98 Pleural rub
Salient features
Examination
• Differentiate between pleural rub and crackles by asking the patient to cough and check whether or not there is any change in the nature (no change with the pleural rub).
• Tell the examiner that you would like to proceed by listening for tachycardia and right ventricular gallop (pulmonary embolism).
Questions
How would you investigate this patient?
• D-dimer: Plasma D-dimers are cross-linked fibrin derivatives produced when fibrin is degraded by plasmin. D-dimers are not specific for pulmonary embolism and are seen myocardial infarction, pneumonia, sepsis, cancer, during the second and third trimesters of pregnancy and after surgery. Therefore, this test is most useful in the emergency department, because most patients already in hospital have elevated D-dimers
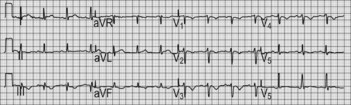
• ECG–RV strain (McGinn-White pattern). A normal electrocardiogram is very unusual in patients with massive acute pulmonary embolism (Fig. 98.1)
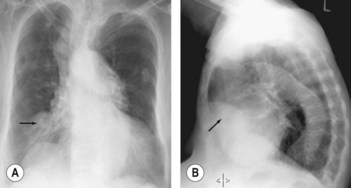
• Chest radiography: small wedge-shaped density at the periphery of the lungs indicates pulmonary infarction (‘Hampton’s hump’; Fig. 98.2)
• Ventilation–perfusion scan: most scans are, however, of intermediate or indeterminate probability and, therefore, CT is increasingly becoming the test of choice
• CT chest has now emerged as the main imaging test in the work up of pulmonary embolism (Fig. 98.3). Chest CT has two advantages: thrombus can be directly visualized and alternative diagnoses can be established on lung parenchymal images that are not evident on chest radiography. It takes <30 s with a single breath-hold to minimize respiratory motion