18 Poisoning
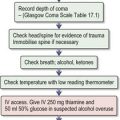
Care of the unconscious patient
Ventilatory support
Cardiovascular support
Other problems
Reduction of poison absorption
Gastric lavage
Single-dose activated charcoal
Increasing poison elimination
Urine alkalinization
Multiple-dose activated charcoal (MDAC)
Haemodialysis, haemodiafiltration and haemofiltration (p. 358)
Specific poisons
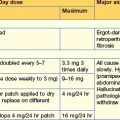
Specific management for each poison is set out below alphabetically. Antidotes are available for only a small number of poisons (Table 18.1) and dosage recommendations are given under each poison.
| Poison | Antidote |
|---|---|
| Anticoagulants (oral) | Vitamin K1 |
| Arsenic | DMSA* Dimercaprol (BAL) |
| Benzodiazepines | Flumazenil |
| β-adrenoceptor-blocking drugs | Atropine Glucagon |
| Carbon monoxide | Oxygen |
| Copper | DMPS† |
| Cyanide | Oxygen Dicobalt edetate Hydroxocobalamin Sodium nitrite Sodium thiosulphate |
| Diethylene glycol | Fomepizole, ethanol |
| Digoxin | Digoxin-specific antibody fragments |
| Ethylene glycol | Fomepizole, ethanol |
| Iron salts | Desferrioxamine (deferoxamine) |
| Lead (inorganic) | Sodium calcium edetate DMSA* |
| Methaemoglobinaemia | Methylthioninium chloride (methylene blue) |
| Methanol | Fomepizole, ethanol |
| Mercury (inorganic) | DMPS† |
| Nerve agents | Atropine Pralidoxime, obidoxime |
| Opioids | Naloxone |
| Organophosphorus insecticides | Atropine Pralidoxime, obidoxime |
| Paracetamol | Acetylcysteine |
| Thallium | Berlin (Prussian) blue |
* Dimercaptosuccinic acid (succimer).
† 2,3-dimercaptopropanesulfonate (unithiol).
Acetone
Clinical features
Treatment
Amfetamines
The N-methylated derivative, metamfetamine, is now used widely; the crystalline form of this salt is known as ‘crystal meth’ or ‘ice’. Ecstasy (MDMA) is discussed on page 675.
Clinical features
Treatment
Anticonvulsants
See carbamazepine (p. 671), gabapentin (p. 677), lamotrigine (p. 679), phenytoin (p. 688) and sodium valproate (p. 691).
Antidepressants
See selective serotonin reuptake inhibitors (p. 690), mirtazapine (p. 681), monoamine oxidase inhibitors (p. 682), tricyclic antidepressants (p. 692) and venlafaxine (p. 693).
Batteries
Treatment
Beta2-adrenoceptor agonists
Clinical features
Treatment
Beta-adrenoceptor-blocking drugs
Clinical features
Treatment
Benzodiazepines
Treatment
Calcium channel blockers
Clinical features
Treatment
Cannabis (marijuana)
Clinical features
Carbamazepine
Carbon monoxide
Clinical features
Treatment
Chloroquine
Cocaine
Clinical features
Treatment
Copper
Clinical features
Corrosive ingestions
Clinical features
Treatment
Cyanide
Cyanide reversibly inhibits cytochrome oxidase a3 so that cellular respiration ceases.
Clinical features
Treatment
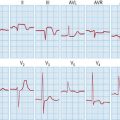
Digoxin
Toxicity occurring during chronic administration is common; acute poisoning is infrequent.
Clinical features
Treatment
Ecstasy (3,4-methylenedioxymethamfetamine; MDMA)
Clinical features
Ethanol
Clinical features
Treatment
Ethylene and diethylene glycols
Clinical features
Treatment
Gamma-hydroxybutyrate (GHB)
Clinical features
Household products
Iron
Clinical features
Treatment
Isopropanol
This is more toxic than ethanol and is the base for many hand washes.
Treatment
Lead
Clinical features
Treatment
Lithium
Clinical features
Mercury
Clinical features
Treatment
Methanol
This is found in windscreen washer fluid, antifreeze and duplicator fluid.
Clinical features
Mirtazapine
This is a 5HT2 and 5HT3 receptor agonist and a potent α2-adrenergic blocker.
Monoamine oxidase inhibitors
Clinical features
Neuroleptics and atypical neuroleptics
Clinical features
Treatment
Opiates and opioids
Treatment
Organophosphorus insecticides
These insecticides inhibit acetylcholinesterase, allowing accumulation of acetylcholine.
Clinical features
Paracetamol (acetaminophen)
Clinical features
Treatment
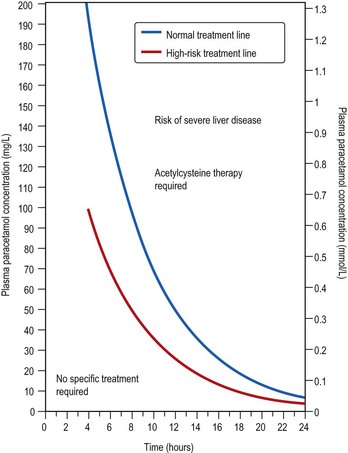
Fig. 18.1 Nomogram of paracetamol. For definition of ‘high risk’, see text.
(British National Formulary 2009, with permission.)
Box 18.1 Management of patients with paracetamol poisoning
≤ 8 hours after ingestion
8–15 hours after ingestion
15–36 hours after ingestion
Paraquat
Clinical features
Petroleum distillates
Clinical features
Treatment
Plant toxins
Yellow oleander (Thevetia peruviana)
• Treatment
Gloriosa superba
Quinine
Salicylates
Clinical features
Treatment
Selective serotonin reuptake inhibitors (SSRIs)
Snake bites
Clinical features
Treatment
Sodium valproate
Clinical features
Treatment
Theophylline
Clinical features
Treatment
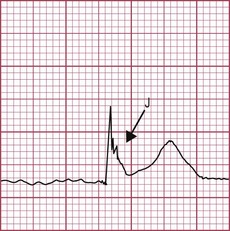
Tricyclic antidepressants (TCAs)
Clinical features
Treatment
Venlafaxine
This antidepressant is a serotonin–noradrenaline (norepinephrine) reuptake inhibitor (SNRI).
Clinical features
Treatment
Warfarin (p. 245)
Clinical features
Treatment
Bailey B. Glucagon in β-blocker and calcium channel blocker overdoses: a systematic review. J Toxicol Clin Toxicol. 2003;41:595-602.
Barceloux D, McGuigan M, Hartigan-Go K, et al. Position paper: cathartics. J Toxicol Clin Toxicol. 2004;42:243-253.
Bateman DN. Digoxin-specific antibody fragments: how much and when? Toxicol Rev. 2004;23:135-143.
Bateman DN. Tricyclic antidepressant poisoning: central nervous system effects and management. Toxicol Rev. 2005;24:181-186.
Borron SW, Baud FJ, Barriot P, et al. Prospective study of hydroxocobalamin for acute cyanide poisoning in smoke inhalation. Ann Emerg Med. 2007;49:794-801.
Bradberry S, Sheehan T, Vale A. Use of oral dimercaptosuccinic acid (succimer; DMSA) in adult patients with inorganic lead poisoning. QJM. 2009;102:721-732.
Bradberry SM, Sheehan TMT, Barraclough CR, Vale JA. DMPS can reverse the features of severe mercury vapor-induced neurological damage. Clin Toxicol. 2009;47:894-898.
Bradberry SM, Thanacoody HKR, Watt BE, et al. Management of the cardiovascular complications of tricyclic antidepressant poisoning: role of sodium bicarbonate. Toxicol Rev. 2005;24:195-204.
Brent J. Fomepizole for ethylene glycol and methanol poisoning. N Engl J Med. 2009;360:2216-2223.
British Medical Association and Royal Pharmaceutical Society of Great Britain. British National Formulary 58. London: BMJ Group and RPS Publishing; 2009.
Buckley NA, Isbister GK, Stokes B, Juurlink DN. Hyperbaric oxygen for carbon monoxide poisoning: a systematic review and critical analysis of the evidence. Toxicol Rev. 2005;24:75-92.
Chyka PA, Seger D, Krenzelok EP, et al. Position paper: single-dose activated charcoal. Clin Toxicol. 2005;43:61-87.
DeWitt CR, Waksman JC. Pharmacology, pathophysiology and management of calcium channel blocker and beta-blocker toxicity. Toxicol Rev. 2004;23:223-238.
Flamminger A, Maibach H. Sulfuric acid burns (corrosion and acute irritation): evidence-based overview of management. Cutan Ocul Toxicol. 2006;25:55-61.
Hall AP, Henry JA. Acute toxic effects of ‘ecstasy’ (MDMA) and related compounds: overview of pathophysiology and clinical management. Br J Anaesth. 2006;96:678-685.
Hoffman RS. Cocaine and β-blockers: should the controversy continue? Ann Emerg Med. 2008;51:127-129.
Krenzelok EP, McGuigan M, Lheureux P, et al. Position paper: ipecac syrup. J Toxicol Clin Toxicol. 2004;42:133-143.
Kulig K, Vale JA. Position paper: gastric lavage. J Toxicol Clin Toxicol. 2004;42:933-943.
Lheureux PE, Zahir S, Gris M, et al. Bench-to-bedside review: hyperinsulinaemia/euglycaemia therapy in the management of overdose of calcium-channel blockers. Crit Care. 2006;10:212.
Lheureux PER, Hantson P. Carnitine in the treatment of valproic acid-induced toxicity. Clin Toxicol. 2009;47:101-111.
Morgan M, Hackett LP, Isbister GK. Olanzepine overdose: a series of analytically confirmed cases. Int Clin Psychopharmacol. 2007;22:183-186.
Proudfoot AT, Krenzelok EP, Brent J, Vale JA. Does urine alkalinization increase salicylate elimination? If so, why? Toxicol Rev. 2003;22:129-136.
Proudfoot AT, Krenzelok EP, Vale JA. Position paper on urine alkalinization. J Toxicol Clin Toxicol. 2004;42:1-26.
Tenenbein M, Lheureux P. Position paper: whole bowel irrigation. J Toxicol Clin Toxicol. 2004;42:843-854.
Vale JA, Krenzelok EP, Barceloux DG, et al. Position statement and practice guidelines on the use of multi-dose activated charcoal in the treatment of acute poisoning. J Toxicol Clin Toxicol. 1999;37:731-751.
Waring WS, Good AM, Bateman DN. Lack of significant toxicity after mirtazapine overdose: a five-year review of cases admitted to a regional toxicology unit. Clin Toxicol. 2007;45:45-50.