61
Plantar warts
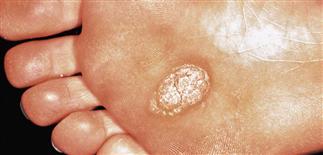
Plantar warts sometimes become confluent. The warty tissue is rough and thick. The excessive hyperkeratosis should be pared for topical treatment to be effective.

Mosaic plantar warts meld together, in this case in apposing skin. The warty tissue has spread the virus from the plantar foot to the apposing fifth toe.

Rough, flesh-colored, hyperkeratotic papules with punctuate hemorrhages along the lateral toe. The apposing toe is also affected. Most warts resolve with time and development of cellular immunity.

Mosaic plantar warts scattered on the heel. Pain or difficulty walking are indications for treatment, although painful destructive or scarring treatment should be avoided.
DESCRIPTION
Caused by human papillomavirus infection on plantar foot. Infection frequently occurs at points of maximal pressure, such as over heads of metatarsal bones, heels, or toes. A wart cluster is referred to as a mosaic wart.
HISTORY
• Human papillomavirus types 1, 2, and 4 are typically associated with plantar warts. • Hyperhidrosis is associated with a more widespread distribution of warts often refractory to treatment.
PHYSICAL FINDINGS
• Round, single or multiple, coalescing, flesh-colored, rough, keratotic papules often look depressed. • Punctate black dots, often seen on paring, are capillary loops. • May be tender with pressure. • Some are depressed, resembling numerous small pits. • Biopsy may be indicated if rapidly growing, ulcerated, atypical, or treatment-resistant; squamous cell carcinoma or melanoma may mimic a wart.
TREATMENT
Treatment often difficult; plantar warts can be refractory, recurrent. Often, multiple treatments required. Plantar warts do not require therapy if painless. Spontaneous resolution with time and development of immunity is the rule. Multiple treatment options exist, indicating no single best option.
Therapeutic options include the following. • Keratolytic therapy with salicylic acid (DuoPlant, Occlusal). A conservative initial treatment. Wart is pared, soaked daily in warm water, and salicylic acid preparation applied. Limitations: irritation, soreness. May require 6–8 weeks. • Plasters with salicylic acid 40% (Mediplast). Useful in treating plantar warts. Leave on for 24–48 h and replace. May require 6–8 weeks. • Imiquimod 5% cream (Aldara). May hasten resolution; one method is to use cryotherapy first, then apply imiquimod every night under duct tape occlusion for 6–12 weeks. • Blunt dissection. Fast, effective surgical treatment (90% cure rate); usually produces no scarring. Superior to both electrodesiccation and curettage and excision, because normal tissue is not disturbed. • Cryosurgery with liquid nitrogen. Nitrogen is applied for 15–30 s twice to wart. Resultant painful blister can interfere with mobility. Repeated light applications of liquid nitrogen are optimal. Treatment painful. • Carbon dioxide and pulsed dye laser treatment. Expensive. Probably no more effective than other treatments. • Electrodesiccation and curettage. Infrequently chosen due to pain from anesthesia, postoperative pain, risk of scarring. • Bleomycin. 0.5 units/mL injected into wart to achieve blanching. Wart size determines injection quantity. Responsive warts show hemorrhagic eschars that heal without scarring. Treatment very painful; necrosis or severe vasospasm may occur. Pregnancy a contraindication. An aggressive treatment option reserved for those experienced in its use.







