7 Placement learning pathways
• To explore the cancer and palliative care placement
• To understand how each team/specialty works in the practice placement
• To understand the health and safety requirements in the departments that may be visited from the hub placement
• How to plan insight visits and opportunities as part of the practice placement
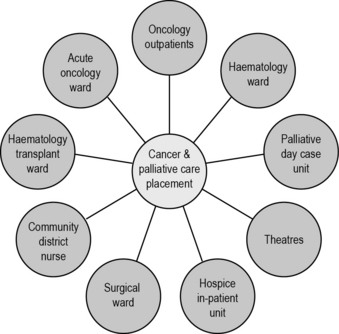
The cancer and palliative care placement
The ‘hub and spoke’ model in Figure 7.1 is supported by the NMC. It gives you the opportunity to be allocated to one clinical area for a period of time while also having the opportunity to be allocated to a spoke area and short insight visits.
The length of the placement may depend on the year of study as well as local arrangements between the university and clinical areas. Box 7.1 outlines a theoretical example of what a first year nursing student’s 18-week (‘year-long’) placement might look like. This sample placement demonstrates a wide range of learning opportunities that can stem from a core hub placement. It is important to remember that a cancer patient can be nursed in any clinical environment. Some placements will be much shorter than this, most ranging between 8 and 12 weeks. This is dependent on the school of nursing and your stage of training.
Box 7.1 A theoretical example of a first year nursing student’s 18-week placement
Weeks 6–7: Spoke – oncology outpatients
Initial patient consultation, treatment decision making, follow-up clinics.
Insight visits: oncologist, site-specific nurse specialist, radiology investigations.
How each team/specialty works in the practice placement
Health and safety requirements in the departments that may be visited from the hub placement
For students who are not working on a specialist chemotherapy/radiotherapy ward, it is important to understand the precautions necessary if escorting a patient to one of these areas or if you spend a day in one of the departments. If you have attended an induction day for the placement, you may have covered these safety topics and this will be a refresher for you.
Extravasation
There are many factors that may influence whether a patient experiences an extravasation:
Healthcare professional-related factors
If an extravasation is suspected, swift action is required. Cytotoxic drugs are categorised into groups depending on the damage they may cause if they extravasate: neutral, irritant and vesicant. The management of each type of drug that extravasates will be treated differently: either spread and dilute or localise and neutralise. Each department that administers cytotoxic drugs should have a policy for how each drug should be handled in the event of it leaking. Each department will also have an emergency extravasation kit which comprises all equipment needed.
Radiation
Obviously radiation has health implications, and ensuring you are not exposed to it is the key to protecting yourself. Every unit that administers radioactive treatment has guidelines called the ‘local rules’ that set out safe practice to protect all individuals. The key principles of the local rules of radiation safety are time, distance and using barriers. As a student nurse, you should never enter a room where a patient has a radioactive source within their body or is receiving external beam radiation (discussed in Chapter 13). Look for the radiation warning sign to identify potential patients. Where a radiation source can be removed temporarily (such as a ‘selectron’ machine), a qualified member of the team can switch the machine off. Once you have checked that the radiation has been safely removed, you may enter the room.
Planning insight visits and opportunities as part of the practice placement
As you prepare for this placement, having considered the wide range of teams and services available as part of the cancer and palliative care specialty, review your competency documentation and essential skills clusters and note down the areas that you need to focus on. Considering the spoke opportunities now night be a way of achieving a wide variety of competencies.
Health and Safety Executive. Safe handling of cytotoxic drugs. Information sheet MISC615.. London:HSE; 2003.
Nursing and Midwifery Council. Standards for pre-registration nursing education. Online. Available at:. 2010. http://standards.nmc-uk.org/PreRegNursing/statutory/background/Pages/introduction.aspx (accessed May 2011)
Royal College of Nursing. Clinical practice guidelines: the administration of cytotoxic chemotherapy. RCN, London: Recommendations; 1998.
Wengstrom Y., Margulies A. European Oncology Nursing Society extravasation guidelines. European Journal of Oncology Nursing. 2008;12(4):357–361.
Cytotoxic handling forum and guidelines. http://www.marchguidelines.com/ (accessed May 2011).
The National Extravasation Information Service, http://www.extravasation.org.uk/ (accessed May 2011).
NHS Education for Scotland (NES), Website supporting practice education, with a specific forum discussing practitioners caring for cancer patients and the health and safety issues of cytotoxic drugs and radiation: http://www.nes.scot.nhs.uk/education-and-training/by-discipline/nursing-and-midwifery/practice-education.aspx (accessed November 2011).