects at a small winter-over camp, summer sleep cycles synchronized within the group and with clock time. During 126 days of sunless winter, rhythms free cycled in all four people and then resynchronized with reappearance of the sun.57 The degree of synchrony versus free cycling appears to depend on a number of factors, notably zeitgeber strength (an environmental agent or event that provides the cue for setting or resetting a biologic clock—that is, activities, social contacts, and the most important zeitgeber in nature, light).32 Studies in Indian stations also confirm continuing sleep pattern changes.13
A number of studies have examined the effect of prolonged polar residence on diurnal variations in the level of melatonin. Its important role in free radical scavenging and sleep regulation is beginning to be elucidated.56 Melatonin has been studied as a chronobiotic and is used as a supplement to treat circadian rhythm disorders.5,109 Of the various studies using melatonin to treat sleep disorders, including delayed sleep phase and for night-shift workers, most have only small numbers of participants. Although the initial studies are promising, more research needs to be done. It appears that exogenous melatonin can be used effectively for most persons. The short-term side effects (headache, nausea, and drowsiness) are few. There are no long-term studies. Use of blue-enriched white light in the workplace improved alertness, performance, and sleep quality, as well as daily resetting of the melatonin cycle.29,75,109
Other endocrine fluctuations also appear to be correlated with the length of the day.122 Some endocrine studies have examined the effects of prolonged residence in polar regions with a longer than diurnal time constant. Twenty-four-hour urinary excretion of catecholamines increases in the cold, but social stresses appear to overwhelm climatic determinants of catecholamine metabolism, correlating with increases in diastolic blood pressure and pulse during the year.41 A more consistent pattern of elevated thyroid-stimulating hormone (TSH), decreased free thyroid hormones, and increased triiodothyronine (T3) clearance after several months has been demonstrated. It has been suggested that rapid clearance of T3 is caused by the cold. A pattern of increased pituitary release of TSH in response to IV thyrotropin-releasing hormone and increased serum clearance of orally administered T3 has been identified and dubbed the “polar T3 syndrome.”24 The full clinical significance of these findings remains unclear, but it appears that the T3 may well be related to the winter-over syndrome (see later).87,95 Several studies that used thyroxine supplementation noted improvement in midwinter cognitive function, mood, and vigor.102,105,127
Environmental Health Issues
Because of Antarctica’s isolation, it seems a particularly disturbing site for litter and pollution. As in the Arctic, events such as the early problems with a nuclear reactor at MCM (since removed) and the 1989 oil spill from the Bahia Paraiso near Palmer Station, and studies by groups such as Greenpeace, have focused attention on environmental health risks in the Antarctic.78,125 Environmental inspections at a broad range of Antarctic stations have raised concern about toxic effluents and heavy-metal residues, as well as about radioisotopes used for research. To address these issues, a number of countries have begun to implement more responsible waste-management and water-monitoring policies and are taking corrective actions. Most have active recycling programs in place, and many cleanups are in progress or have been completed. Currently, most stations, including all U.S. stations, discharge raw sewage. Proposals are in place to find a way to ameliorate the contamination from raw sewage that is discharged into the sea, and/or into large bubble holes in the ice for the inland stations. The BAS Rothera Station installed a sewage treatment plant with significant improvement in the near-shore marine environment.47,48,74
Occupational Health and Injury Prevention
Rigorous studies of risk are important for injury prevention. Unfortunately, they are complex and often bedeviled by challenges, including controversial data, multiple variables, and biases. For example, for purposes of occupational epidemiology, it may ultimately prove useful to stratify the Antarctic sojourner population into groups such as sport expeditions, military, commercial, and scientific, but the health behaviors of these groups overlap, and few studies have gone beyond aggregate descriptive statistics. There is no current system for archiving these data, except by individual programs or organizations; therefore much of the data is not available for review. There were plans to address this issue at the Council of Managers of National Antarctic Programs (COMNAP) at the planning meeting for the International Polar Year of 2007-2008.9 Unfortunately, because of funding issues, this has not been done.33
Even from these broad statistics, some figures emerge that may be useful cognitive anchors. There were 16 fatalities from 1947 to 1999 in the Australian Antarctic Program, but only 1 fatality in the past decade. Among 3500 scientists and support personnel (2000 person-years), there were 4 medical deaths, 2 myocardial infarctions, 1 case of appendicitis, 1 perforated gastric ulcer, and 1 cerebral hemorrhage. The remainder of the events were accidents involving falls, head injuries, hypothermia, drowning, crush injury, and burns.65,67
There have been 60 deaths in the U.S. Antarctic Program since 1946.1,69 These can be ranked by cause: aviation, 61%; vehicles, 11%; ships, 7%; recreational, 7%; station/industrial, 5%; field activities, 5%; and other, 4%.69 Although it is difficult to adhere to standard occupational safety practices when in a remote location, new guidelines and serious efforts in some of the programs have led to improved worker and participant safety.
A review of data for the Australian National Antarctic Research Expedition (ANARE) 2002-2003 season listed the following reasons for medical consultation: medical (e.g., upper respiratory, GI), 39%; injuries (sprains, strains, dermatologic, lacerations, fractures), 27%; follow-up visits, 24%; and preventive (immunizations, midyear examinations, wellness programs), 10%.17 For the 2004-2005 season, Antarctica New Zealand (ANZ) reported the following: musculoskeletal, 42%; medical (e.g., upper respiratory infections, GI), 22%; other injuries, 20%; dermatologic, 15%; and preventive, dental, and other, 8%.99 Usually, most visits are related to injuries, and the next most frequent medical clinic visits are attributable to upper respiratory infections. Environmental problems include dry skin and fissures, particularly on fingertips as a result of cold and very dry conditions. Cyanoacrylate glue hastens healing of disabling fingertip and heel fissures.7 Cold-induced urticaria, frostnip, and frostbite are frequently underreported, except for moderate to severe cases. Small nasal bleeds occur frequently, but they rarely require treatment beyond instruction to use petrolatum or antibiotic/antiseptic ointment once or twice a day to protect the delicate nasal epithelium, which easily becomes dehydrated or can suffer frostnip. Although the bulk of care is limited to routine visits, the pathologic conditions encountered even among this carefully screened population have included myocardial infarctions, massive GI bleeds, unreported Crohn’s disease, bowel obstructions, acute cholelithiasis with pancreatitis, pulmonary emboli, massive head injuries, fractures, crush injuries, newly diagnosed schizophrenia, and cancer.
Fire Safety
Elaborate predeployment training, frequent on-site drills, and keen awareness of potential fire hazards have correlated with a satisfactory fire safety record to date, but this good fortune cannot be taken for granted. One of the most life-threatening events was the explosion and fire at Vostok in 1982, leaving the station basically without power or adequate heat. Only one person died, however there were several injuries, and the winter crew had to endure 8 months without a power plant to supply heat.103 In 2001, the BAS Rothera Station lost its new Bonner Lab building when an electrical short started a fire. No one was injured, but with 50- to 70-knot winds, little could be done to save the station.11 Although fire-suppression systems are built into the newer buildings, a historic A-frame building at New Zealand’s Scott Base burned down in May 2009 and, much more seriously, a two-story building at Russia’s Progress Station burned down in October 2008, killing one person and seriously injuring two others. Because the building contained their radio equipment, they could not contact the outside world for 4 days after the event. In Antarctica, fire is an ever-present threat.
Tourist Safety
Polar regions are imbued with a sense of the exotic, conjuring up “images of hardship, personal valor, danger, adventure, and of course, the hero.”111 As transportation increasingly opens up previously inaccessible areas, this image attracts growing tourist traffic and, with it, hot debate from both legal and environmental viewpoints. The essential medicolegal issue is the extent of governmental organizations’ responsibility for medical care of participants in nongovernmental activities, whether scientific, political, or commercial. Although this discussion started much earlier, it is still ongoing.77 When a tourist group requires aid beyond its own capabilities, whose responsibility is it? To what extent should a research station with limited medical supplies be required to divert some of those supplies to an individual who presumably bears responsibility for planning his or her own medical coverage? By default, stations provide what assistance they can, although they often try to bill tourist companies and their insurance agencies for costs involved in patient treatment or transport. The Antarctic Treaty Consultative Meeting XXXI provided attendees with a list of guidelines recommended before trips to Antarctica, including travel insurance, contingency plans and other necessary equipment.3
Air Safety
As in the Arctic, reliance on aircraft for transportation has highlighted the critical importance of air safety. The worst Antarctic air accident was the crash of an Air New Zealand tourist “flightseeing” DC-10 on Mt Erebus in November 1979.83 This accident killed all 257 people aboard and temporarily ended such flights, although IAATO records indicate that overflights are now happening with new guidelines in place. There have been 35 air-related fatalities in the U.S. Antarctic Program since 1946 from crashes related to either fixed-wing or rotor aircraft.69,111 A ski-equipped LC-130 Hercules crashed at the remote D-59 camp in 1971 (Figure 9-7). Fortunately, none of the 10 crew members aboard was injured, but during a salvage operation in 1987, another LC-130 bringing supplies to D-59 crashed nearby, killing two and injuring nine. More recently, a helicopter crash occurred in the dry valleys; both the pilot and passenger were seriously injured. After a weather delay, they were extricated and evacuated to New Zealand for definitive care.17,81 The review of literature for air crashes in Antarctica is exhaustive. With better weather prediction and increased safety standards, the accident profile is improving.
Psychosocial Health Problems
As the U.S. Polar Manual explained in 1965, “No psychiatric case ever got better in the cold.”43 For many, polar living arrangements and psychosocial issues may be more important than the strictly medical or environmental factors. Psychiatric problems are mentioned even in reports of early expeditions, and almost any participant in expeditions will recognize Thor Heyerdahl’s observation: “The most insidious danger on any expedition where men have to rub shoulders for weeks is a mental sickness that might be called ‘expedition fever’—a psychological condition that makes even the most peaceful person irritable, angry, furious, absolutely desperate because his perceptive capacity gradually shrinks until he sees only his companions’ faults while their good qualities are no longer recorded by his grey matter.”121
Most psychological problems, primarily sleep disturbances, are minor and temporary. Many disturbances are more related to the social environment than to the physical environment.89,108 Appropriate lighting or changes in photo periodicity (the duration of daylight and darkness in a 24-hour period) help improve mood and sleep.91,129 In addition to appropriate exercise facilities, opportunities for quality mental stimulation and frequent contact with friends and family via the Internet and telephone can help maintain stability. Except for insomnia, which is perhaps endemic, the incidence of psychiatric problems is lower than expected in the overall population.
Many nations use formal and informal psychological screening, especially for participants planning to winter over in Antarctica. How well the screens function is debatable. A British study showed that an extensive psychological screening examination weeded out many participants with problems with “defensive-hostility” and “emotion-focused coping.” Simple interviews did not identify these problems.34
Alcohol Abuse
Adjustment to psychosocial stresses in polar communities depends on a complex array of sociocultural factors. One coping mechanism is alcohol use. As in many isolated communities at high latitudes, alcohol use can disrupt or lubricate social interactions. In the U.S. Antarctic Program, summer support-staff members are not infrequently terminated for alcohol abuse, and both summer and winter-over staff are occasionally prohibited from purchasing alcohol. In some instances, interventions with group support are found to be very effective. At many Antarctic stations, alcohol is easily available and may be subsidized. In some stations, rations can be excessive or nonexistent. Observations are that at least 50% of recreational injuries are alcohol related. Recommendations have called for routine monitoring of alcohol levels of anyone involved in an accident111 or even prohibition of alcohol at Antarctic stations. However, as with prohibition in other countries, this might create more problems than it might solve. Judicious use of monitoring can help identify persons who may need intervention before an accident happens.
Psychoneuroimmunology
Psychological stress at research stations may arise from several sources. One is the environment itself; environmental severity has been found to be an independent predictor of hostility and anxiety after wintering over.90 Perhaps more important is the perception of the environment. Newcomers to the South Pole station are usually observed wearing a full 12-kg (26.5-lb) polar outfit at −20° C (−4° F) for several weeks after arrival. By midwinter, the same individuals think little of walking short distances in only workout shorts and a T-shirt at −60° (−76° F).
Stress can also result from disjunction between a person’s original motivation for joining the program and the realities of life in the station—that is, the sociocultural environment. This may be the greatest determinant of difficulties.90 Studies suggest that people who go to Antarctic stations to seek thrills or to challenge themselves often have more difficulty sustaining their motivation and performance than those who go to accomplish a scientific mission or even those primarily motivated to earn money. In general, older individuals who are somewhat introverted are able to set work goals and work toward them, and persons who have broadly defined hobby interests seem to cope better with the social isolation and dynamics of wintering over. One study found that members with low social coherence reported significantly more depression, anxiety, and anger than did individuals belonging to expeditions with high social cohesion.88,130
Small-Group Dynamics
Social isolation is an important factor in polar communities, although this isolation has been lessened by modern communications and transportation. A number of studies have drawn parallels between group processes in polar stations and those in other isolated and confined environments, such as submarines or in space. As space travel becomes a reality, studies on group selection, leadership style, and interaction between the isolated group and headquarters take on urgency.35,63,93,131 Collaborative efforts are being made between many stations and space agencies, in particular the European Space Agency (ESA) and the NASA program.108
Cross-cultural and cross-gender issues by research groups are currently being studied at the international station, Concordia, particularly as an analog for long-distance space missions. Whereas in some areas cross-gender differences increase difficulties, in others they are beneficial. Further studies on rigorous selection criteria and training before deployment will avoid the problems that have occurred with sexual harassment. It is felt that the positive effect of better communication, less rude behavior, and increased supportive environment outweigh the negative effect. Other stations have already gone through this process.63,108
Winter-Over Syndrome
Stressors such as those mentioned previously can result in what has been termed the winter-over syndrome. The historically oft-mentioned “Big Eye” or “20-foot stare in a 10-foot room” seems to be less common now, perhaps because the stations are increasingly comfortable and have stimulating environments. But the constellation of depression, hostility, sleep disturbances, and impaired cognition still seems to be both common and underreported.94,95,105 The winter-over syndrome is not a static condition but a time- and individual-dependent process. At the South Pole research station, for example, winter-over staff characteristically report a recognizable pattern of fluctuating activity and mood. There is often a mixture of relief, pride, and fearful anticipation as the last LC-130 flight departs in mid-February, followed by a period of frenetic activity to beat inventory deadlines, file resupply orders, launch projects, and prepare the station for winter. As work and recreation routines develop, mood generally drops with the setting sun. A rise in mood occurs toward sunrise but is followed with anticipation, increase in anxiety, and stress as the time of the arrival of the first return flight draws near. Studies at the Australian stations of Mawson and Macquarie Island suggest that the influx of new staff at station opening may actually be associated with increased depression.
Seasonal Affective Disorder
A probable contributor to and confounder of the winter-over syndrome is the apparently fairly consistent exacerbation of stress and depression under conditions of winter or night, leading to seasonal affective disorder (SAD). Subsyndromal SAD (S-SAD) is perhaps a better definition of what is experienced by many who winter over in the dark latitudes.92 Further studies indicate that S-SAD may be part of the T3 syndrome.95 Correlations with melatonin levels have been shown to be associated with the frequent sleep disturbances at higher latitudes, both with advanced or delayed phases, and with increased latency.5,129 In some studies, melatonin’s chronobiotic properties are used to resynchronize the individual’s sleep.5 Other studies have demonstrated the effectiveness of light therapy in helping resynchronize the body.129 SAD may be no more prevalent in Antarctica than at lower latitudes; some of the depressive symptoms may well be the result of social isolation or related to seasonal changes.96
Beneficial Effects of Isolation
An interesting point is that isolation may have positive as well as negative effects.96 Isolation is not synonymous with loneliness and depression, as Amundsen reported from his sojourn at Framheim. In fact, a subset of “professional isolates” may actually prefer polar stations to “normal” society.120 In some cases, reentry and adaptation to the rest of the world can take up to 6 months. The positive effect of isolation may be reflected in a study of somatic complaints, published in 1992, that compared Navy volunteers who qualified for winter duty in Antarctica and wintered over, with those who were physically qualified but were assigned elsewhere because of the limited number of winter assignments. Those who spent the winter in Antarctica had fewer illnesses and hospitalizations after the winter-over period. These volunteers were followed an average of 5.4 years after the winter period. It was also noted that the complex psychophysiologic symptoms experienced during the winter-over period were probably adaptive coping mechanisms. Coping led to a process of negotiation leading to compromise, which frequently led to finding new strategies or resources that could be used for subsequent stressful experiences. Newer studies confirm the salutogenic effect of completing a long-term contract in an isolated environment.88,96
Screening and Selection
Based on the preceding findings, several attempts have been made to refine the selection and screening processes for successful polar and space sojourners. It is not surprising that previous successful polar experience seems to be among the best predictors of subsequent high performance. Biographic data, peer ratings, psychometric testing, and interviews all seem helpful in selection, although each has weaknesses and inconsistencies. Recent studies have suggested that team climate significantly related to the perception of good leadership.110 More research needs to be done to explore the characteristics and behaviors that constitute effective leadership, in order to guide selection of crew and leader.14,110 Early studies led to the tripartite “ability, stability, compatibility” criteria for successful participation in the Antarctic programs.34 This simple but useful scheme recognizes that technical skill, emotional equilibrium, and interpersonal skills all play important roles in an individual’s performance and internal satisfaction. It would be desirable to improve measurement and predictive usefulness of these factors; such studies remain at the active frontier of Antarctic research.34
Overview and Future Developments
Fourth World Medical Decision Making
Polar medical lore is replete with stories like that of the physician of the sixth Soviet Antarctic Expedition at Novolazarevskaya Station, who performed an appendectomy on himself in April 1961 with assistance from the station mechanic.107 Although the basic principles of emergency medicine, epidemiology, occupational health, psychology, and other disciplines still apply in polar settings, the spectrum of health problems and some important aspects of their management are undoubtedly skewed. However, with newer and improved technical communication modalities and transportation, delivery of advanced care in the polar latitudes has improved, and many lessons learned in Antarctica are applicable to space exploration and settlement.
Fourth World medicine requires distillation of medical practice into a compact yet comprehensive package that is sufficiently robust to travel well. Novel constraints and the inherently unpredictable nature of a hostile environment further stretch the usual, already-tentative rules and thresholds of medical decision making. Perhaps to a greater extent than in most settings, prevention and preparation are paramount in polar medicine. As might be imagined, cold and its effects on both humans and equipment exacerbate the risks from even minor mishaps, altitude impairs tissue oxygenation and wound healing, and bulky clothing restricts dexterity and vision. Isolation from medical facilities exerts a multiplier effect on these risks. Victim extrication and resuscitation that would be routine in most urban or suburban settings present overwhelming challenges in polar settings.102
With lives at stake, arguments have been made for planning for worst-case scenarios rather than only for likely situations.111 On the other hand, a realistic balance point on the cost-versus-utility curve, based on estimated risks, must be set for each situation. Given existing fiscal and logistic constraints, preventive measures should take priority over higher-cost options.8
A recurrent medical issue in polar stations involves contingency planning and the optimal level of inventory. This question applies equally to drugs, equipment, training, and personnel and is faced immediately by any incoming physician. “Just in time” principles of inventory management are not likely to be appropriate.8,111
Combined improvements in communications systems, the Internet, and the powerful tool of telemedicine with its many modalities have transformed what was once an extremely isolated practice of medicine. The advantages of rapid access to organized databases and remote consultations for radiology and other specialties via video are realities. Telemedicine is in place and functioning in many northern Arctic regions. The Australian, British, Italian, and United States Antarctic Programs and many others have been using it successfully for a number of years.35,56,64,104 Physiologic, psychological, and occupational health data can be monitored or retrieved, ultimately linking geography and information flow and allowing nearly real-time consultation and guidance from multiple specialists. These promising tools are real solutions to the problems of isolation faced by earlier physicians.
Medical Aspects of Arctic Racing
The Medical Team
Before the start of the race, and after consultation with local hospitals, an emergency evacuation plan is written for extrication of racers to the most appropriate trauma/emergency medical facility, depending on the type of injury. At each checkpoint, a physician is available to provide treatment and consultation to the racers. A more experienced polar physician forms part of the mobile medical team (contacted via satellite pager), which also includes a navigator and a local Inuit guide/mechanic. This team is placed strategically on the ice for the duration of the race. It responds to any medical event either by snowmobile or on foot, with full air evacuation support on standby at all times. The race physicians carry an extensive range of equipment and drugs (Box 9-1) designed to handle any eventuality in this environment. This kit is refined annually after each postrace injury debriefing.
Prerace Selection and Training
Competitors for the race range in ability from experienced and very well trained Arctic travelers to complete novices. Ages so far have ranged from 20 to 65 years with a mix of two-thirds men and one-third women, totaling 80 racers in 7 years. All are offered the same training program (Box 9-2). If required, experts are available for extra tutoring specifically tailored to individual needs.
Team Medical Training
Each team is required to carry a prepacked medical bag. The bags and their contents are identical for all teams. Constructed of lightweight yet tough material, they have two outer pockets and internal color-coded pouches, whose contents are listed in Box 9-3. Each bag contains a color-coded contents list with instructions for use. This makes giving advice over the satellite telephone much easier, reducing the likelihood of error. Each race physician knows which drugs are in which color-coded pouch and so can instruct racers accordingly. The external pouches contain emergency dressings and wound and blister treatments.
BOX 9-3 Polar Challenge Medical Advice Sheet 2005
Suspected fractures or serious trauma or illness—tent up and call for help
Painkillers
Antibiotics
Gut
Skin
Arctic Racing Injuries Encountered to Date
Frostnip in varying degrees has been seen in most competitors during the race, regardless of their previous cold-weather experience. It has affected mainly the extremities, such as the nose, ears, and fingertips (Figure 9-8). All cases were treated by rewarming and diligent future protection. The number of frostnip injuries decreased after a team buddy system was instituted, which led to rapid prediction of impending injury and timely avoidance.
Frostbite was seen in six competitors, five of whom had finger injuries (Figure 9-9, online). All the fingers made a complete recovery largely as a result of early detection and rapid evacuation of affected competitors from the race to a rewarming and treatment facility.
One case of fingertip frostbite was caused by a fuel spill onto the fingertips, which caused rapid freezing and subsequent injury. This competitor was a highly experienced Arctic traveler and was therefore allowed to continue, subsequently making a full recovery during the race (Figure 9-10).
The final case of frostbite was more unusual, affecting a competitor’s penis (Figure 9-11). After urinating, he forgot to close the zipper correctly on his wind suit. After walking into a headwind with a windchill factor of −80° C (−112° F) for an hour, he discovered his foreskin to be frozen. Rapid evacuation prevented further damage and, after a circumcision on his return to the United Kingdom, he made a complete recovery both in sensation and function. During the event, this competitor could easily have gone into urinary retention and would have been catheterized accordingly, making it essential to carry such equipment in the physician’s medical kit.
Snowblindness was seen in 4% of racers (Figure 9-12, A). Diagnosis in the field was achieved with the aid of fluorescein stain, and the eyes were treated with topical local anesthetics, antibiotics, oral analgesia, rest, and eye patches (Figure 9-12, B). All affected racers went on to complete the race.
All the female racers (and none of the male racers) developed a cold-induced urticarial rash isolated to the anterior surfaces of the thighs (Figure 9-13). This was treated with oral antihistamines and topical corticosteroids but was difficult to cure, taking days to weeks to resolve in a warmer environment after the race. Steps are being taken to design clothing for female competitors to prevent this from happening in the future.
Trench foot was reported in two competitors at a late stage in the race (Figure 9-14). Both were treated after completion of the race. Diligent foot care during the race would have helped prevent this injury.
Fatigue and hypothermia affected all racers to varying degrees. Despite consuming 7000 cal and drinking 4 L per day, most competitors are likely to lose 10% of their body weight. Training is given to all the teams on how to treat a teammate with severe fatigue and hypothermia. Only two competitors have withdrawn for such reasons (Figure 9-15, online).
The Use of Frozen Medications
The medical literature is relatively sparse on this topic.31 One of the authors has rewarmed frozen fluorescein stain, oxybuprocaine hydrochloride 0.4%, ophthalmic local anesthetic, corticosteroid creams, antifungal creams, inhaled salbutamol, and IV hydrocortisone, all of which worked normally after rewarming. All forms of tablet medications warmed from frozen have also been fine after rewarming. A study from the BAS found that most medications remained stable, even after multiple freeze-thaw cycles. The exception was hydrocortisone cream, although the investigator also recommended against subjecting eye medications to temperature extremes. Medical devices, such as IV cannulas, worked normally after rewarming, as did all forms of tape and dressings. Frozen IV fluids expanded when frozen, perforated the bags, and thus leaked when rewarmed.
Acknowledgments
Special thanks to Kenneth H Willer, MLS, Manager—Library Services, Samaritan Health Services, Corvallis, Ore, kwiller@samhealth.org.

FIGURE AOO 9-1 The McMurdo Station medical facility—examination room 1.
(Courtesy Kenneth V. Iserson.)
1 Adams G: Personal communication, July 2005.
2 Adler A. Arctic first aid. N Engl J Med. 1992;326:351.
3 Antarctic Treaty Special Consultative Meeting XXXI, annex 1, Guidelines on contingency planning, insurance and other matters for tourist and other non-governmental activities in the Antarctic treaty area. http://www.ats.aq/documents/recatt/Att225_e.pdf, 2008.
4 [Antarctic Treaty Summit, November 30—December 03 2009, Smithsonian Institution, http://www.atsummit50.aq/treaty/members.php.
5 Arendt J, Skeene DJ. Melatonin as a chronobiotic. Sleep Med Rev. 2005;9:25.
6 Ayotte P, Dewailly E, Bruneau S, et al. Arctic air pollution and human health: What effects should be expected? Sci Total Environ. 1995;529:160.
7 Ayton J. Polar hands: Spontaneous skin fissures closed with cyanoacrylate (Histoacryl Blue) tissue adhesive in Antarctica. Artic Med Res. 1993;52:126.
8 Ayton J: Report on Australian Antarctic human biology and medicine research. Meeting of SCAR Life Sciences Expert Group on Human Biology and Medicine: SCAR XVIII, Bremen, Germany, 2004 Personal correspondence.
9 Bachelard C: TAAF medicine. Personal communication. July 2005.
10 Ballschmite K, Hackenberg R, Jarman WM, et al. Man-made chemicals found in remote areas of the world: The experimental definition for POPs. Environ Sci Pollut Res Int. 2002;9:274.
11 BBC News. UK to rebuild Antarctic Lab. http://news.bbc.co.uk/2/hi/science/nature/1715922.stm, Dec 18, 2001.
12 Berner J. Health status of the Arctic residents: AMAP assessment 2002: Human health in the Arctic. http://www.amap.no.
13 Bhattacharyya M, Pal MS, Sharma YK, et al. Changes in sleep patterns during prolonged stays in Antarctica. Int J Biometeorol. 2008;52:869.
14 Bishop SL. Evaluating teams in extreme environments: From issue to answers. Aviat Space Environ Med. 2004;75:1.
15 Bjerregaard P, Young TK, Dewailly E, et al. Indigenous health in the Arctic: An overview of the circumpolar Inuit population. Scand J Public Health. 2004;32:390.
16 Carlisle B: Personal knowledge, McMurdo 2001.
17 Carlisle B: Turnover report McMurdo, 2002-2003.
18 . CIA World Fact Book. update May 10, 2010 https://www.cia.gov/library/publications/the-world-factbook/geos/ay.html
19 CNN. Amundsen-Scott Station, Antarctica. http://www.southpolestation.com/news/medevac.html, April 25, 2001.
20 Cockell CS, Sherer K, Horneck G, et al. Exposure of Arctic field scientist to ultraviolet radiation evaluated using personal dosimeters. Photochem Photobiol. 2001;74:570.
21 Conway G, Lincoln J, Jorgensen S, et al. Preventing deaths in Alaska’s commercial fishing industry. Int J Circumpolar Health. 1998;57:503.
22 Council of Managers of National Antarctic Programs Antarctic Facilities http://www.comnap.aq/facilities
23 Curry C. Death in Antarctica [letter]. Med J Aust. 2002;176:451.
24 Do NV, Mino L, Merriam GR, et al. Elevation in serum thyroglobulin during prolonged Antarctic residence: effect of thyroxine supplement in polar 3.5.3′- triiodothyronine syndrome. Int J Circumpolar Health. 1998;57:388.
25 Dyck R, Osgood N, Lin T, et al. Epidemiology of diabetes mellitus among First Nations and non-First Nations Adults. CMAJ. 2010;182:249.
26 Feldman J: Personal communication, Palmer Station, January 10, 2010.
27 Fenge T. Environmental clean-up and sustainable development in the circumpolar. Arctic. Northern Perspectives 21, 1993-94, http://www.carc.org/pubs/v21no4/cleanup.htm.
28 Fenge T, Watt S, Crump J, et al. Persistent organic pollutants: Are we close to a solution?. Indigenous peoples and global POPs. Northern Perspectives 26, http://www.carc.org/pubs/fall2000/Northern_Perspectives_26.pdf, 2000.
29 Francis G, Bishop L, Luke C, et al. Sleep during the Antarctic winter: Preliminary observation on changing the spectral composition of artificial light. J Sleep Res. 2008;17:354.
30 Francis JL, Gleeson M, Lugg DJ, et al. Trends in mucosal immunity in Antarctica during six Australian winter expeditions. Immunol Cell Biol. 2002;80:382.
31 Freitas CD, Symon L. Bioclimatic index of human survival times in the Antarctic. Polar Rec. 1987;23:651.
32 Gander PH, MacDonald JA, Montgomery JC, et al. Adaptation of sleep and circadian rhythms to Antarctic summer: A question of zeitgeber strength. Aviat Space Environ Med. 1991;62:1019.
33 Grant IC: Personal communication, March 2011.
34 Grant I, Ericksen HR, Marquis P, et al. Psychological selection of Antarctic personnel: The “SOAP” instrument. Aviat Space Env Med. 2007;78:793.
35 Grant IC. Telemedicine in the British Antarctic Survey. Int J Circumpolar Health. 2004;63:356.
36 Haggarty JM, Cernovsky Z, Husni M, et al. Seasonal affective disorder in an Arctic community. Acta Psychiatr Scand. 2002;105:378.
37 Hall S. The Fourth World: The heritage of the Arctic and its destruction. New York: Vintage Books; 1988.
38 Hansen JC. Environmental contaminants and human health in the Arctic. Toxicol Lett. 2000;119:112.
39 Hansen JC, Gilman AP. Exposure of Arctic population to methylmercury from consumption of marine food: An updated risk-benefit assessment. Int J Circumpolar Health. 2005;64:121.
40 Hansen V, Jacobsen B, Husby R. Mental distress during winter: An epidemiologic study of the 7759 adults north of the Arctic Circle. Acta Psychiatr Scand. 1991;84:137.
41 Harinath K, Malhotra AS, Pal K, et al. Autonomic nervous system and adrenal response to cold in man at Antarctica. Wilderness Environ Med. 2005;16:81.
42 Hassi J. Environmental health risks of the Arctic assessed. Int J Circumpolar Health. 2002;61:289.
43 Hedblom EE. Polar manual, ed 4. Bethesda, Md: Naval Medical School; 1965.
44 Homler I. Problems with cold work: Proceedings from an international symposium. Stockholm, Arbetslivsinstitutet, 1997, pp 96-98 http://gupea.ub.gu.se/dspace/bitstream/2077/4185/1/ah1998_18.pdf
45 Horwitz S. Jump on the Pole. http://airsports.fai.org/may98/may9804.html, May 1998.
46 Hudson S. Risk assessments and casualty evacuation. Expedition Med http://www.expeditionmedicine.co.uk/index.php/advice/resource/r-0014.html
47 Hughes KA, Blenkharn N. A simple method to reduce discharge of sewage microorganism from Antarctic research station. Mar Pollut Bull. 2003;46:353.
48 Inspections under Article VII of the Antarctic Treaty. http://www.state.gov/documents/organization/15274.pdf.
49 International Association of Antarctic Tour Operators. Tourism overview. http://www.iaato.org/tourism_stats.html.
50 International Association of Antarctic Tour Operators. Tourism summary 2003-2004. http://www.iaato.org/tourism_stats.html.
51 Iserson KV: Personal observations McMurdo Station 2009-2010.
52 Jacobs M, Richardson JI, editors. Arctic life: Challenge to survive. Pittsburgh, Pa: Carnegie Institute, 1983.
53 Jenkins AL, Gyorkos TW, Culman KN, et al. An overview of factors influencing the health of Canadian Inuit infants. Int J Circumpolar Health. 2003;62:17.
54 Johnson D, Gamble W. Trauma in the Arctic: An incident report. J Trauma. 1991;31:1340.
55 Juliano S, Ayton J. Antarctic expeditioners assist bone loss study. Australian Antarctic Magazine. 2005;8:29.
56 Karasek M. Melatonin, human aging, and age-related diseases. Exp Gerontol. 2004;39:1723.
57 Kennaway D, Van Dorp CF. Free-running rhythms of melatonin, cortisol, electrolytes and sleep in humans in Antarctica. Am J Physiol. 1991;260:R1137.
58 Korhonen M. Alcohol problems and approaches: Theories, evidence and northern practice. Med J Aust. 2004;180:32.
59 Korhonen M. Helping Inuit clients: Cultural relevance and effective counseling. Int J Circumpolar Health. 2004;63:135.
60 Krummel EM. The Circumpolar Inuit Health Summit: A summary. Int J Circumpolar Health. 2009;68:509.
61 Lansing A. Endurance: Shackleton’s incredible voyage. New York: Carroll & Graff; 1986.
62 Lehti V, Niemelä S, Hoven C, et al. Mental health, substance use and suicidal behaviour among young indigenous people in the Arctic: a systematic review. Soc Sci Med. 2009;69:1194.
63 Leon GR, Sandoval GM. Women and couples in isolated extreme environments: Applications for long duration missions. Acta Astronaut. 2003;53:259.
64 Levine M, Duffy L, Moore DC, et al. Acclimation of a non-indigenous sub-Arctic population: Seasonal variation in thyroid function in interior Alaska. Comp Biochem Physiol A Physiol. 1995;111:209.
65 Lugg DJ: Personal communication, 1999.
66 Lugg DJ. Antarctic medicine. JAMA. 2000;283:2082.
67 Lugg DJ, Gormerly P, King H. Accidents on Australian Antarctic expeditions. Polar Rec. 1999;23:720.
68 Macdonald RW, Bewers JM. Contaminants in the Arctic marine environment: Priorities for protection. I CES J of Marine Science. 1996;53:537.
69 Mahar H: Personal communication, January 1999.
70 Marriott BM, Carlson SJ, editors. Committee on Military Nutrition Research: Nutrition needs in cold and high-altitude environments: Applications for the military personnel in field operations. National Academy Press, Washington, DC, 1996;198-200.
71 Matheson B, Walker KZ, Taylor DM, et al. Effect on serum lipids of monounsaturated oil and margarine in the diet of an Antarctic expedition. Am J Clin Nutr. 1996;63:993.
72 Mawson D. Home of the blizzard. New York: St. Martin’s Press; 2000.
73 Meinander H, Anttonen H, Bartels V, et al. Manikin measurements versus wear trial of cold protective clothing (SubZero Project). Eur J Appl Physiol. 2004;92:619.
74 Meyer-Rochow VB. Coming to grips with a slippery issue: Human waste disposal in cold climates. Int J Circumpolar Health. 1999;58:57.
75 Midwinter M, Arendt J. Adaptation of the melatonin rhythm in human subjects following nite shift work in Antarctica. Neurosci Lett. 1991;122:195.
76 Montgomery-Andersen R. Adolescent mothers: A challenge for First Nations. Int J Circumpolar Health. 2004;63:274.
77 Murray C, Jabour J. Independent expeditions and Antarctic tourism policy. Polar Rec. 2004;40:309.
78 Nagaya Y, Shiozaki M, Seto Y. Radioactive contamination of the Indo-Antarctic Ocean water in early parts of 1961 and 1962. J Radiat Res (Jap). 1964;5:206.
79 Natani K, Shurley JT, Pierce CM, et al. Long-term changes in sleep patterns in men on the South Polar Plateau. Arch Intern Med. 1970;125:655.
80 National Institute on Polar Research: Proceedings of the International Symposium: Asian collaboration in IPY 2007-2008, Tokyo, Japan.
81 National Science Foundation. Helicopter crash [news release]. Antarctic Sun. January 19, 2003, http://antarcticsun.usap.gov/oldissues2002-2003/Sun011903/crash.html.
82 Neri M, De Jongh R. Medical and trauma evacuations. Clin Occup Environ Med. 2004;4:85.
83 New Zealand disasters, aircraft accident: DC 10 ZK-NXP flight 901. http://christchurchcitylibraries.com/Kids/NZDisasters/Erebus.asp.
84 NIOSH Safety & Health Topic. Commercial aviation in Alaska (1990-2008). http://www.cdc.gov/niosh/topics/aviation/.
85 [Occupational Safety and Health Report. In Healthy Alaskans 2010, vol 1, State of Alaska, Health & Social Services, http://www.hss.state.ak.us/dph/targets/ha2010/PDFs/10_Occupational.pdf.
86 Oliveri B, Zeni S, Lorenzetti MP, et al. Effect of one year residence in Antarctica on bone mineral metabolism and body composition. Eur J Clin Nutr. 1999;53:88.
87 Pääkkönen T, Leppäluoto J, Mäkinen T, et al. Seasonal levels of melatonin, thyroid hormones, mood, and cognition near the Arctic Circle. Aviat Space Environ Med. 2008;79:695.
88 Palinkas LA. Going to extremes: the cultural context of stress, illness and coping in Antarctica. Soc Sci Med. 1992;35:651.
89 Palinkas LA. The psychology of isolated and confined environments: Understanding human behaviour in Antarctica. Am Psychol. 2003;58:353.
90 Palinkas LA, Glogower F, Dembert M, et al. Incidence of psychiatric disorders after extended residence in Antarctica. Int J Circumpolar Health. 2004;63:157.
91 Palinkas LA, Houseal M, Miller C, et al. Sleep and mood during a winter in antarctica. Int J Circumpolar Health. 2000;59:63.
92 Palinkas LA, Houseal M, Rosenthal NE. Subsyndromal seasonal affective disorder in Antarctica. J Nerv Ment Dis. 1996;184:530.
93 Palinkas LA, Johnson JC, Boster JS, et al. Cross-cultural differences in psychosocial adaptation to isolated and confined environments. Aviat Space Environ Med. 2004;75:973.
94 Palinkas LA, Mäkinen TM, Pääkkönen T, et al. Influence of seasonally adjusted exposure to cold and darkness on cognitive performance in circumpolar residents. Scand J Psychol. 2005;46:239.
95 Palinkas LA, Reed HC, Reedy KR, et al. Circannual pattern of hypothalamic-pituitary-thyroid (HPT) function and mood during extended Antarctic residence. Psychoneruroendocrinology. 2001;26:421.
96 Palinkas LA, Suedfeld P. Psychological effects of Polar expeditions. Lancet. 2008;371:153.
97 Parkinson A, Muchmore H, Scott E. Rhinovirus respiratory tract infections during isolation at South Pole Station. Antarctic J US. 1984;19:186.
98 Parkinson AJ. The international polar year 2007-2008: The Arctic human health legacy. I. 2007;49:43.
99 Pascoe J: New Zealand Antarctic Programme. Report to SCAR, Sofia, Bulgaria. July 12-15 2005; Human biology and medicine in the New Zealand Antarctic Programme. Personal communication.
100 Pause B. Development of a new cold protective clothing with phase change material: Problems with cold work. http://gupea.ub.gu.se/dspace/bitstream/2077/4185/1/ah1998_18.pdf.
101 Pitson GA, Lugg DJ, Roy CR. Effect of seasonal ultraviolet radiation fluctuations on vitamin D homeostasis during an Antarctic expedition. Eur J Appl Physiol Occup Physiol. 1996;72:231.
102 Plowright R. Crevasse fall in the Antarctic: A patient’s perspective. Med J Aust. 2000;13:576.
103 Pravda. 45th birthday of Russia’s Antarctic Station Vostok, April 13, 1982 http://english.pravda.ru/russia/19216-0
104 Raimer GG, Hermstein SM, Angelo J, et al. Telemedicine at the South Pole. Telemed e-Health. 2003;9:67.
105 Reed HL, Reedy KR, Palinkas LA, et al. Impairment in cognitive and exercise performance during prolonged Antarctic residence: Effect of thyroxine supplementation in the polar triiodothyronine syndrome. J Clin Endocrinol Metab. 2001;86:110.
106 Risikko T, Anttonen H. Use of personal heaters in cold work. Problems with cold work: Proceedings from an international symposium,. Arbetslivsinstitutet, Stockholm, 1997;29-30, http://gupea.ub.gu.se/dspace/bitstream/2077/4185/1/ah1998_18.pdf.
107 Rogozov V, Bermel N. Auto-appendectomy in the Antarctic: Case report. BMJ. 2009;339:b4965.
108 Rosnet E, Jurion S, Bachelard C. Mixed-gender groups: Coping strategies and factors of psychological adaptation in a polar environment. Aviat Space Environ Med. 2004;75:C10.
109 Ross JK, Arendt J, Horne J, et al. Nightshift work in Antarctica: Sleep characteristics and bright light treatment. Physiol Behav. 1995;57:1169.
110 Schmidt LL, Wood J, Lugg DJ. Team climate at Antarctic Research Stations 1996-2000: Leadership matters. Aviat Space Environ Med. 2004;75:681.
111 Schweickart R, et al. Safety in Antarctica. Washington, DC: National Science Foundation; 1988.
112 Shephard RJ. Some consequences of polar stress: Data from a transpolar ship-trek. Arctic Med Res. 1991;50:25.
113 Smylie J. SOGC Policy Statement #100 2001: Guide for health professionals working with aboriginal peoples: Health issues affecting aboriginal peoples. J Obstet Gynaecol Can. 2000;22:1074.
114 Strand P. Radioactivity in the environment (including the Arctic and Antarctica): The International Conference in Nice, France, 2-6 October 2005. editor]. J Environ Radioact. 2007;96:1.
115 Strand P, Howard BJ, Aarkrog A, et al. Radioactive contamination in the Arctic: Sources, dose assessment and potential risks. J Environ Radioact. 2002;60:5.
116 Stroud MA, Jackson AA, Waterlow JC. Protein turnover rates of two human subjects during an unassisted crossing of Antarctica. Br J Nutr. 1996;76:165.
117 Stroud MA, Ritz P, Coward WA, et al. Energy expenditure using isotope-labelled water (2H218O), exercise performance, skeletal muscle enzyme activities and plasma biochemical parameters in humans during 95 days of endurance exercise with inadequate energy intake. J Appl Physiol Occup Physiol. 1997;76:243.
118 Sugden D. Arctic and Antarctic: A modern geographical synthesis. Totowa, NJ: Barnes & Noble Books; 1982.
119 Syme D. The circumpolar Inuit: Health of population in transition. BMJ. 1999;318:133.
120 Taylor A. Professional isolates in New Zealand’s Antarctic research programme. Int Rev Appl Psychol. 1969;18:135.
121 Taylor AJW. Antarctic psychology. New Zealand Department of Scientific and Industrial Research Bulletin. Science Information Publishing Centre, Wellington, NZ, 1987. 244:20
122 Tkachev A, Ramenskaya EB, Bojko JR. Dynamics of hormone and metabolic state in polar inhabitants depend on daylight duration. Arctic Med Res. 1991;50:152.
123 2009 Human health report, AMAP assessment 2009: Human health in the Arctic. 2009, Oslo, Norway. Arctic Monitoring and Assessment Programme (AMAP).
124 UNEP/GRID-Arendal. Population distribution in the circumpolar Arctic, by country (including indigenous population). Maps and Graphics Library http://www.maps.grida.no/go/graphic/population-distribution-in -the-cicumpolar-arctic-by-country-including-indigenous-population1, 2008.
125 United Nations Environment Programme Report. Global environment outlook 2000. chap 2: The state of the environment polar regions, http://www.grida.no/publications/other/geo2000/.
126 United Nations Environment Programme Report. Global environment outlook 2000. chap 2: The state of the environment—The Arctic http://www.grida.no/publications/other/geo2000/
127 Van Do N, Mino L, Merriam GR, et al. Elevation in serum thyroglobulin during prolonged Antarctic residence: Effect of thyroxine supplement in polar T3 syndrome. J Clin Endocrinol Metab. 2004;89:1529.
128 Varynen S. Ergonomic design of machinery for use in the cold: A review based on the literature and original research. Arctic Med Res. 1992;51:87.
129 Warman VL, Dijk DJ, Warman GR, et al. Phase advancing human circadian rhythms with short wavelength light. Neurosci Lett. 2003;15:37.
130 Wintrhereik M. The spread of HIV in Greenland: Heterosexual epidemic-risk or reality? A 10 year review of HIV transmission and preventive care. Ugesker Laeger. 1998;160:2851.
131 Wood J, Schmidt L, Lugg D, et al. Life, survival, and behavioral health in small closed communities: Studying isolated Antarctic groups. Aviat Space Environ Med. 2005;76:B89.
132 Yablokov AV, Nesterenko VB, Nesterenko AV. Consequences of the Chernobyl catastrophe for public health and the environment 23 years later. Ann N Y Acad Sci. 2009;1181:318.
133 Zerath E, Holy X, Gaud R, et al. Decreased serum levels of 1,25-(OH)2 vitamin D during 1 year sunlight deprivation in the Antarctic. Eur J Appl Physiol Occupat Physiol. 1999;79:141.