Pituitary function
The pituitary gland
Anterior pituitary hormones
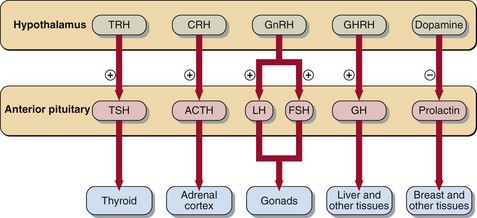
 TSH (thyroid-stimulating hormone), acts specifically on the thyroid gland to elicit secretion of thyroid hormones.
TSH (thyroid-stimulating hormone), acts specifically on the thyroid gland to elicit secretion of thyroid hormones.
 ACTH (adrenocorticotrophic hormone) acts specifically on the adrenal cortex to elicit secretion of cortisol.
ACTH (adrenocorticotrophic hormone) acts specifically on the adrenal cortex to elicit secretion of cortisol.
 LH (luteinizing hormone) and FSH (follicle-stimulating hormone), known jointly as the gonadotrophins, act cooperatively on the ovaries in women and the testes in men to stimulate sex hormone secretion and reproductive processes.
LH (luteinizing hormone) and FSH (follicle-stimulating hormone), known jointly as the gonadotrophins, act cooperatively on the ovaries in women and the testes in men to stimulate sex hormone secretion and reproductive processes.
 GH (growth hormone) acts directly on many tissues to modulate metabolism. Metabolic fuels (e.g. glucose, free fatty acids) in turn modify GH secretion.
GH (growth hormone) acts directly on many tissues to modulate metabolism. Metabolic fuels (e.g. glucose, free fatty acids) in turn modify GH secretion.
 Prolactin acts directly on the mammary glands to control lactation. Gonadal function is impaired by elevated circulating prolactin concentrations.
Prolactin acts directly on the mammary glands to control lactation. Gonadal function is impaired by elevated circulating prolactin concentrations.
The hypothalamic factors that control anterior pituitary hormone secretion are shown in Figure 42.1.
Hyperprolactinaemia
 stress (venepuncture is sufficient to raise plasma prolactin in some patients)
stress (venepuncture is sufficient to raise plasma prolactin in some patients)
 drugs (e.g. oestrogens, phenothiazines, metoclopramide, α-methyl dopa)
drugs (e.g. oestrogens, phenothiazines, metoclopramide, α-methyl dopa)
 primary hypothyroidism (prolactin is stimulated by the raised TRH)
primary hypothyroidism (prolactin is stimulated by the raised TRH)
If these causes are excluded, the differential diagnosis is between:
Pituitary tumours
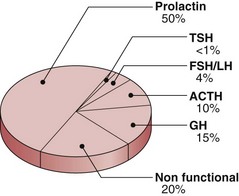
Pituitary tumours may be either functional (that is they secrete hormones) or non-functional. The incidence of different tumour types is shown in Figure 42.2. Local effects include headaches, papilloedema and visual field defects. There may be specific signs of hormone excess particularly in acromegaly, Cushing’s syndrome and prolactinoma. There may be signs of hypopituitarism in skin, hair and musculature.
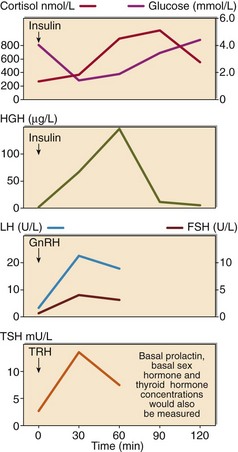
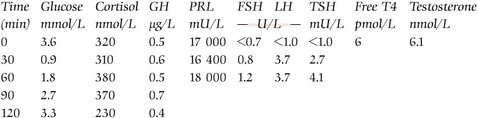
The impact of the tumour on pituitary function requires formal assessment by dynamic function tests. GH and ACTH-secreting cells are most vulnerable, and an insulin stress test (see p. 82) may suffice. However, comprehensive assessment of anterior pituitary reserve requires a combined anterior pituitary function test (Fig 42.3). TRH, GnRH and insulin are administered. All hormones are assessed at 0, 30 and 60 minutes, and GH additionally at 90 and 120 minutes. It is usual also to assess basal thyroid (thyroxine) and gonadal (testosterone or oestradiol) function.
Treatment
 Medical. Dopamine agonist drugs like bromocriptine and cabergoline are widely used to treat hyperprolactinaemia, especially when due to microprolactinomas. They may also be used to shrink large suprasellar prolactinomas before surgery.
Medical. Dopamine agonist drugs like bromocriptine and cabergoline are widely used to treat hyperprolactinaemia, especially when due to microprolactinomas. They may also be used to shrink large suprasellar prolactinomas before surgery.
 Surgery. Trans-sphenoidal hypophysectomy is the standard procedure. Patients undergoing this are routinely given steroid cover (usually hydrocortisone), in case they cannot mount an adequate cortisol response to the stress of the operation. For the same reason, postoperative assessment of pituitary reserve should be deferred for several days.
Surgery. Trans-sphenoidal hypophysectomy is the standard procedure. Patients undergoing this are routinely given steroid cover (usually hydrocortisone), in case they cannot mount an adequate cortisol response to the stress of the operation. For the same reason, postoperative assessment of pituitary reserve should be deferred for several days.
 Radiation. The impact of radiation on pituitary function is cumulative, and irradiated patients require annual dynamic function testing of their anterior pituitary reserve thereafter.
Radiation. The impact of radiation on pituitary function is cumulative, and irradiated patients require annual dynamic function testing of their anterior pituitary reserve thereafter.