Pioneers and Milestones in the Field of Orthodontics and Orthognathic Surgery
• Pioneers in the Field of Orthodontics
• Early Pioneers in the Field of Orthognathic Surgery
• Hugo L. Obwegeser: Development of the Standard Orthognathic Procedures
• William H. Bell: Experimental Studies to Confirm the Biologic Basis of the Standard Orthognathic Procedures
• Hans G. Luhr: Development of Plate and Screw Fixation for Craniomaxillofacial Surgery
Pioneers in the Field of Orthodontics
Background
Orthodontic appliances that are somewhat primitive but surprisingly well-designed for their time have been found in Ancient Greek written materials.8 Four Etruscan specimens of young adult women dating back to 900 B.C. that specifically demonstrate appliances on the teeth have also been recovered.23,208 The orthodontic type appliances are gold bands around teeth that are adjacent to an edentulous gap. The appliances appear to be for the purpose of managing the space left by tooth loss earlier in life (Fig. 2-1).209 In addition, the Ancient Greek scholars Hippocrates and Aristotle both have writings that discuss various ways to straighten teeth and to treat various dental conditions.20,51 Knowledge of dental extractions carried out for the purpose of mechanically straightening the remaining teeth was also reported by Leonardo da Vinci during the High Italian Renaissance.166 The bandolet or bandeau, which was created in 1723 by Pierre Fauchard of France, was the first documented dental arch expansion appliance (Fig. 2-2).202 It consisted of a heavy maxillary labial arch wire to which the teeth were ligated.202 The term orthodontia is said to have been coined in 1841 by Lafoulon, and it appeared in the book about malocclusion written by J.M. Alexis Schange.11,157,203
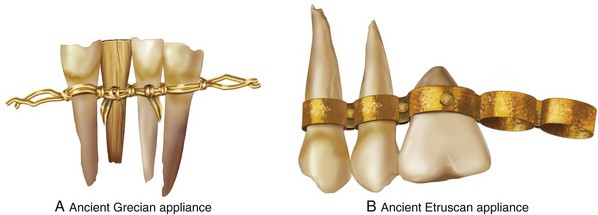
Figure 2-1 A, A drawing of the anterior mandibular dentition in a mummy specimen from ancient Greece (approximately 1000 B.C.) currently housed in the Archaeological Museum in Athens, Greece. A gold wire was used to tie teeth together and to band others to support replacements. The use of human, animal, carved wood, bone, or ivory for replacement teeth was practiced by the ancient Grecian society. B, A drawing of an ancient Etruscan orthodontic appliance found on the maxilla of a mummy in a tomb (approximately 700 B.C.), which is currently at the Civic Museum in Cornet, Italy. It demonstrates gold soldered rings and rivets to hold dental replacements as a bridge. The specimen has two natural teeth, one riveted oxtooth and four spaces for others
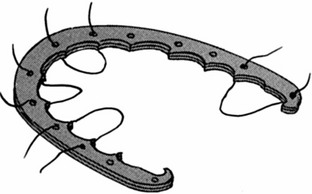
Figure 2-2 Illustration of the “bandolet” bandeau, which was created in 1723 by Pierre Fauchard of France. This was the first documented dental arch expansion appliance.
In 1858, perhaps the first formal article on orthodontics published in a medical journal was written by Norman W. Kingsley (Fig. 2-3). By the 1880s, Norman Kingsley’s Treaties on Oral Deformities as a Branch of Mechanical Surgery systematically described the current techniques of the day for the repositioning of teeth (Fig. 2-4).109 Kingsley was among the first to fully describe how extraoral forces (e.g., headgear) could be used to correct protruding maxillary anterior teeth. His emphasis was primarily on the alignment of the anterior maxillary teeth in an attempt to improve facial appearance. To Kingsley, the extraction of teeth for the purpose of uncrowding and to reduce the protraction of the incisors was acceptable practice. Details of how the upper and lower teeth articulated with each other (i.e., occlusion) were of secondary importance. He used a wide variety of apparatus to reposition the anterior teeth, including wires, bands, custom palatal plates, elastics, wedges, linen twine, rubber tubing, leathers, gold bands, and vulcanite. Impressions of the teeth and dental models were used during planning and for the precontouring of labial placed wires. The use of an external apparatus placed over the top of the head and then either secured to the chin or held with bands secured to the maxillary incisors became part of his everyday practice (Fig. 2-5).
Figure 2-4 Norman Kingsley’s text entitled A Treatise on Oral Deformities as a Branch of Mechanical Surgery, which was published in 1880.

Figure 2-5 Headgear designed and used by Norman W. Kingsley. According to Kingsley, “I sat to work to make an apparatus that would pull the lower jaw back. As you can see from the photograph taken at the time she was wearing the apparatus, it consists of two parts. For the lower part, I made a brass plate to fit the chin, having arms with hooked ends reaching to a point just below the point of the chin. These arms were arranged in such a way that the distance between them could be altered at will by simply pressing them apart or to gather. The upper part consisted of a simple network going over the head and having two hooks on each side, one hook being above and the other below the ear. When the apparatus was completed and in use, there were four ligatures of ordinary elastic rubber pulling in such a way as to force the lower jaw almost directly backward.” From Kingsley NW: A treatise on oral deformities as a branch of mechanical surgery, London, 1880, H.K. Lewis, pp 137, Figure 68.
Kingsley’s basic principles for the mechanical alignment of the teeth can be summarized as follows:
• The positioning of the six maxillary anterior teeth with regard to each other and in relationship to the lip is essential for facial aesthetics.
• The contact of a certain number of maxillary and mandibular posterior teeth, at least on one side, is important for the grinding and mastication of food.
• All other teeth are potentially expendable, depending on the effort required by the clinician for straightening and the individual’s desire to maintain them.
• From both a mastication and an aesthetic perspective, there is no particular need for the maintenance of all 32 teeth or to achieve a specific and detailed way of the upper and lower teeth occluding with one another.
Dr. Kingsley also commented on facial aesthetics, stating that “the eye soon tires of the stiffness and formality of unbroken uniformity, and is only permanently pleased with the beauty which comes from graceful variation.”109 He acknowledged the occurrence of jaw deformities when he said that “[a] lack of harmony between the maxilla and mandible is occasionally seen. For instance, when the mandible is very large and massive or unusually small in comparison to the upper jaw. When present, this will interfere with the harmony of the surrounding parts of the face.”109
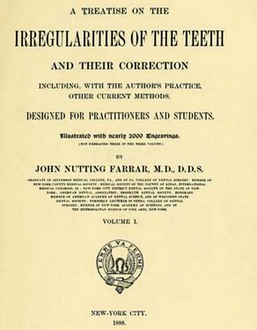
In 1897, J.N. Farrar published a two-volume illustrated text entitled A Treatise on the Irregularities of the Teeth and Their Corrections (Fig. 2-6).12 In that text, he also demonstrates detailed orthodontic appliances, and he was among the first to suggest the advantages of mild (rather than heavy) force applied at intervals to effectively move the teeth.10
Edward H. Angle
It was common practice through the later half of the 19th century to extract the teeth in response to most dental problems.9,60 Restorative dentistry was generally not the first choice for the management of “toothaches.” Most adults at that time (i.e., the 1880s) did not have a full complement of teeth nor was there much stigmata associated with partial edentulism.210 Details of how the teeth occluded with each other seemed important only when establishing how upper and lower dentures were to meet so as to prevent loosening or mobility when wearing them and to improve chewing ability. It was a natural extension of this thinking for a prosthodontic-trained dentist like Edward H. Angle to develop a more holistic concept regarding the importance of the occlusion of the natural dentition (Fig. 2-7).5–8 During his career, Angle taught prosthetics at the University of Minnesota (Minneapolis, Minn), Northwestern University Dental School (Chicago, Ill), and the Missouri Dental College (St. Louis, Mo). Dr. Angle’s interest in dental occlusion and his ingenuity and dedication with regard to the correction of malocclusion led to the development of the specialty that we now call “orthodontics.”
Angle’s textbook, Treatment of Malocclusion of the Teeth, was first published in 1887 (Fig. 2-8).6 It went into seven much-revised editions, and it laid the foundation for the modern specialty of orthodontics. The publication of Angle’s classification of malocclusion during the 1890s was a key step in the development of orthodontics (Fig. 2-9).42,43 Angle introduced the first precise and simple definition of the normal human occlusion of the natural dentition. He postulated that a key aspect of how the teeth should fit together was the positioning of the maxillary first molars. He then went on to describe three classes of malocclusion that were based on the occlusal relationships of the first molars:
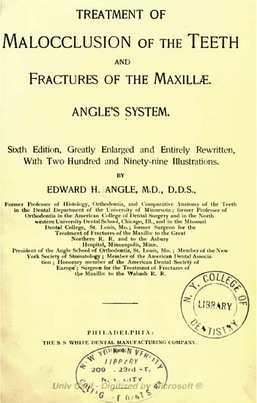
Figure 2-8 Dr. Angle published a comprehensive text entitled A Treatment of Malocclusion of the Teeth and Fractures of the Maxillae, the first edition of which was published in 1887. It went into seven revised editions, and it laid the foundation for the modern specialty of orthodontics.
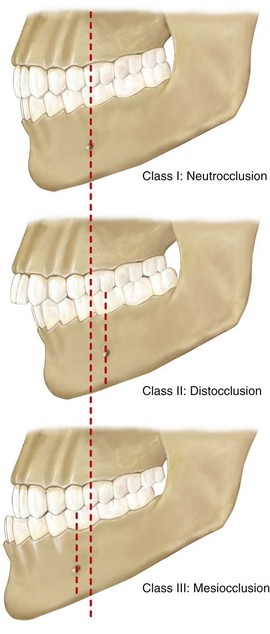
Figure 2-9 Angle described three classes of malocclusion based on the relationships of the first molars: Class I, Class II, and Class III.
Class I: There is a normal relationship of the molars, but the line of occlusion is incorrect as a result of malposed teeth, rotations, or other causes.
Class II: The lower molar is distally positioned relative to the upper molar, and the line of occlusion is not specified.
Class III: The lower molar is mesially positioned relative to the upper molar, and the line of occlusion is not specified.
Angle’s classification actually has four classes:
By the early 1900s, orthodontists no longer just aligned irregular teeth in each arch.175,218 The practice had now evolved into the treatment of malocclusion (i.e., how the upper and lower teeth align with each other). Angle’s philosophy was to achieve a specific relationship between the upper and lower teeth for each patient. Since Angle’s precisely defined dental relationships also required a full complement of teeth in each arch, the maintenance of an intact dentition became an important component of orthodontic treatment. Angle and his followers strongly opposed extraction for orthodontic purposes.69 In an attempt to achieve the three-axis control of tooth movement, Angle introduced the ribbon arch (Fig. 2-10).70 He then devised the edgewise appliance to overcome the weaknesses of the ribbon arch (Fig. 2-11). The Angle reoriented bracket slot was designed to control the bodily movement of teeth and to limit tipping.135 Angle also heavily relied on the use of intraoral rubber bands and limited the use of extraoral appliances (e.g., headgear) as much as possible.
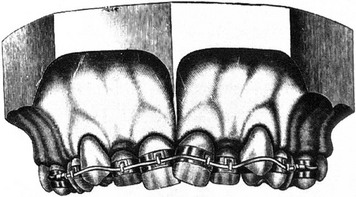
Figure 2-10 The ribbon arch appliance, which was introduced by Angle in 1916. The vertical slot in the bracket accepts either round or rectangular wire, which in turn is held in place by a locked pin.
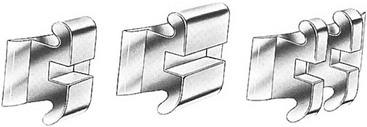
Figure 2-11 The edgewise bracket attachment comes in a variety of modifications. The original single bracket (left) has been widened for molar teeth and for greater rotational control (center). The twin edgewise modification (right) is available in different widths, and it is used most frequently because of its greater versatility, its reduced frictional component, and its adaptability to various light-wire techniques.
Angle was among the first to state that jaw discrepancies exist in some individuals and that these discrepancies will prevent the achievement of a normal occlusion. He then acknowledged the need for jaw-straightening surgery. In Chapter 14: Operative Surgery of the sixth edition of Angle’s textbook, he states that the use of appliances to move teeth may be properly called conservative surgery to distinguish it from more bold or aggressive operations involving the use of cutting instruments, which were designated as operative surgery. He states the following: “While such operations [mandibular osteotomies] should probably be employed only as auxiliary to the conservative method, they are doubtless destined to play an more important part in the practice in the future.”6
Dr. Angle worried that no technique that relied solely on tooth movement could establish the appropriate relationships of the teeth or truly improve the facial lines in cases involving the severe overdevelopment of the inferior maxilla [mandible].6 He felt that these cases may be successfully treated by removing a section of bone from each of the lateral halves of the mandible. At the time, the removal of a single complete section of the jaw had been reported for cases involving such conditions as ankylosis, tumors, and gunshot wounds, but Dr. Angle was unable to find information about the removal of complete sections from each of the lateral halves of the mandible. This idea was discussed by Dr. Angle with various surgeons and dentists and determined to be feasible. His proposal involved the following6:
• Careful photographs should first be taken of the patient.
• Two accurate models should be made of the lower dental arch, and one should be made of the upper.
• One of the plaster models of the lower jaw should then be sawed through and the sections removed.
• The positions and extent of the sections should be carefully experimented with until the three remaining sections of the model could be made to best harmonize with the upper arch so that the teeth may be in best possible occlusion with those of the upper jaw.
• The sections of the plaster model should then be cemented or waxed together.
• Over this reconstructed model, a vulcanite or metal splint should then be formed.
• With the use of careful comparisons and measurements of the reconstructed model as compared with the unchanged model, the exact size and form of both resections of bone to be removed can be determined so that there need be no guessing as to the relationships of the bone. In this way, complete apposition of the cut ends can be made.
• Because there is a lingual inclination of the lower incisors in all cases of mandibular prognathism, the sections of bone to be removed must not be parallel on their sides but instead more or less wedged or V-shaped to gain the best positions for the occlusion of the incisors as well as for the appearance of the chin.
• The degree of variation from the parallel of the lines of bone resection must be determined by the conditions that are present (i.e., patient variation).
• Because the operation must be skillfully performed, the most rigid support should be given to the reconstructed jaw. This technique (i.e., a cap splint over the teeth) should give more rigid support than is possible with the crude, unstable, and unmechanical plan of wiring the ends of the bone together, which is so often employed for the reduction of fractures.
According to Dr. Angle, “The question most often raised by dentists in discussing the practicability of an operation as outlined above was the uncertainty as to union of the bones and as to impairment of vitality of the teeth in the anterior segment [of the mandible].”36 However, Dr. Angle helped with the overcoming of these concerns via two case reports that were presented in his textbook, Treatment of Malocclusion of the Teeth and Fractures of the Mandible: Angle’s System6 (pp 173-184):
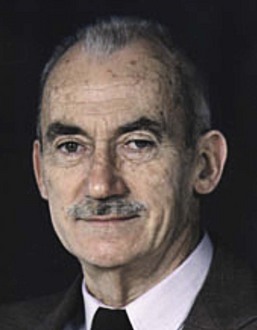
Holly Broadbent
The introduction of the cephalometer by Holly Broadbent in 1931 was another important milestone that placed orthodontic research on a scientific foundation (Fig. 2-12).157 For the first time, it made possible the accurate study of the facial bones in the growing child (Figures 2-13 and 2-14). It became a valuable supplement to the orthodontist’s plaster models and intraoral x-rays. The value of serial cephalograms in clinical practice was quickly realized. Broadbent’s original work on the “face of the normal child” and Brody’s classic research “on the growth pattern of the human head from the third month to the eighth year of life” were among the earliest contributions.163 These were followed by the research of Down’s “Variations in Facial Relationships,” the work of Thompson in “Functional Analysis of Occlusion,” Wylie’s “Assessment of Anterior-Posterior Dysplasia,” and the work of Margolis’ “Basic Facial Pattern and Its Application in Clinical Orthodontics.”174 The use of cephalometric radiography in clinical practice became widespread after World War II and made clear to all clinicians that many of the Class II and Class III malocclusions being treated actually resulted from abnormal skeletal relationships rather than just malposed teeth.165 These radiographic truths were hard to ignore and further inspired orthodontists and surgeons to search for operative solutions.181

Figure 2-12 Photograph of Holly Broadbent (1894-1977). From Broadbent BH Sr., Broadbent BH Jr and Golden WH: Bolton Standards of Dentofacial Developmental Growth, St. Louis, C.V. Mosby, 1975.
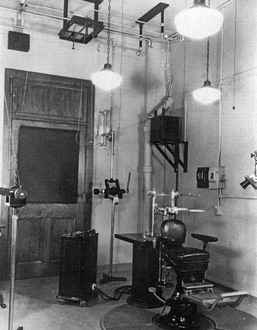
Figure 2-13 Broadbent was the first to develop the standardized lateral “head plate.” The cephalometer is a device for holding the patient’s head, the x-ray film, and the central ray of the x-ray machine in proper relationship with one another. Ear-rod extensions are necessary to adjust the head so that the profile is centered, regardless of the size or shape of the head. The orbital pointer and the ear rods adjust the patient’s head along the horizontal or Frankfort plane. An adjustable chair is used, and the teeth are placed in “centric occlusion” unless otherwise indicated. The cephalometer may be rotated so that posterior and anterior radiographs as well as profile radiographs can be taken. The central ray is directed through the ear rods, thereby producing a circle on the x-ray film. From Broadbent BH Sr., Broadbent BH Jr and Golden WH: Bolton Standards of Dentofacial Developmental Growth, St. Louis, C.V. Mosby, 1975.
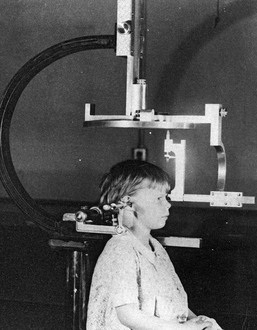
Figure 2-14 The cephalostat device, as described in Figure 2-13, is shown with a patient who is positioned and ready for film exposure. From Broadbent BH Sr., Broadbent BH Jr and Golden WH: Bolton Standards of Dentofacial Developmental Growth, St. Louis, C.V. Mosby, 1975.
Charles Tweed and Raymond Begg
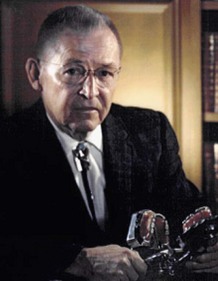
Another “orthodontic truth” was also soon to fall. A purest “Angle” approach to maintaining and straightening all of the teeth in all patients frequently proved untenable with regard to the maintenance of the occlusion after the appliances were removed.54,144,145 This non-extraction, arch-expansion approach gave little consideration to long-term periodontal health or to the individual’s overall facial aesthetics.161 The extraction of teeth (typically the bicuspids) to achieve occlusal stability and periodontal health was reintroduced into American orthodontics during the 1930s by Charles Tweed (Fig. 2-15) and simultaneously into the United Kingdom (Australia) by Raymond Begg (Fig. 2-16) (see Chapter 17 for in-depth discussion).47–49,59,204
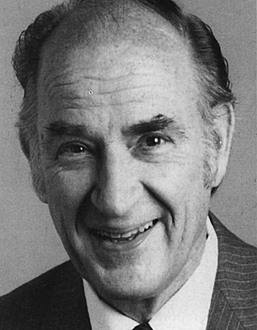
Lawrence F. Andrews
Dr. Lawrence F. Andrews’ pioneer contributions to the field of orthodontics and the treatment of dentofacial deformity must also be mentioned (Fig. 2-17).2–4 After completing orthodontics training at Ohio State University in 1958, he entered private practice that was limited to orthodontics. Early in his career, Dr. Andrews recognized clinical problems that were yet unsolved and sought solutions. This sent him on a search to better understand occlusion as well as deviations from normal. Between 1960 and 1964, Dr. Andrews began to gather data for analysis. One hundred and twenty non-orthodontic normal (dental) models were acquired with the cooperation of local dentists, orthodontists, and a major university. The models selected for study were of teeth that had never undergone orthodontic treatment; that were straight and pleasing in appearance; that had a bite that looked generally correct; and that, in Dr. Andrews’ judgment, would not benefit from orthodontic treatment.
Dr. Andrews studied the crowns of this multisource collection of models to ascertain which characteristics, if any, would be found consistently in all of them. Angle’s molar cusp groove concept was validated but found to be incomplete. After meticulous evaluation, including comparison with “treated cases” from the nation’s most skilled orthodontists (n = 1150), six consistent occlusal characteristics were formulated by Dr. Andrews in general terms and then explained in detail.2 The six fundamental qualities or Six Keys of Optimal Occlusion were validated not solely because all were present in each of the non-orthodontic normal models (n = 120) but because the lack of even one of the six was a defect that was predictive of an incomplete end result in the orthodontically treated models that were studied (n = 1150).
In his published article, Dr. Andrews acknowledged that, although each normal person is unique in his or her own way, they nevertheless have much in common.2 The 120 non-orthodontic normal models studied differed with regard to certain aspects, but all shared the Six Keys. Dr. Andrews suggested that we use as our benchmark “nature’s best” and that, in the absence of abnormalities outside of our control, we limit compromise and strive for the ideal. He developed the straight-wire appliance in 1970 for orthodontic use to help accomplish these objectives. This preadjusted appliance soon became the standard of the specialty.2–4
Element I: Proper arch shape and positioning of the maxillary and mandibular teeth (roots) over the basal bone
Element II: Proper horizontal (sagittal) projection of the maxilla
Element III: Proper width of the maxillary and mandibular arches
Element IV: Proper vertical height of the maxilla
Element V: Proper prominence (shape) of the chin (i.e., pogonion prominence)
Element VI: Establishment of the Six Keys to Optimal Occlusion
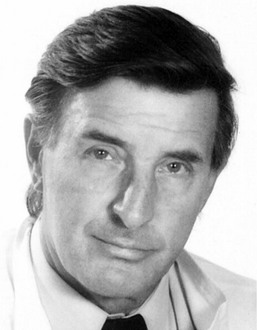
William R. Proffit
By the mid 1970s, Dr. Proffit recognized the benefits of a collaborative surgeon–orthodontist interaction for the correction of dentofacial deformities.164 He and others convincingly demonstrated to surgeons that rectangular orthodontic arch wires in edgewise brackets were satisfactory for surgical patients without the need for the intraoperative placement of Erich arch bars. This paved the way for the routine preoperative orthodontic relief of dental compensations, and it was followed by the placement of orthodontic “surgical wires and hooks” for intraoperative use. After the initial surgical healing, a smooth transition to orthodontic maintenance and detailing soon became the standard of care. Dr. Proffit was also an early believer in the importance of a collaborative effort to understand the patient’s presenting dysfunction and dysmorphology and then to develop a comprehensive treatment plan. The use of a cephalometric analysis with prediction tracings followed by dental model planning with splint construction became the routine. Dr. Proffit and others also insisted on analysis of the early results that were achieved. This was followed by critical studies of the long-term outcomes after various surgical approaches and orthodontic techniques were employed. This analytic approach has been responsible for much progress in the field over the past four decades.
According to Dr. William R. Proffit* (Fig. 2-18), orthodontics in the 21st century differs from that of the previous century in three fundamental ways162,163:
1. There is more emphasis on both facial and dental aesthetics and less on the details of dental occlusion as an overriding objective. This has much to do with the safe and reliable orthognathic surgical techniques that are currently available and with the recognition that long-term stable occlusion and periodontal health can best be achieved in conjunction with harmonious jaw relationships. This will require extractions when necessary to uncrowd and achieve periodontal health; decompensating orthodontic therapy to place teeth that are solidly in the alveolar bone; and jaw-straightening surgery, when indicated.
2. Patients and families expect greater involvement in the treatment planning process. Full disclosure requires the orthodontist to consider and review ideal and compromised treatment options. Providing a balanced and objective assessment of each option’s effect on facial aesthetics, dental stability, periodontal health, speech articulation, and the upper airway is ideal. Consultation with appropriate dental, surgical, and medical specialists before instituting treatment has become the standard of care.
3. Orthodontics is now offered not just to children, adolescents, and young adults but also to older adults through an interdisciplinary approach. Consideration should be given to facial aesthetics, occlusion, periodontal health, the upper airway, speech articulation, and the long-term maintenance of the dentition. There is increased emphasis on coordinated treatment with other dentists, surgeons, and medical specialists. Taking advantage of currently available sophisticated orthodontics and orthognathic surgery to provide individuals of all ages with quality care should now be considered routine.
Early Pioneers in the Field of Orthognathic Surgery
Mandibular Setback for Prognathism
Simon Hullihen described a procedure for the correction of mandibular dentoalveolar protrusion in the American Journal of Dental Science in January 1849 (Fig. 2-19, A).18,98 Technically, this was a bilateral bicuspid region wedge ostectomy to “set back” the anterior mandibular dentoalveolar segment. The osteotomy did not violate the inferior border of the mandible. The procedure was performed on a middle-aged woman whose mandibular deformity was the result of a severe burn scar contracture of the anterior neck and lip from an injury that had occurred during her childhood (see Fig. 2-19, B and C).
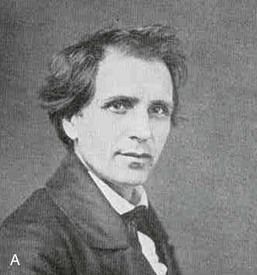
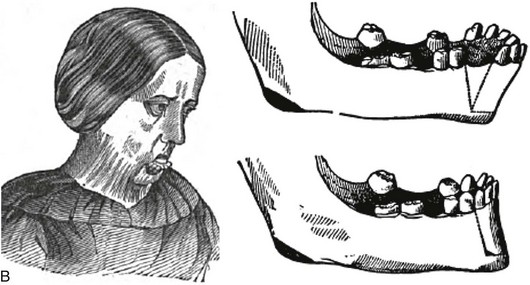
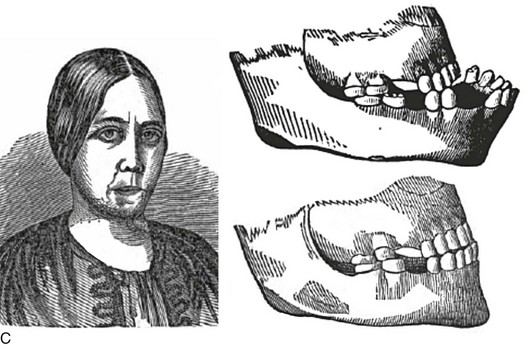
Figure 2-19 A, Photograph of Simon Hullihen (1810-1897). B, Illustration of anterior mandibular dento-alveolar segmental osteotomy proposed and C, carried out by Dr. Hullihen. A from Ambrecht EC: Hullihen, the oral surgeon. Int J Orthod Oral Surg 23:377, 511, 598, 711, 1937. B and C from Hullihen S: Case of elongation of the under jaw and distortion of the face and neck, caused by a burn, successfully treated. Am J Dent Sci 9:157, 1849.
In 1887, Berger from Lyon, France, described bilateral condylar neck osteotomies to set back the prognathic mandible.90 In 1895, Jaboulay also reported the bilateral osteotomy of the condylar neck (condylectomy) for the correction of prognathism.100 This method continued to be popular in France for the treatment of prognathism through the 1950s.75
On December 19, 1897, Vilray Blair in St. Louis, Mo, carried out a distinct modification of the original Hullihen procedure for the treatment of mandibular prognathism (see the “Second Patient (Operation)” case report by Dr. Angle earlier in this chapter) (Fig. 2-20).38 The operation was performed on a 22-year-old man with asymmetric mandibular prognathism. The young man had difficulty with chewing and speech articulation, and he also was self-conscious about his appearance; thus, he was enthusiastic about proceeding with the recommended surgical plan. Dr. Blair stated that the immediate surgical objective was to carry out bilateral body osteotomies to shorten the horizontal ramus [body of the mandible] and to change the mandibular angle [rotate the distal mandible counterclockwise], thereby allowing for the closure of the open bite. Dr. Blair’s preoperative concerns about the operation included the following:
1. Could a portion of the mandible be cut out on each side in a satisfactory way?
2. Would sacrifice of the inferior dental nerve cause detrimental injury to the distal mandible?
3. After healing had occurred, would the mandible continue to grow and cause a recurrence of the deformity?
Through cadaver dissections, Dr. Blair satisfied his concerns regarding whether the mandible could be sectioned and repositioned successfully. As a result of the age of the patient (22 years), he had little concern regarding further growth after surgery. He conferred with two other surgeons (Dr. E.H. Gregory and Dr. P. Tupper), both of whom concurred that the surgical plan seemed reasonable. The patient was also under the care of Dr. J.W. Whipple (orthodontist). Dr. Blair had discussed the feasibility of a surgical solution for mandibular prognathism with Dr. Angle (the patient had also consulted with Dr. Angle before surgery), and Dr. Angle “had advised such an operation.”38
The surgery was carried out at the Missouri Baptist Sanatorium. The surgery commenced with the patient under chloroform anesthesia at 9:20 AM with the patient in the recovery room by 10:30 am. During the operation, the patient’s head was hyperextended over the end of the operating room table. Skin incisions below the inferior border of the mandible on each side provided exposure. The incisions extended up into the mouth and involved cutting through the mucous membrane. A full-thickness osteotomy was to be completed on the left side of the mandible between the first and second bicuspids and on the right side between the second bicuspid and the first molar. The osteotomy was initiated with a “double-bladed saw” three quarters of the way through on each side; the inferior border remained intact.38 This allowed for the presence of a stable mandible on each side before the cut was fully completed on either side. A drill was used to place holes on either side of the osteotomy site for eventual “cooper wire fixation”38 near the inferior border on each side before cutting through the inferior border on either side. After the completion of both full-thickness osteotomies, soft gutta-percha was placed over the mandibular dentition, and the upper and lower teeth were firmly wired together through the gutta-percha. This method of intermaxillary fixation immobilized the distal mandible in its new position for the closure of the open bite. Dr. Blair stated that “this method of fixation was suggested to him by seeing Dr. Angle’s fracture bands.”38 The fracture band method of mandible fracture management was commonly in use.
Dr. Blair stated that, as the patient was emerging from the anesthesia, the vomiting of mucus and blood occurred, thereby necessitating the cutting of the intermaxillary fixation.38 After the vomiting subsided, rather than reapplying intermaxillary fixation, a Barton bandage of plaster was used to secure the mandible into occlusion with the maxilla.21 When the Barton bandage was removed several weeks later, Dr. Blair felt that there was “bony union on the right side and a very slight but perceptible motion on the left side when the fragments were grasped.”38 Dr. Blair decided to take the patient to the office of the treating dentist (orthodontist), Dr. Whipple. He requested that Dr. Whipple place two dental bands with a bar between them across the weak left osteotomy site. This would afford the patient sufficient support and allow him to go without the additional protection of a Barton bandage or intermaxillary fixation.” Unfortunately, while he was tightening the bands across the left and right osteotomy sites, Dr. Whipple “broke the union of the provisional callus.”38 At this point, Dr. Whipple applied properly adjusted bands to the teeth on the left side of the mandible, and Dr. Blair reapplied a Barton plaster external facial bandage.38 Dr. Whipple also placed crowns on the mandibular teeth posterior to the osteotomy sites so that the molars would occlude properly with the upper teeth, and he filled some points on the teeth to improve the occlusion of the incisors.38 Apparently, the combination of the mandibular setback with the clockwise rotation resulted in “a small [osteotomy] gap between the second bicuspid and first molar on the right side” but “without a gap [previous edentulous space] in the left first bicuspid region.”38 Despite these difficulties, the osteotomies went on to heal with a reasonable correction of the occlusion.38 Dr. Blair stated that there was “almost a complete loss of cutaneous sensation of the lower lip” but that the “sensation of the tooth-pulp is good.”38
Interestingly, Dr. Whipple, the treating dentist and orthodontist, published his version of the patient’s surgery, convalescence, and ultimate result in Dental Cosmos in 1897.212 This was before the journal publication by Dr. Blair, in which he gave a full account of the case from his perspective.38 Although Dr. Whipple’s description of events varied somewhat from what was eventually reported by Dr. Blair, both concurred that the procedure had taken place and that it was a success.
In his textbook, Dr. Blair cautions the surgeon that “the lower jaw should be set back only far enough to be in harmony with the rest of the face” and that the surgeon should “leave it to the orthodontist to bring forward the upper incisors if necessary.”40 He stated that “an orthodontist should be involved in the planning of the patient’s treatment from the beginning.”40 For some patients, Dr. Blair notes that “it would be of considerable advantage to have the upper jaw [orthodontically] expanded and the upper incisors and canines brought forward before the lower jaw is surgically set back.”40
A horizontal osteotomy through the ascending ramus, on each side and above the occlusal plane, as a method of “setting back” the prognathic mandible was first described by Lane.117 During the early 1900s, Blair39 and Babcock19 also made use of the horizontal ramus osteotomy on each side for the correction of prognathism.36
In 1912, Harsha reported bilateral wedge resections of the mandible body near the angle regions to set the mandible back; this was similar to the procedure that Blair described in 1897.89 Unfortunately, at least one of his reported patients suffered the loss of (and the eventual need to remove) the entire anterior part of the jaw. In 1945, Moose143 may have been the first to describe a fully intraoral technique to carry out horizontal ramus osteotomies for the correction of mandibular prognathism. In 1950, G.V. Barrow and Reed O. Dingman discussed the surgical management of mandibular prognathism.22 They described a method to determine the exact amount and shape of mandibular bone to be resected on each side by using dental models that involved the construction of splints and templates. Their described meticulous approach was similar to that of Angle in the 1903 edition of his textbook.7 The operation was reported by Dingman as having a two-stage approach71,72; this was to separate the intraoral and extraoral aspects to maintain control of the segments and to limit the risk of infection. During the first stage, the teeth to be extracted (i.e., the first molars) were removed with the use of local anesthesia. As determined by the “preconstructed template,” osteotomies for wedge resection were initiated through the intraoral approach at the time of the extractions. Approximately 4 weeks later, the patient was anesthetized in the operating room for the second stage. An incision of the skin of the neck was made 2 cm below the inferior border, and the lower aspect of the mandible was exposed on each side. The previous intraoral vertical cuts on each side were identified. With a power-driven bur or saw, the two vertical cuts were continued through the inferior border. Attempts to preserve the inferior alveolar nerve were made. Stabilization across the osteotomy on each side site was with 24-gauge stainless-steel wires. The teeth were placed into occlusion with the use of either orthodontic appliances or Erich arch bars. In either case, to improve accuracy, the mandibular dentition was secured into a prefabricated acrylic wafer before intermaxillary fixation occurred.
In 1954, J.B. Caldwell and G.S. Letterman devised a vertical osteotomy of the ascending ramus that involved the decortication and perforation of the fragments and then the splitting of the medial and lateral cortices of the ramus to allow for setback of the mandible followed by direct wire fixation.45,46 This innovative technique had the advantage of providing at least a degree of overlapping of the bone for more reliable and rapid healing.
All of these techniques for the management of mandibular prognathism79,87,91–93,96,138,167,211 eventually fell by the wayside after the introduction by Hugo Obwegeser of what we now refer to as the “intraoral sagittal splitting of the mandibular ramus,” which is described later in this chapter.149 The stabilization of the osteotomy segments is now generally accomplished with titanium bicortical screws or with a titanium plate and screws in accordance with the pioneering innovations of H. Luhr, who is also discussed in a later section of this chapter.127
Mandibular Advancement for Retrognathism
An important early maxillofacial textbook publication was Surgery and Diseases of the Mouth and Jaws by Vilray P. Blair (Fig. 2-21).40 At the time of publication, Dr. Blair was a Major in charge of the subsection of Plastic and Oral Surgery, Section of Surgery of the Head Office of the Surgeon General of the Army in Washington, DC.197 He was also a professor of oral surgery at the Washington University Dental School and an associate in surgery at the Washington University School of Medicine in St. Louis, Mo. In his textbook, Chapter 21 deals with the treatment of deformities and malrelations of the jaws.
Figure 2-21 Vilray P. Blair published a text entitled Surgery and Diseases of the Mouth and Jaws, the first edition of which was published by the C.V. Mosby Company in 1912.
• To not undertake any cases without first having the fullest confidence in his or her patient
• To remember that procedures undertaken for only “moderate” deformity should not be taken lightly
• To remember that maximum restoration will also require orthodontics
• To remember that the earlier a competent and genial orthodontist is associated with the case, the better it will be for both the surgeon and the patient
According to Dr. Blair, for the treatment of mandibular micrognathia, a surgical procedure may be used to “bring forward the lower jaw to harmonious outline” with the maxilla.40 Malocclusion in a patient with a jaw deformity results from the “pressure and counter pressure of growth and apposition.”40 Normal occlusion cannot be established by jaw surgery alone. To reach certain objectives, the surgeon “shall have knowledge of occlusion and of the scope and limitations of orthodontic procedures.”40
Blair went on to say this: “We have to accept the upper jaw position but the lower jaw is capable of almost any kind of surgical adjustment. The complication of an ununited fracture of the lower jaw is rare. The complication of necrosis or loss of teeth from surgically sectioning the ramus is not reported in the world literature.”40 However, “osteotomy of the ramus of the mandible is a recognized procedure for the treatment of temporomandibular joint ankylosis.”40 Esmarck, who was a prominent surgeon when Dr. Blair was discussing this treatment, recommended the removal of a whole section of the horizontal ramus to avoid a union (i.e., reankylosis) when creating a pseudoarthrosis for the treatment of temporomandibular joint ankylosis. However, Blair felt that surgeons did not need to concern themselves with the possibility of necrosis or nonunion when “completing an osteotomy through the inferior alveolar neurovascular bundle.”40
Blair felt that the surgeon could correct mandibular retrognathia by completing a ramus osteotomy on each side and then “bringing the distal mandible forward to meet a good occlusion with the maxillary arch.”40 Intermaxillary fixation could then be achieved with stainless steel wires and the use of soft cement in between the occluding teeth.40 Fixation across the osteotomy site was felt to be unnecessary. The (horizontal) ramus osteotomy was made at or just above the mandibular occlusal plane with the use of a Gigli saw placed transcutaneously.39 The osteotomy was cut through the inferior alveolar neurovascular bundle, which was not felt to be important either to the circulation of the mandible or as a cause of disability. The ramus osteotomies were later made blindly and transorally with a Gigli saw.40
According to Dr. Blair, “the operation presented three distinct problems: (1) the cutting of the bone [which is the easiest of the three]; (2) the placing of the jaw into its new position; and (3) holding it there [for the time required for healing].”40 He used postoperative x-rays to show that the fragments of the ramus remained in contact at the posterior border of the osteotomy. “[A]s the distal mandible is brought forward,” said Dr. Blair, “a gap is created anteriorly while the fragments remain in contact at the posterior border. For healing to occur, the bone gap must be filled with granulations. The resulting bone scar tends to contract [relapse] for months afterwards.”40 The maintenance of tight intermaxillary fixation was felt to be essential to maintain the new position. Blair used iron wire for its strength, lack of stretch, and pliability; it could also be twisted, unless it was damaged by sharp instruments.40 He also used quick-setting cement between the occlusal surfaces of the molars to prevent the placement of postoperative forces on the anterior teeth, which could cause the patient significant pain.40
Dr. Blair also used this same operation involving horizontal ramus osteotomies for the treatment of ankylosis associated with severe mandibular retrusion; this operation was first carried out by Dr. Mudd with Dr. Angle assisting in 1897. Dr. Blair also suggests addressing the residual chin deformity by either “injecting paraffin into the chin or by inserting a piece of cartilage or rib.”40
Most of the early reported attempts at horizontally advancing the retrognathic mandible focused on the mandibular body. Dr. Blair specifically addressed the problem of an anterior open bite by rotating the distal mandible counterclockwise after body osteotomies and ostectomies. He states that the “sectioning of the mandible on both sides in front of the first molars [as long as the molars are in occlusion] is the preferred procedure. The anterior mandible can then be moved into good occlusion with the upper teeth. In other cases, it is necessary to remove a V-shaped section of the bone on each side with extraction of the tooth [bicuspid]. The apex of the V-shaped ostectomy segment is at the lower border of the mandible and usually a tooth is extracted from the site of the section on each side. The bone is cut using a Gigli saw or a cross-cut Fisher bur.”40
Dr. Blair goes on to state that “the deformity is in both jaws but the operation is limited to the lower jaw. It is best to restore the lower jaw to its proper form and then manage the residual open bite by bringing down the upper incisors with orthodontic appliances or by extending the upper teeth with porcelain crowns. Fixation is achieved with a prefabricated splint constructed on plaster dental models. This will prevent pulling down of the distal segment by the digastric and geniohyoid muscles.”40
A variety of techniques were carried out by pioneering surgeons to address concerns regarding the maintenance of contact between the fragments to achieve bony union; soft-tissue coverage to limit infection; opposing muscle pull to limit relapse; and adequate fixation. In 1928, a “step osteotomy” of the body of the mandible was proposed by Von Eiselberg.201 Also in 1928, Gadd reported a stepped procedure for the body of the mandible for the purpose of correcting asymmetric mandibular deficiency.80 That same year, Limberg completed L-shaped sliding osteotomies of the mandibular body to improve bone-to-bone contact after advancement.122,123 In 1931, Kostecka published his work with the Blair-type transcutaneous horizontal ramus osteotomies with the use of a Gigli saw (Fig. 2-22).115 In 1936, Kazanjian performed mandibular “step” osteotomies anterior to the mental foramen with extension back into the body of the mandible to allow for advancement and fragment approximation (Fig. 2-23, A through D).68,103–108 The constant problems encountered with all of these approaches involved maintaining sufficient bone-to-bone contact and achieving adequate fixation for a stable long-term result. The problems were finally solved through the pioneering work of Hugo Obwegeser (i.e., the intra-oral sagittal splitting of the ramus of the mandible) and Hans Luhr (i.e., plate and screw fixation across the osteotomy site), which is described later in this chapter. In 1960, Caldwell described vertical osteotomies of the ramus with interpositional iliac bone graft for the correction of micrognathia.45 A C-osteotomy of the ramus was later described by Caldwell and colleagues, in 1968.46 Although these osteotomies with interpositional grafting are occasionally used for the management of mandibular retrognathism, the Obwegeser sagittal split ramus osteotomy is generally preferred. Throughout the 18th and 19th centuries, many surgeons saw the need to mobilize the maxilla for better access either to remove an epipharyngeal tumor or for the correction of maxillary deformity.
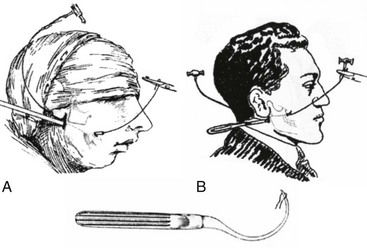
Figure 2-22 As originally depicted, methods for the correction of mandibular deformities by the blind technique. A, The method of Blair. From Blair VP: Surgery and diseases of the mouth and jaws, ed 3, St. Louis, 1914, C.V. Mosby Company. B, The method of Kostecka. From Kostecka F: Die chirurgische therapie der proggeni. Zahnaertzliche Rundschau 40:669–687, 1931.




Figure 2-23 A, Dr. Varaztad H. Kazanjian leaving Buckingham Palace after his investiture as a Companion of St. Michael and St. George for his services during World War I, March 15, 1919, B, View of the hospital showing Dr. Kazanjian’s three wards, circa 1916, C, Photograph of the hospital ward within the makeshift (Harvard unit) barrack where trauma patients were under the care of Varaztad H. Kazanjian (1915-1919). D, Photograph of Varaztad H. Kazanjian later in his career. A and B, From The Harvard Medical Library in the Francis A. Countway Library of Medicine. C, From Deranian HM: The miracle man of the western front. Bull Hist Dent 32:85-95, 1984.
Maxillary Osteotomies for Management of Dentofacial Deformity
In 1868, David Williams Cheever of Boston published a report of a Le Fort I osteotomy for the purpose of exposing and removing a large nasopharyngeal polyp (Fig. 2-24).55,88 After completing the tumor resection, the maxilla was placed back in its original location. Cheever stated, “so far as I know, the operation including both superior maxillary bones—is novel.”55 “Nothing but the posterior attachments of the upper maxilla now prevented their depression and hinging on the pterygoid processes. The upper jaw was brought down so as to expose the tumor.”55 By the early 1900s, reports of series of patients undergoing maxillary osteotomies for the purpose of tumor resection were detailed in the literature.37
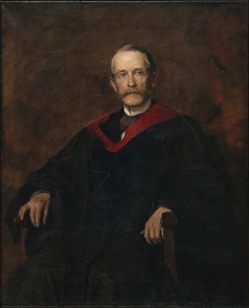
Figure 2-24 Photograph of David Williams Cheever of Boston (1831-1915). Courtesy Harvard University Portrait Collection.
With reference to the treatment of dentofacial deformities, in 1921 in Berlin, Cohn-Stock was the first to report an elective maxillary osteotomy to establish a preferred occlusion.56,214 He used a two-stage approach (a precaution against flap necrosis) when completing an anterior maxillary osteotomy. Martin Wassmund, the founder of the “German school” of maxillofacial surgery, is credited with developing the one-stage anterior maxillary osteotomy.205–207 The Wassmund procedure was completed through limited palatal and labial incisions with subperiosteal tunneling. The tunneling incisions limited mobilization, but this was thought to be necessary to maintain circulation. Karl Schuchardt is credited with developing the posterior maxillary segmental osteotomy.171–173 This was completed with the use of broadly elevated full-thickness palatal flaps and limited labial flaps. In 1959, Köle described the combined simultaneous maxillary and mandibular anterior segmental (alveolar) osteotomies for the correction of bimaxillary protrusion and other forms of open bite, deep bite, and posterior crossbite.111–114 He also pioneered the “corticotomy of maxillary and mandibular bones to facilitate the orthodontic movement of either a single tooth or group of teeth.”114
Wassmund is credited with performing a first “total maxillary osteotomy” for the correction of a dentofacial deformity in 1927.205–207 This was in a patient with an open-bite malocclusion. The maxillary osteotomy was completed through tunneling incisions without full down-fracture. Intermaxillary elastics were applied, with the gradual movement of the maxilla into occlusion occurring over the course of 2 weeks. In 1934, Axhausen was the first to mobilize and immediately reposition a malunited maxillary fracture by Le Fort I osteotomy.15–17 Pioneering surgeons described and continued to attempt maxilla osteotomies (anterior segmental, posterior segmental, and total maxillary) to improve the occlusion in individuals with dentofacial deformities.44,50,57–59,61,116,119–121,126,141,158,160,169,180,183,212,213,219,220 Unfortunately, circulation requirements of the maxillary segments were poorly understood, mobilization was often incomplete, and available fixation options were limited.66,86,87,110 These problems severely hampered the results that were possible for the patient with a jaw deformity.142,217
It was not until Hugo H. Obwegeser described the total horizontal Le Fort I osteotomy with complete down-fracture through a circumvestibular incision followed by full mobilization that the maxillary deformity could be universally addressed in all three planes, as described later in this chapter (Fig. 2-25).153 Animal research carried out in William H. Bell’s laboratory soon confirmed the vascular integrity of each specific dentoalveolar–musculomucosal mandibular and maxillary osteotomy-created flap that had been clinically described and used by Obwegeser and other European maxillofacial pioneers (Fig. 2-26).29 Experimental confirmation of the adequacy of the circulation to each of these flaps, when properly elevated, encouraged the rapid dissemination of knowledge and the incorporation of orthognathic procedures into maxillofacial clinical practice throughout the world; this is discussed in more detail later in this chapter.
Dr. Hans Luhr’s innovative ideas with regard to the development and clinical use of plate and screw fixation in maxillofacial surgery was the final piece of the puzzle, as described later in this chapter (Fig. 2-27).127–134 Interestingly, the third edition of Dr. Blair’s text, which was published in 1912, illustrates the use of what he calls “silver splints” for fixation across a mandibular osteotomy site (Fig. 2-28).40 He stated that the use of these fixation devices was essential for healing. The “silver splints” look much like the titanium mini-plates with screws that we use today. He states that the “silver splints” were used on a patient for the correction of mandibular prognathism.
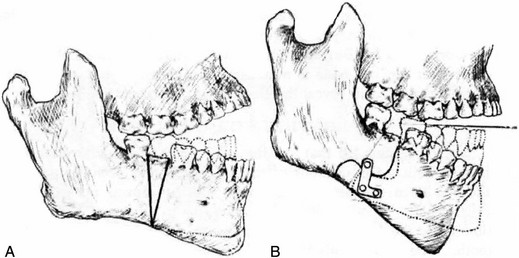
Figure 2-28 A, Open bite of an extreme type in a young man showing how correction may be made by with V-shaped excision. This would have the disadvantage of shortening the jaw considerably, as shown in the reconstructed jaw, which is indicated by the dotted lines. B, A demonstration of how an operation involving an S-shaped bone cut that lengthens the jawbone provides for the better closure of the mouth. The silver splints at the site of the bone-cutter are absolutely necessary. From Blair V: Surgery and diseases of the mouth and jaws, ed 3, St. Louis, 1917, C.V. Mosby Company, pp 309, Figures 287 and 288.
Hugo L. Obwegeser: Development of the Standard Orthognathic Procedures*
After completing his medical studies in mid 1945, Hugo Obwegeser started his career as an unpaid visiting doctor in a small hospital near his hometown. By doing so, he had the opportunity to assist with surgery, including the treatment of extremity fractures. He did not know at that point in what direction his medical training would lead him. His uncle, an orthopedic surgeon, gave him this advice: “Whatever you want to become, a general medical practitioner in a small town or a specialist in any field of medicine, you will always need a fundamental knowledge of pathology and pathophysiology.”156 Obwegeser listened to his uncle, and, in October 1945, he accepted an unpaid position training under Professor Chiari at the Rockitansky Institute of Pathological Anatomy at the University of Vienna. At first, Obwegeser watched and listened, and he was occasionally allowed to assist at the dissecting tables. After 1 year of general surgery training and 2 years of pathology training, he was offered a paid position to train in maxillofacial surgery under Richard Trauner at Graz University. At Graz, Obwegeser would also train in dentistry and sit for the Austrian dental qualification examination (dentistry in Austria was a subspecialty of general medicine). Obwegeser trained and worked with R. Trauner for 6 years. He saw professor Trauner both as a teacher and like a father.156 According to Obwegeser, Trauner “opened our eyes regarding the scope of the specialty [maxillofacial surgery] and stimulated us to see problems and find solutions for them.”156 The maxillofacial clinical practice at the Graz University Hospital included primary clefts, head and neck cancer, facial trauma, and the management of severe residual facial war injuries.
During that time and with a scholarship from the British Council, Trauner sent Obwegeser to Harold Gillies, the founder of modern plastic and reconstructive surgery (Fig. 2-29).81–85 Obwegeser observed and worked with Gillies from October 1951 to February 1952, primarily on the reconstruction of war cases. From Dr. Gillies, Obwegeser learned “how to plan the reconstruction of a facial defect and how to handle soft tissues.”156 Trauner also sent Obwegeser to spend time with Edward Schmid at Marien-Hospital in Stuttgart, where Obwegeser further advanced his knowledge of the handling of soft tissues, the movement of flaps to a new location, the management of cleft defects, and the closure of fistulas.156 During his career, Obwegeser was also influenced by Dr. Paul Louis Tessier (Fig. 2-30).184–196 Obwegeser states that, from Paul Tessier, he learned “the principal technique for advancing the whole middle third of the face and how to rotate the eye sockets into the planned position.”156 Tessier used these new techniques to correct posttraumatic or congenital anomalies of the upper half of the face. Tessier’s “cranial approach to the orbits via the anterior base of the skull has created the possibility of producing a normal appearance and with that a normal life for many patients”156; this is described later in this chapter.
In June 1966, Dr. Obwegeser broadly introduced his orthognathic surgery techniques to North American surgeons when he presented a series of invited lectures and demonstrations at a comprehensive conference sponsored by the American Society of Oral Surgery at Walter Reed Military Hospital in Washington, DC.156 At that time, Obwegeser also described other new ideas with broad implications for the scope of oral and maxillofacial surgery, including preprosthetic procedures, transoral approaches to the reduction of mandibular fractures, and the simultaneous resection and reconstruction of tumors of the mandible with the use of a transoral approach.150–155
According to Obwegeser, “With fundamental basic training in medicine and dentistry and through my teachers’ influence, I was able to produce new ideas and procedures, assemble them in contrast to the then existing rules. The influence of my teachers enabled me to become a teacher myself. It enabled me from 1958 until 1987 to establish the so-called Zurich-School of Maxillofacial Surgery.”156
The Transoral Sagittal Splitting of the Mandibular Ramus
Trauner R, Obwegeser H: Zur operationstechnik bei der progenia und anderen unterkieferanomalien. Dtsch Zahn Mund Kieferhlkd 23:11–25, 1955
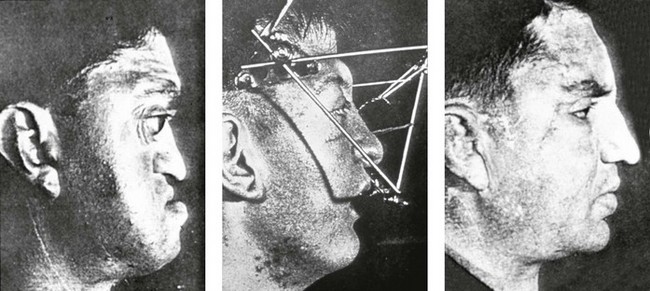
In 1947, Obwegeser started his training in maxillofacial surgery under the direction of Richard Trauner from the maxillofacial unit of the dental school at the University of Graz in Austria. At that time, orthognathic surgery was considered to be a series of unsatisfying procedures carried out primarily for the correction of prognathism. The available mandibular procedures were limited variations of horizontal ramus osteotomies. The basic techniques were those described by Blair38–41 and Kostecka115:
“The Blair-Kostecka technique included: The ascending ramus was cut on each side of the face [see Fig. 2-22]. The patient was placed in IMF [intermaxillary fixation] (6 to 8 weeks). It was estimated that approximately 50% of patients experienced significant complications including: partial or total relapse; residual malocclusion (open bite); pseudoarthrosis; injury to the facial nerve; injury to the inferior alveolar nerve; or parotid gland fistula. It was assumed that a primary reason for nonunion/malunion was the limited area of bone to bone contact across the osteotomy site once the distal mandible was placed in occlusion. This was compounded by contraction of the temporalis muscle of the non-fixed proximal segment causing further dislocation and separation. This complication was especially common when the procedure was used to correct mandibular deficiency as the distal mandible had to be advanced to achieve IMF [intermaxillary fixation].”156
In 1952, Dr. Obwegeser retrospectively reviewed a consecutive series (n = 36) of Dr. Trauner’s mandibular osteotomies that had been treated with the Blair-Kostecka approach.76,198–200 Obwegeser found a 50% incidence of significant complications. At his teacher’s request to look for a better way to solve the mandibular deformity problem, Dr. Obwegeser made a personal decision about two aspects. First, he felt that the extraoral (cutaneous) approach left an unpredictable quality of scar and added a risk of injury to the inferior alveolar (sensory) nerve and the facial (motor) nerve, so he chose to find an intraoral approach. Second, he believed that the available techniques produced inadequate bone-to-bone contact to ensure stable bony healing. A new approach would have to provide broad contacting bone surfaces, even after anterior mandibular repositioning from micrognathia.
Dr. Obwegeser studied the cadaver mandible and concluded that “the ramus could be split along its sagittal plane—with a broad bony surface area for healing.”156 He had noticed a sagittal pattern on the radiographs of mandibular fractures that he had seen, and he wondered if such a fracture could be purposely created by a surgeon. Obwegeser was certain that “the inner and outer cortex could be cut at different levels and [then] the two corticotomies [could be] reconnected along the sagittal plane.”156 He was also convinced that the intraoral approach would not in itself result in infection. He had treated mandibular fractures via an intraoral approach by repositioning the fragments and providing intermaxillary fixation within 24 hours of the injury, and he had found that this resulted in minimal complications.156
Obwegeser then set out to sagittally split the ramus transorally on a cadaver. He did his cadaver work at the Institute of Anatomy in Graz, Austria (Fig. 2-31). Professor Trauner, who was Obwegeser’s chief, then agreed to let Obwegeser try the new technique (i.e., intraoral approach sagittal split of the mandibular ramus) on a patient. Dr. Trauner would carry out his preferred approach (reverse L-shaped osteotomy of the ramus through a combined extraoral and intraoral approach) on one side, and Obwegeser would be allowed to try his technique on the other side. The procedure was carried out on an edentulous 27-year-old woman who presented with mandibular prognathism. A preoperatively constructed acrylic splint was made for the final occlusion, and the jaws would be wired together with the use of intermaxillary fixation (IMF). The procedure was carried out with the patient in a half-sitting position under local anesthesia on February 17, 1953. Unfortunately, when Obwegeser tried to execute his technique, the ramus “unexpectedly shattered instead of splitting.”156 The patient’s mandible was set back, the occlusion was secured with the acrylic splint, and IMF was applied. Healing was satisfactory.
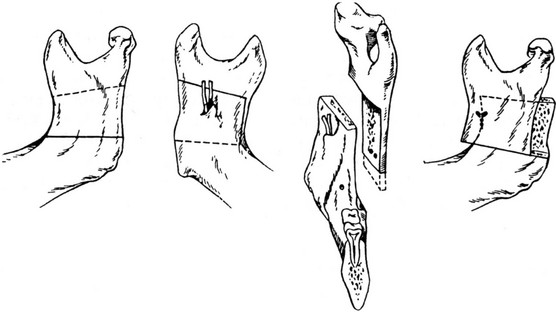
Figure 2-31 Illustration demonstrating the first sagittal splitting of the rami. From Trauner R, Obwegeser H: Zur operationstechnik bei der progenia und anderen unterkieferanomalien. Dtsch Zahn Mund Kieferhlkd 23:11–25, 1955.
Two months later, a 24-year-old woman with mandibular prognathism and a nearly full dentition presented. Dr. Trauner again agreed to allow Dr. Obwegeser to try his technique. On April 22, 1953, with the patient in a half-sitting position and under local anesthesia, Dr. Obwegeser completed his osteotomy using long Lindemann burs, a keyhole saw and a fissure bur to perforate the cortex, and then a rose bur to connect the cortical perforations. An osteotome was finally used to split the ramus. The coronoid process fractured off, but, “with a gentile twisting maneuver, the cortical plates fell apart and the ramus was sagittally split.”198 On the other side, Dr. Trauner performed his inverted L-shaped osteotomy through a combined oral and extraoral approach. “This was followed by six weeks of IMF. The recovery was uneventful.” The published result shows a favorable occlusion and good facial contour198 (Fig. 2-32).
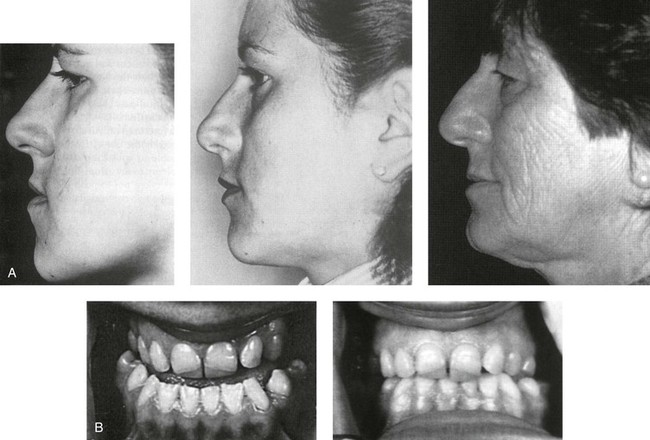

Figure 2-32 The patient shown underwent the first successful transoral sagittal split of the ramus on the left side. This operation was completed by Obwegeser. A transcutaneous inverted L osteotomy on the right side was completed by Trauner on April 22, 1953. A, Left profile views before surgery as well as 5 months and 22 years after the surgery. B, The patient’s occlusion before and after surgery is also shown. C, The posteroanterior cephalometric radiograph shows the wire fixation on the inverted L side (the right side) and without wire fixation on the sagittal split side (the left side). From Obwegeser HL: Orthognathic surgery and a tale of how three procedures came to be: a letter to the next generations of surgeons. Clin Plastic Surg 34:335, 2007, Figure 4.
Obwegeser recognized that additional problems to be overcome included the need for special instrumentation, intraoral lighting, and improved anesthesia. He joined the Department of Maxillofacial Surgery at the University Hospital in 1954. In 1956, Dr. Hotz, an orthodontist, asked Dr. Obwegeser to perform the “sagittal splitting procedure” on one of his patients.156 This patient was a 14½-year-old girl with a prognathic mandible who was partially maxillary edentulous.156 On April 9, 1956, with the patient under nasotracheal intubation, Dr. Obwegeser successfully completed the sagittal splitting of the ramus of the mandible on each side. On one side, the lateral ramus broke off, but it was secured back in place at the end of the procedure with direct wires. The operation took 4 hours, and healing was uneventful. According to the surgeons, “She had a wonderful aesthetic and functional result—no external scars”150 By the early 1960s, the sagittal splitting technique of the ramus of the mandible became routine for Dr. Obwegeser, and word soon spread worldwide.
Obwegeser mentions two important modifications to the sagittal splitting of the ramus of the mandible that later came about.151–153 The first modification was in “the placement of the lateral corticotomy to increase the surface area of the bony contact for improved union and to accommodate a wider range of advancement of the distal mandible.”156 The change was from a horizontal orientation of the lateral corticotomy of the ramus to a vertical orientation of the lateral corticotomy of the mandibular body. In 1957, while an observer of Dr. Obwegeser in Zurich, Dr. Dal Pont “conceived the idea of changing the lateral corticotomy from horizontal in the ramus to vertical in the body.”156 Dal Pont assisted Obwegeser with this goal, and it worked. In 1958, Dal Pont went back to his home base in Italy and eventually published these results himself.62,63 However, Dal Pont failed to mention that the patient described was Dr. Obwegeser’s patient. A second modification was also suggested by Dal Pont when he observed that, in some patients, the split did not go back all the way to the posterior border when the ramus was sectioned; satisfactory results nevertheless occurred.64 This second modification was also recommended by Hunsuck and Epker when they “advocated that the osteotomy of the lingual side should be incomplete, extending just past the entrance of the neurovascular bundle.”156 This would result in an incomplete fracture along the medial aspect of the ramus.65,67,77,78,99,136
The Transoral Sliding Osseous Genioplasty
Trauner R, Obwegeser H: The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg Oral Med Oral Pathol 10:677–689, 1957
Through the late 1950s, the correction of microgenia was achieved through onlay techniques to augment the deficient chin.13,14,102,140 The procedures were carried out through a submental (skin) incision. Autogenous bone and cartilage grafts (e.g., rib, hip) and a variety of alloplastic materials (e.g., acrylic, Silastic, metal) were used to augment the deficient chin. The onlay bone grafts resorbed over time. The cartilage grafts healed in a capsule and were often mobile and displaced, thereby causing asymmetry. The alloplastic materials, although easy to fabricate and place, had a high complication rate that included infection, displacement, the erosion of underlying bone, the resorption of the dental roots, and an unfavorable appearance.
Early in his career, Dr. Obwegeser had the intention of finding a reconstructive technique that would correct microgenia through an intraoral approach, that would allow for sufficient bone contact for reliable union, and that would maintain the advancement without resorption or relapse. After evaluating a woman with a retrusive chin and normal occlusion and reviewing her lateral cephalometric radiograph, Obwegeser realized that a favorable chin contour could best be accomplished by sectioning the chin transversely (i.e., below the roots of the teeth and the mental foramen) and then advancing it. He used the same transoral incision that he was familiar with from mandibular fracture management. He used a Lindemann bur to make a horizontal osteotomy below the roots of the teeth and the mental foramen, and he then completed the osteotomy with a chisel. He repositioned the distal chin horizontally forward by 10 mm while maintaining the geniohyoid muscle pedicle. He fixed the chin in its new position with circum-mandibular threads around the chin and bicuspid regions. The threads were primarily secured over a prefabricated acrylic wafer that was placed on the occlusal surfaces of the mandibular teeth to prevent “cheese wiring” through the interproximal regions. Obwegeser published this successful chin osteotomy outcome in 1957 (Fig. 2-33).150 Interestingly, an earlier publication by Hofer reported the sliding the inferior border of the chin forward.94,95 Although this osteotomy was similar to the one reported by Obwegeser, it was completed through an extraoral incision, and it was performed on a cadaver rather than a living patient. Over the decades, few useful clinical modifications of the original chin osteotomy (i.e., the Obwegeser technique) have been found in the literature. They include a double-step advancement and the splitting of the osteotomy in the midline to control width and angulation.150
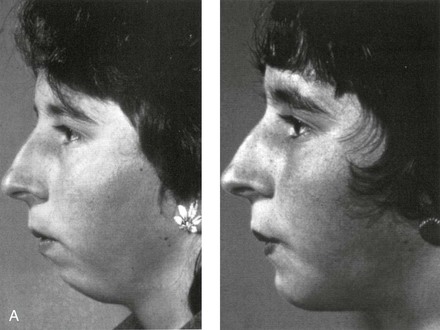
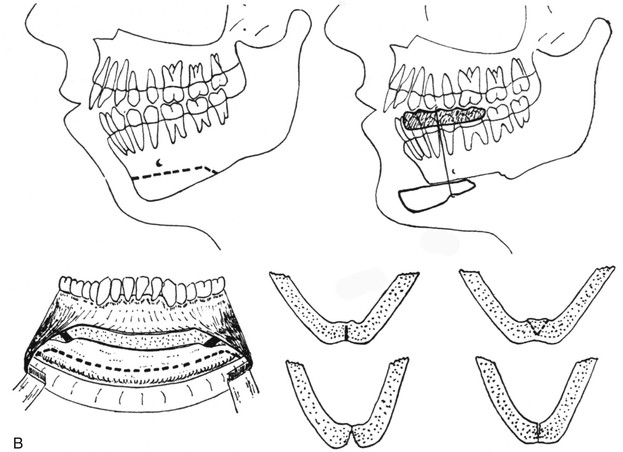
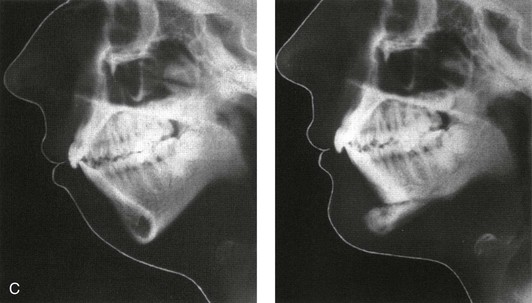
Figure 2-33 The first transoral approach of an osseous genioplasty to correct a chin deformity. A, Facial profile views before and after surgery. B, The transoral osseous genioplasty as illustrated in a 1957 article by Obwegeser. C, Lateral cephalograms before and after surgery. From Obwegeser HL: Surgical procedures to correct mandibular prognathism and reshaping of the chin. In Trauner R, Obwegeser H, editors: The surgical correction of the mandibular prognathism and retrognathia with consideration of genioplasty. Oral Surg Oral Med Oral Pathol 10:677–689, 1957.
The Le Fort I (Type) Osteotomy
Obwegeser H: Der offene biss in chirurgischer sicht. Schweiz Monatschr Zahnhlkd 74;668–687, 1964
Obwegeser knew that Langenbeck118 and Cheever55 were able to section the maxilla horizontally above the roots of the teeth through skin incisions of the cheek and lip for the purpose of gaining access to the posterior pharynx and the skull base. Wassmund reported that, in 1927, he had “detached the maxilla as a Guerin-type fracture” (personal communication) but without separating it from the pterygoid processes.205–207 He then used elastics (rather than a complete mobilization of the maxilla) to close the anterior open-bite malocclusion. Axhausen successfully completed osteotomies and repositioned the upper jaw in posttraumatic and cleft patients.15–17 He used elastics to relocate the maxilla after an osteotomy of the upper jaw, which included separation from the pterygoid processes but without complete intraoperative mobilization. In 1942, Schuchardt reported about a posttraumatic midface deformity caused by a war injury in which he completed a horizontal osteotomy of the maxilla above the roots of the teeth as a first procedure.171–173 Several weeks later, during a second operation, he fractured the pterygoid processes. After the second procedure, he used weight traction to horizontally advance the maxilla. He stated that “this procedure would have a large indication in cleft cases, but it would probably never come into use.”171–173 In 1951 and 1952, Obwegeser observed Sir Harold Gillies completing maxillary osteotomies to correct cleft maxillary deformities in numerous patients.156 Dr. Gillies “used horizontal vestibular incisions to approach the maxilla,” “but he only rotated the collapsed cleft segments with a Green-stick fracture at the pterygoid-maxillary junction.”156 This is similar to what Schmid reported in 1956 for the correction of posterior crossbites.170 According to Obwegeser, neither Gillies nor Schmid completed the horizontal maxillary osteotomies with the purpose of advancing the maxilla.156 Gillies and Rowe84 and Gillies85 did report that, in 1947, they had completed an osteotomy of the maxilla and were able to bring the upper jaw into the desired position in a patient with a cleft palate, with Gillies reopening the alveolar/palatal cleft and dividing the maxilla in two. This was followed by immobilization that lasted for 12 weeks. Gillies would secure the maxilla in its new location with the use of cast cap splints over the teeth that then attached to a vertical bar in front of the face and to a head cap. Gillies placed cancellous bone grafts on the steps (gaps) in the canine fossa regions and directly into the maxillary sinuses. Because of Gillies’ reticence to advance the maxilla, the horizontal discrepancy in the jaws had to be overcome by setting the mandible back. Unfortunately, the patients retained their “dish face” with, at best, a “flat appearance.”156
Throughout the 1950s, Obwegeser looked for solutions to correct the midface deformity seen in cleft and posttraumatic patients.137,159 He believed that vertical vestibular incisions—which were felt by most surgeons of the day to be necessary to maintain the maxillary blood supply—limited successful outcomes.156 He was convinced that the limited vertical vestibular mucosal incisions 1) prevented the full mobilization of the maxilla; 2) prevented the relaxed repositioning of the upper jaw in the operating room; and 3) prevented the placement of fixation and bone grafts, 4) thus further limiting the stability of the advancement and resulting in eventual relapse.
Obwegeser was able to innovate by making a quantum leap in the reconstructive possibilities of maxillary osteotomies for the correction of jaw deformities. In 1964, he was asked to treat an 18-year-old man who had been in a car accident 6 weeks earlier. The young man had sustained a fracture of the maxilla in two segments (palatal split), with telescoping occurring into the nose and the maxillary sinus. This resulted in a retropositioned maxilla with a severe anterior open bite. Three maxillary incisors were lost, there were multiple oronasal fistulas, and the vestibular mucosa had been lacerated circumferentially. There was initial healing of the soft tissues present, with scarring and malunion of the bones. To repair the deformity, Obwegeser realized that limited vertical vestibular incisions, which were part of his usual approach, were not feasible. He instead elected to reopen the circumferential vestibular incisions, also through the oronasal fistula opening (Fig. 2-34). He then completed a Le Fort I osteotomy through the two halves of the maxilla that had healed in malunion. This required horizontal osteotomies above the teeth from the canine fossa past the tuberosities and through the sinus on each side. He used osteotomies and a fissure-type bur on a rotary drill to complete the osteotomies. He raised the nasal mucosa, detached the septum, cut through the lateral nasal walls, and separated the pterygoid plates vertically. With each step, he confirmed that the vascularity to the dento-osseous–musculomucosal flap was not jeopardized. With finger pressure, the maxilla was disimpacted via the down-fracture technique. Obwegeser fully mobilized the maxilla to move it forward. He recreated the palatal fracture (segmentation) to independently reposition the two halves of the maxilla. He realized that the descending palatine arteries were no longer intact; while working through a circumvestibular incision, he was able to split the maxilla into two segments and to maintain the circulation to each half. He simultaneously closed the oronasal fistulas, fixed the maxillary segments in place, and established the preferred occlusion. By doing so, it was not necessary to complete mandibular osteotomies to correct the occlusion.
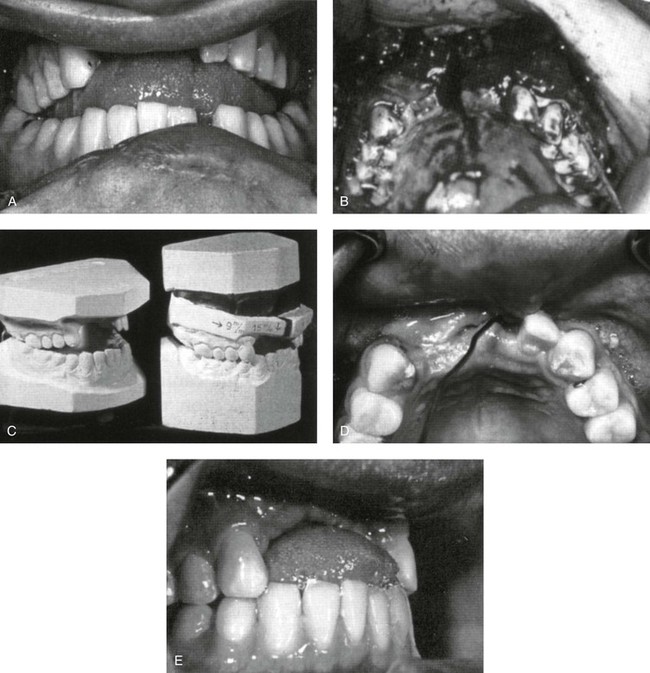
Figure 2-34 The first case of the advancement of the maxilla in two segments through a circumvestibular approach was performed by Obwegeser in 1964 to correct a posttraumatic deformity. A, A severe anterior open bite caused by posttraumatic telescoping retromaxillism in two segments. B, Oral-nasal communication and vestibular scarring on both sides. C, Model surgery indicating 9 mm of advancement and 15 mm of movement vertically down. D, Palatal view after reconstruction. E, The final occlusion after the complete mobilization of the two halves of the maxilla. From Obwegeser HL: Orthognathic surgery and a tale of how three procedures came to be: a letter to the next generations of surgeons. Clin Plastic Surg 34:341, 2007, Figure 10.
Over the next several years, Obwegeser succeeded in advancing the maxilla in cleft patients “without the need to establish the occlusion with a mandibular setback as in years past.”156 On April 14, 1968, he treated a patient with unilateral cleft lip and palate and a severe maxillary deficiency. Obwegeser advanced the lesser segment by 15 mm and the greater segment by 13 mm. The Le Fort I osteotomy was completed, and this was followed by down-fracture and mobilization. He recognized that “mobilization—release of scar tissue—and having both segments absolutely loose—was the entire key to success.” He realized that he could advance the maxilla as far forward as he needed to because he had a blood supply that was, surprisingly, still satisfactory.156 He then used blocks of cancellous bone from the iliac crest to fill the horizontal and vertical gaps.156
On September 5, 1969, Obwegeser completed the first simultaneous sagittal splitting of the ramus of the mandible and a Le Fort I osteotomy on a patient. He realized that he could establish the occlusion with either procedure and that he needed to vertically lengthen the mandible while at the same time setting it back. Thus, “both jaws had to be moved to improve the aesthetic result.”156 He used his clinical aesthetic judgment in combination with a review of a cephalometric radiograph to confirm what needed to be done. With the maxilla and the mandible completely freed up, he placed them into occlusion as a single unit. He then repositioned the maxillomandibular complex “according to [his] imagination.”156 When he was satisfied with the aesthetic result, he fixed the maxilla and then the mandible in place with wires and bone grafts. He maintained the patient in IMF for 6 weeks, after which he reported, “The occlusal and facial aesthetic results were excellent!”154
Only minor modifications have been introduced to the basic Obwegeser design of the maxillary Le Fort I osteotomy. According to Dr. Obwegeser, “In time, internal fixation with plates and screws became a reality. In 1968, Hans Luhr published his [initial] work with plate and screw fixation. It revolutionized internal fixation, limiting the need for extended IMF and increased [the osteotomy] stability.”156
William H. Bell: Experimental Studies to Confirm the Biologic Basis of the Standard Orthognathic Procedures*
William H. Bell attended a Jesuit high school, college, and dental school in St. Louis, Mo (Fig. 2-26), and he would be forever affected and influenced by the Jesuit challenge to “be men for others.” After completing dental school in 1954, he interned in oral surgery in New York City at the Metropolitan City Hospital. He recalls that “in any given week, [he] would literally see hundreds of patients who [were] candidates for either orthognathic surgery or orthodontics. Unfortunately, none of them received any treatment.”156 In 1955, he served as resident in oral surgery at the Jefferson Davis Hospital in Houston, Tex. Dr. Edward C. Hinds was the program director, and, at the time, it was considered one of the country’s finest programs in reconstructive mandibular surgery. Hinds had refined and clinically applied the extraoral vertical ramus osteotomy technique for the correction of mandibular prognathism. The program was also strong in the management of facial trauma, particularly mandibular and midface fractures. In 1956, Dr. Bell was the first teaching fellow in oral surgery at M.D. Anderson Hospital in Houston, Tex. His clinical work was limited to extracting teeth and the treatment of benign tumors and cysts of the jaws, but he had the opportunity to observe innovative head and neck cancer surgery. According to Dr. Bell, “Dr. Hinds and the other American oral surgeons in Houston were aware of descriptions of both anterior and posterior maxillary osteotomies, but none were performed for orthognathic problems at that time”(personal communication). Bell envisioned the potential of maxillary osteotomies for the correction of dentofacial and posttraumatic deformities. He searched the English literature available to him for relevant studies, but he found none that supported the biologic foundation of these procedures. Dr. Sumpter Arnim encouraged Bell’s interest in studying the circulation requirements of jaw osteotomies and offered experimental rabbits for use. After visiting the laboratories of orthopedic surgeons Drs. Rhinelander and Baraquay in Cleveland, Ohio, Dr. Bell performed a preliminary pilot study in rabbits to work out the details of microangiographic and histologic laboratory techniques (personal communication). This initial work gave support to these techniques for studying the biologic basis for jaw osteotomies. While at the University of Texas Dental Branch of the Texas Medical Center in Houston, Tex, and with support from U.S. Public Health Service grants, Dr. Bell carried out the first of his many revascularization bone-healing studies after completing maxillary and mandibular osteotomies with the use of adult rhesus monkeys, mongrel dogs, and baboons. In his first revascularization publication, Dr. Bell states the following: “Despite numerous clinical successes and occasional failures, the rationale for using various surgical techniques [for maxillary and mandibular osteotomies] remains virtually empiric. Basic questions concerned with the healing of the surgical wound produced by maxillary osteotomies and the vessels necessary to maintain blood supply to the bone segments and viability of the teeth have not been investigated.”24 Nine further animal laboratory studies would eventually be completed from 1969 to 1995, and these would validate the circulatory integrity of all of the basic osteotomies used in orthognathic surgery.25–35
In 1971, Dr. Bell was recruited by Dr. Robert Walker to the University of Texas Southwestern Medical Center in Dallas, Tex, to develop a research laboratory that focused on the vascularity and wound healing associated with maxillary and mandibular osteotomies (Fig. 2-35). This provided the opportunity to continue animal studies and to apply the knowledge gained in the laboratory to the solving of clinical challenges. For the next 20 years, he worked with and trained 27 oral and maxillofacial surgery residents in his research laboratory at the University of Texas Southwestern Medical School. He also conducted weekly dentofacial deformity conferences for surgical residents, faculty, and visitors from every corner of the world as well as for Dallas community orthodontists and surgeons. Beginning in 1973 and continuing through 1985, Dr. Bell, Dr. Raymond White, and Dr. William Proffit wrote and edited the text Surgical Correction of Dentofacial Deformities (Fig. 2-36). Volumes I and II of this text, which were published in 1980, became the comprehensive clinical reference for the interdisciplinary art and science of the correction of dentofacial deformities by surgeons and orthodontists. This work combined an atlas of surgical and orthodontic procedures with sound diagnostic and biologic guidelines for their application. The outstanding supporting original artwork by Bill Winn was remarkable for its clarity regarding the presenting dysmorphic maxillofacial anatomy and for its demonstration of how surgical procedures can be used to solve clinical problems.
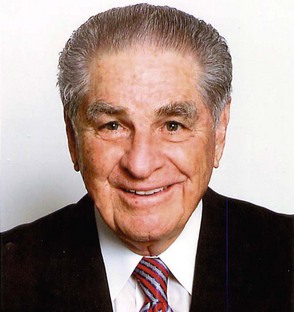
Figure 2-35 Photograph of Robert V. Walker (1924-2011). From Fonseca RJ, Barber D, Powers MP, Frost DE: Oral and maxillofacial trauma, ed 4, St. Louis, 2013, Saunders.
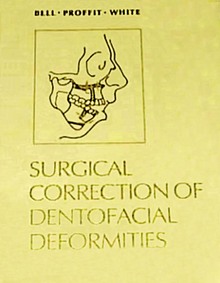
Figure 2-36 A textbook entitled Surgical Correction of Dentofacial Deformities, which was edited by W. Bell, W. Proffit, and R. White and which was published by W.B. Saunders in 1980. This was the first comprehensive textbook to cover the subject of orthognathic surgery.
Biologic Basis for the Maxillary Anterior Segmental Osteotomy
Bell WH: Revascularization and bone healing after anterior maxillary osteotomy: a study using adult rhesus monkeys. J Oral Surg 27:249–255, 1969
An investigation was designed by Bell and colleagues to delineate the biology of anterior maxillary osteotomy wound healing. This was done by studying revascularization and bone regeneration in monkeys with the use of microangiographic and histologic techniques after completing an anterior maxillary osteotomy. Standard anterior maxillary osteotomies (i.e., labial versus palatal pedicle) were completed with the Wassmund technique, and the animals were sacrificed at 1, 3, and 6 weeks after surgery. Before sacrifice, the common carotid arteries were exposed, cannulated, heparinized, and perfused with a suspension of Micropaque injection medium. Each maxilla was then dissected from the specimen, and radiographs were taken. The 1-week specimens confirmed a “blood clot in the center of the osteotomized fragments bounded by proliferating young granulation tissue.”24 The 3-week specimens “showed early callus formation between the bone fragments. Considerable subperiosteal new bone formation was present in some of the sections.”24 The 6-week specimens “showed osseous union of the osteotomized bone fragments with no evidence of necrosis.”24 According to Dr. Bell, “The results indicated that no single blood vessel, such as the incisive canal or greater palatine arteries, is essential to maintenance of circulation to the anterior maxillary fragment. Interosseous and soft tissue collateral circulation and the freely anastomosing gingival, palatal, floor of the nose and periodontal plexuses permit many variations of the anterior maxillary osteotomy technique [labial versus palatal pedicles] without detriment to the integrity of the blood supply to the anterior maxillary segment”24 (Fig. 2-37).
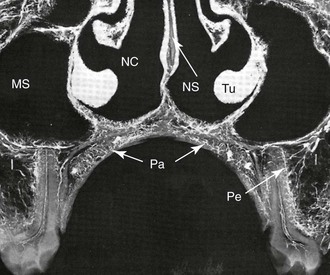
Figure 2-37 Microangiogram of a 1-mm transverse tissue slice from the molar region of a control animal. Areas are indicated as follows: palatal (Pa), maxillary sinus (MS), and nasal cavity (NC) blood vessels, penetrating bone and anastomosing with intramedullary blood vessels (I) and periodontal vascular plexus (Pe), turbinate (Tu), and nasal septum (NS). Courtesy William Bell.
Biologic Basis for the Anterior Mandibular Segmental Osteotomy
Bell WH, Levy BM: Revascularization and bone healing after anterior mandibular osteotomy. J Oral Surg 28:196–203, 1970
In 1970, Bell and Levy published an experimental animal study to analyze the biologic basis for wound healing and revascularization after anterior mandibular segmental osteotomy in adult rhesus monkeys (n = 11). Half of the experimental animals underwent a one-stage anterior mandibular segmental osteotomy that involved six teeth. The procedure was performed through a circumgingival degloving labial flap. The lingual soft-tissue pedicle remained attached to the osteotomized segment. Second bicuspids were extracted, and the mandibular anterior segment was set back. The second group underwent the same one-stage anterior mandibular segmental osteotomy, but this was performed through a labial vestibular incision with the maintenance of a gingival cuff around the labial aspect of the teeth. The lingual soft-tissue pedicle also remained attached to the osteotomized segment. The repositioned (set-back) anterior mandibular segment was stabilized with a prefabricated acrylic splint that was ligated to the teeth with interdental wires. The animals were sacrificed at specific postoperative intervals at weeks 1, 3, 6, and 24. Microangiograms and histologic slides were reviewed. The analysis of the data demonstrated that intraosseous and intrapulpal circulation to the anterior mandibular segments was maintained with the use of both of the surgical flap designs. The dento-osseous–musculomucosal flaps healed by osseous union within 6 weeks. In the control animals—in which the complete degloving of the labial and lingual soft tissues from the bone occurred—intraosseous necrosis, vascular ischemia, and nonunion resulted (Fig. 2-38).
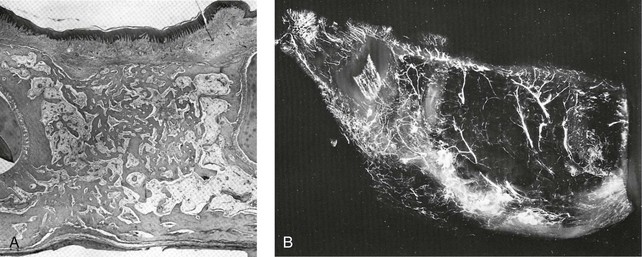
Figure 2-38 A, Photomicrograph of a section of the mandible of an animal 6 weeks after osteotomy. The osteotomy site is replaced by cancellous bone. Hematoxylin-eosin stain. Original magnification ×10. B, Microangiogram demonstrating the generalized distribution of injection medium throughout the anterior mandibular bone fragment 6 months after anterior mandibular osteotomy. Reconstitution of normal vascular architecture. Sagittal section. Courtesy William Bell.
Biologic Basis for the Posterior Maxillary Segmental Osteotomy
Bell WH, Levy BM: Revascularization and bone healing after posterior maxillary osteotomy. J Oral Surg 29(5):313–320, 1971
An animal model investigation was designed by Bell and Levy to clarify the biology of wound healing after posterior maxillary osteotomies with the Schuchardt technique (Fig. 2-39). In half of the posterior maxillary osteotomy flaps, the greater palatine vessel was ligated. The microangiographic and histologic studies were completed. At 1 week after surgery, the dento-alveolar segments remained freely movable. By 3 weeks, mobility had greatly diminished. After 6 weeks, the clinical union of the osteotomy segments was seen. The individual teeth and the mobilized bone segments remained stable. There was minimal osteonecrosis and only transient vascular ischemia, and osseous union between most of the osteotomized segments occurred. No difference was seen with or without the ligation of the palatine vessels. The results of the experimental study suggested that “clinically analogous single-stage posterior maxillary osteotomies are biologically sound.”26
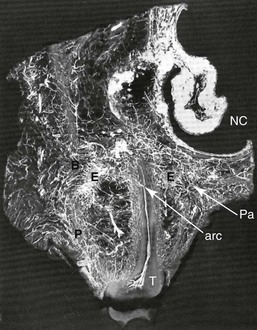
Figure 2-39 Microangiogram of 1-mm transverse tissue slice taken from the first molar region of an experimental animal 3 weeks after posterior maxillary osteotomy. This image demonstrates the proliferation of endosteal (E) and periosteal (P) circulatory beds; the reattachment of buccal and palatal mucoperiosteal flaps to underlying bone; and the vascularization of pulp canal from periodontal vascular plexus and accessory root canal (arc), buccal (B), and palatal (Pa) osteotomy sites; the nasal cavity (NC); and the first molar tooth (T). Courtesy William Bell.
Revascularization and Bone Healing after Maxillary Corticotomies
Bell WH, Levy BM: Revascularization and bone healing after maxillary corticotomies. J Oral Surg 30:640–648, 1972
In 1972, Bell and colleagues published an experimental animal study to analyze the biologic basis for revascularization and bone healing after maxillary interdental corticotomies with the use of the Köle technique (Fig. 2-40). Five adult rhesus monkeys underwent Köle type procedures and analysis. One-stage maxillary corticotomies were performed bilaterally in the premolar and incisor regions in four monkeys; one monkey served as a control. Corticotomies were completed in each dento-osseous segment. These segments were then mobilized by a chisel between the corticotomy sites, and the wounds were closed. The mobile segments were stabilized with a preoperatively made acrylic splint by ligating each tooth to the splint with interdental wires. The experimental monkeys were sacrificed at 1, 7, 21, and 63 days after surgery. Microangiographic and histologic slides were reviewed. The procedures that were carried out were found to have a destructive effect on the maxillary incisors. The intraosseous and interpulpal circulation also appeared to be imperiled.
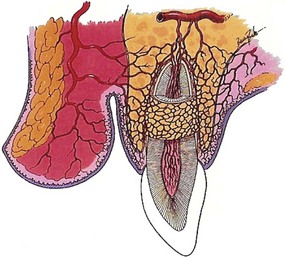
Figure 2-40 Illustration of blood supply to the anterior maxilla. The vascular architecture—which consists of freely anastomosing gingival plexus, palatal plexus, periodontal plexus, labial artery, intra-alveolar vessels, apical vessels, and pulp vessels—permits anterior maxillary osteotomies to be performed without compromising circulation to the anterior maxilla and the teeth. Courtesy William Bell.
Biologic Basis for the Le Fort I (Down-Fracture) Osteotomy
Bell WH, Fonseca RJ, Kenneky JW, Levy BM: Bone healing and revascularization after total maxillary osteotomy. J Oral Surg 33:253–260, 1975
In 1975, Bell and colleagues published an experimental animal study that confirmed the biologic basis for bone healing and revascularization after total maxillary (Le Fort I) osteotomy carried out through a circumvestibular incision followed by down-fracture and disimpaction via the Obwegeser technique. Twelve adult rhesus monkeys underwent single-stage total maxillary osteotomy according to Obwegeser’s protocol (Fig. 2-41). Two non-operated animals served as controls. In seven animals, the greater palatine arteries were preserved; in three animals, they were transected. The animals were sacrificed at the following intervals: immediately; after 2 days; and 1, 2, 4, 6, and 12 weeks after surgery. In all of the animals, the wounds healed without signs of infection or dehiscence. Revascularization and bone healing were studied with the use of microangiographic and histologic techniques (Fig. 2-42). Within 1 week after surgery, there was increased filling of both the endosteal and periosteal vascular beds. By 4 weeks, a callus that was composed of fibrous connective tissue and young bone was seen histologically. By 6 weeks, the callus contained mature bone. The 12-week specimen showed complete osseous bridging between fragments. Interestingly, the ligation of both greater palatine arteries had only minimal short-term effects on the perfusion of Micropaque through the intraosseous, intrapulpal, or soft tissues.
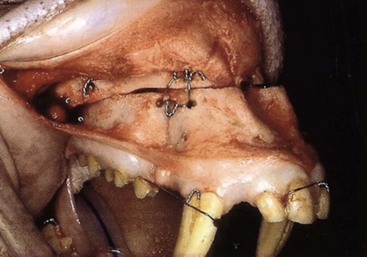
Figure 2-41 Clinically analogous pedicled down-fractured four-segment Le Fort I osteotomy technique performed in rhesus monkey. Courtesy William Bell.
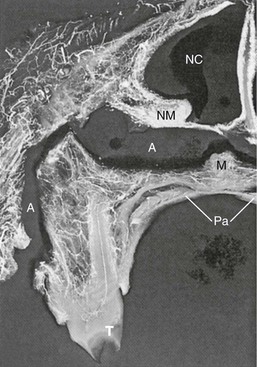
Figure 2-42 Microangiogram of the molar region of experimental animal 2 days after surgery, revealing generalized distribution of the injection medium in soft tissues, bone, and pulp canals of the molar (T) as well as an avascular space (A) between superior surface of the maxilla (M) and detached nasal mucosa (NM). Pa, Palate; NC, nasal cavity. Courtesy William Bell.
Biologic Basis for the Vertical Oblique Osteotomy of the Mandible
Biologic Basis for the Sagittal Split Osteotomy of the Mandible
Bell WH, Schendel SA: Biologic basis for modification of the sagittal ramus split operation. J Oral Surg 35:362–369, 1977
In 1977, Bell and Schendel published an experimental animal study to analyze the biologic basis for vascularization, revascularization, and bone healing in conjunction with sagittal ramus split procedures (Fig. 2-43). Ten adult rhesus monkeys were used. In each animal, on one side, the procedure was completed with complete subperiosteal stripping on the medial and lateral sides of the ramus osteotomy segment. On the contralateral side, the maximizing of the soft-tissue attachments on the medial and lateral side of the osteotomies was carried out. The animals were sacrificed at specific postoperative intervals (immediately or at 1, 2, 3, 6, 12, or 24 weeks). Microangiograms and histologic slides were reviewed at each time interval. The results of the experimental study confirmed that the Obwegeser technique of sagittal ramus osteotomy was biologically sound. Intraosseous ischemia and osteonecrosis were dramatically reduced when the mucoperiosteum and the pterygomasseteric sling were maintained to the repositioned proximal segment.
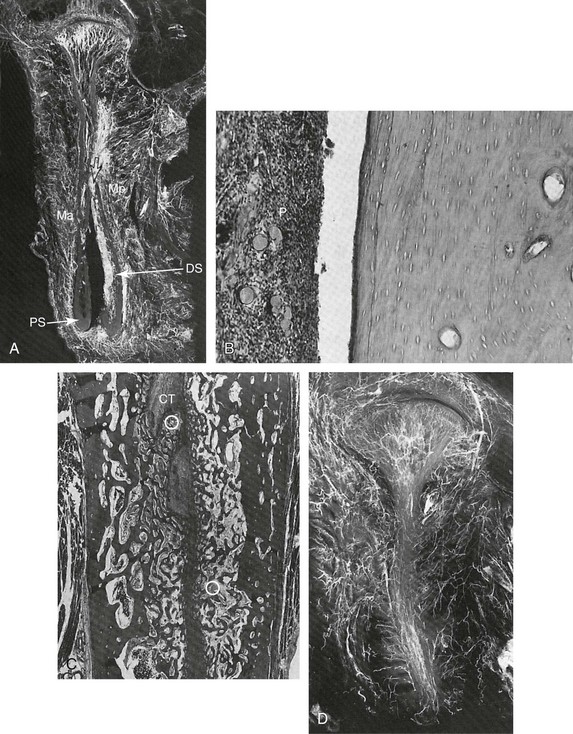
Figure 2-43 A, Microangiogram of a transverse section of vertical ramus 1 week after conventional sagittal split ramus osteotomy technique showing decreased perfusion of Micropaque into the distal region of the proximal segment (PS) and increased filling of the endosteal circulatory bed in the medial aspect of the distal segment (DS). Ma, Masseter muscle; Mp, medial pterygoid muscle. Arrows indicate the osteotomy site. B, Photomicrograph of the demarcated area of proximal segment showing detached periosteum (P) and subjacent avascular bone with empty lacunae. C, Histologic appearance of osteotomy site in the vertical ramus 6 weeks after modified sagittal split ramus osteotomy technique. There was some bridging of the proximal and distal bone segments with mature fibrous connective tissue (CT) and focal areas of viable vascularized osteophytic bone (O). D, Microangiogram of a 1-mm section through the ramus and condyle of a conventional saggittal split ramus osteotomy specimen 6 months after surgery showing vascular architecture similar to that seen in control animals. Courtesy William Bell.
Biologic Basis for a “One Tooth” Dento-Osseous Segmental Osteotomy
Bell WH, Schendel SA, Finn RA: Revascularization after surgical repositioning of one-tooth dento-osseous segments. J Oral Surg 36:757–765, 1978
In 1978, Bell, Schendel, and Finn published an experimental animal study to analyze the biologic basis for wound healing and revascularization after “one-tooth” dento-osseous segmental osteotomies in six adult mongrel dogs. Half of the experimental animals underwent a two-stage (single-tooth dento-osseous segment) approach, whereas the other group underwent a one-stage (single tooth dento-osseous segment) approach. The animals were sacrificed at specific postoperative intervals (3 days or 1, 3, 4, or 8 weeks). Microangiograms and histologic slides were reviewed. The data showed early transient vascular ischemia, minimal osteonecrosis, and osseous union between most of the osteotomized segments. The study parameters showed that necrosis occurred at a few of the interdental osteotomy sites. The authors stated that the “excessive removal of interseptal and interradicular bone may cause protracted bone healing and have a destructive effect on the periodontium.”33 The authors cautioned that the single-tooth dento-osseous segments were critically dependent on the preservation of viable circulation through the soft-tissue attachments to the underlying bone. This was by way of a freely anastomosing vascular plexus of the gingiva, the palate, the periodontium, and the dental pulp.
Biologic Basis for the Oblique Osteotomy of the Chin
Storum KA, Bell WH, Nagura H: Microangiographic and histologic evaluation of revascularization and healing after genioplasty by osteotomy of the inferior border of the mandible. J Oral Maxillofac Surg 48:210–216, 1988
In 1988, Storum, Bell, and Nagura completed microangiographic and histologic studies in adult rhesus monkeys. These studies indicated that an intra-oral pedicled genioplasty involving an osteotomy of the inferior mandibular border maintained circulation and osseous viability after the manipulation and repositioning of the chin segment (Fig. 2-44). Circulation to the dental pulp was not discernibly affected.182
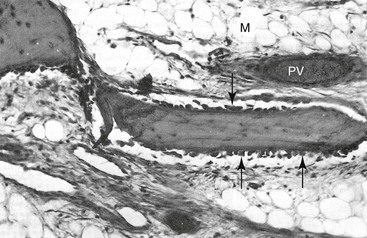
Figure 2-44 Biologic foundation for the use of an advancement osseous genioplasty with the maintenance of a soft-tissue pedicle. An adult Macaca nemestrina monkey was used as the experimental model. The genial segment was advanced 5 mm and fixed in the planned position with interosseous wires. This is a microangiogram of a 2.0-mm mid-sagittal tissue slice from an experimental animal that was sacrificed 1 week after advancement genioplasty. The photomicrograph shows vascularized and vital bone in the center of the genial segment. Proliferating osteoblasts (arrows) line viable trabecular bone, and bony lacunae are filled with osteocytes. Hematoxylin-eosin stain, ×125. M, Medullary space; PV, small perfused blood vessel. Courtesy William Bell.
Hans G. Luhr: Development of Plate and Screw Fixation for Craniomaxillofacial Surgery*
In 1963, Luhr began his training in maxillofacial surgery under the direction of Professor Karl Schuchardt. At that time, the Hamburg unit was considered the most prestigious in Germany. It was a regional maxillofacial trauma center, and, because Schuchardt had pioneered segmental osteotomies of the maxilla, there was much activity concerning jaw deformities with malocclusion. Schuchardt had also developed the acrylated arch bar, which was considered the treatment of choice for most mandibular fractures as well as for stabilization after elective mandibular osteotomies. Until Obwegeser described the Le Fort I down-fracture procedure with full mobilization, the Schuchardt method of horizontal Le Fort I osteotomy without pterygoid–maxillary disjunction was the procedure of choice. The incompletely mobilized maxilla was then managed by a “roll extension” and the application of 1.5 kg of weight via a sack of sand that was attached over the end of the hospital bed (Fig. 2-45). Disimpaction was gradual and occurred over a 2-week period. When the preferred occlusion was finally realized, the jaws were secured with IMF.
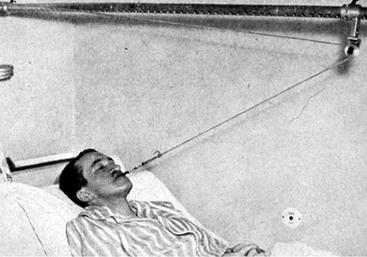
Figure 2-45 Roll extension with the application of 1.5 kg of weight on the side of the hospital bed. Disimpaction of the maxilla was gradual and occurred over a period of 2 weeks. Courtesy Hans Luhr.
Although it was clear that interosseous wire fixation was not rigid enough to counteract the masticatory muscle forces, it and other methods of fixation (e.g., plaster head cap with reinforced bar, palatal plate, cast cap splint, wire suture) were all that was known for the treatment of mandibular fractures and elective osteotomy stabilization (Fig. 2-46). Extended periods of IMF were also applied in an attempt to achieve healing. With these limited fixation and immobilization methods, complications such as osteomyelitis and nonunion frequently occurred, especially in the mandible. Skeletal wire suspension via the “belt-and-suspenders approach” had been introduced by Milton Adams in 1942 for the added stabilization of midface fractures, and this approach was later applied to elective jaw (orthognathic) osteotomies (Fig. 2-47).1 These suspension wires were occasionally supplemented by threaded Steinmann pins as clinicians searched for improved ways of establishing stable fixation. Long periods of IMF continued to be the workhorse of immobilization in an attempt to achieve bony union of the jaws. Prolonged periods of limited mouth opening had negative effects on speech, breathing, chewing, swallowing, hygiene, and temporomandibular joint mobility. As a resident in training, Dr. Luhr viewed these maxillofacial challenges with fresh eyes. Appreciating the limitations and hazards of these methods of immobilization and with background knowledge of what was known at the time about long bone fractures, he hypothesized that the addition of compression across a mandibular fracture would provide the necessary interfragmentary stability and eliminate the need for intermaxillary fixation. With research interests in the biomechanics of bone healing and jaw fracture management in particular, Luhr established an animal laboratory to study these issues. His experimental dog model involved a traumatically induced mandibular fracture. The fracture model confirmed that interfragmentary pressure created by a compression bone plate was at least partially maintained during the healing period (i.e., approximately 50% at 4 weeks). Further experiments by Luhr determined that the use of compression increased the rate of strength during fracture union as compared with fixation techniques without the use of compression. Interestingly, Luhr found that, with an actual fracture model, the histologic pattern of primary bone healing differed significantly from the descriptions by Schenk and Willenegger (i.e., Association for Osteosynthesis/Association for the Study of Internal Fixation investigators), who used a “saw-cut” tibia osteotomy dog model.129 During healing, these researchers observed the primary penetration of the osteotomy line via an ossification process that originated predominantly or exclusively in the cells and vessels within the Haversian canals. They termed this process intracanalicular osteogenesis, and they also called it contact primary bone healing. In their “saw-cut” tibia osteotomy dog model, the bone surfaces were in direct apposition to one another as fusion occurred. This was in contrast with “microgap healing,” which was described by Luhr in the mandible fracture model (Fig. 2-48, A). Luhr’s experimental model more closely simulated a real-life mandibular fracture. He found that the microscopic reduction of the fracture did not occur, despite the fact that the fracture appeared to the clinician to be grossly reduced. Small gaps still existed between the opposing bone spicular surfaces. Blood vessels and cells that originated in the endosteal cavity and in the periosteal side first invaded the microgaps between the opposing spicular surfaces. Lamellar bone was then deposited on the partially devitalized bone within the small interfragmentary gaps, and it soon filled up the microgaps and united the fracture segments (Fig. 2-48, B). As soon as 4 weeks later, the fracture was already clinically solid. The Haversian system contributed only to the late remodeling of the whole fracture zone, which could take several months. However, “gap healing” was seen with regularity, and it is viewed as a form of primary bone healing.
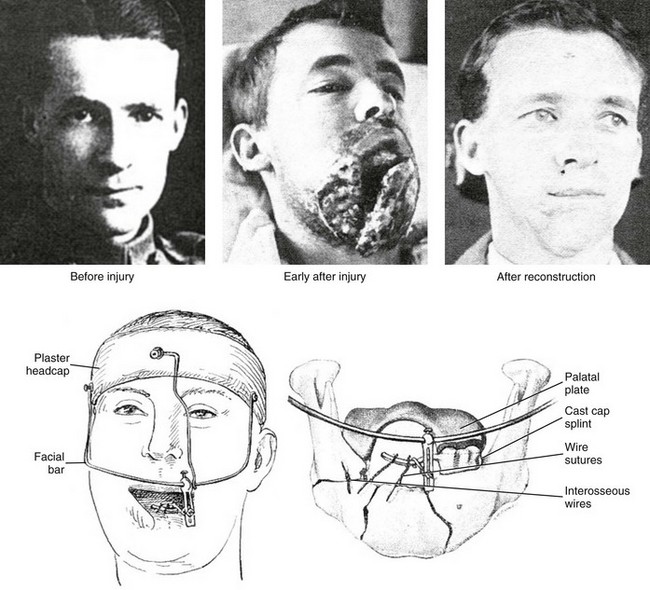
Figure 2-46 Kazanjian published an example of his management of a complex facial injury that was sustained by a soldier during World War I. The wound involved the soft tissues and skeletal structures of the face. Kazanjian used a combination of a plaster head cap, a facial bar, a palatal plate, cast cap splints, wire sutures, and interosseous wires to establish bony healing and soft-tissue maintenance. From Kazanjian VH, Converse EJ: The surgical treatment of facial injuries, Baltimore, 1949, The Williams and Wilkins Company.

Figure 2-47 An illustration of Adams suspension wires used to stabilize a midface fracture. In the past, this was a common method that was used in an attempt to immobilize a midface fracture.
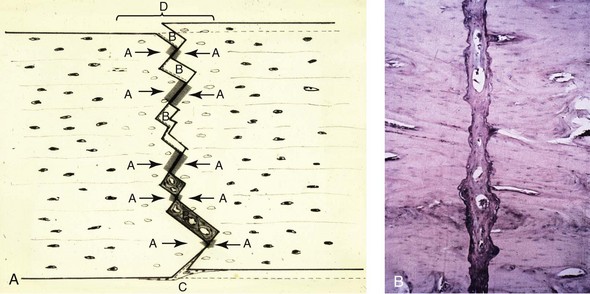
Figure 2-48 A, A schematic diagram of microgap healing at the microscopic level after the compression osteosynthesis of an experimental mandibular fracture in a dog. Although the fracture looks reduced at the time of surgery, microscopically, there were discrete areas of contact and separation between the fracture ends. The regeneration of bone took place in the non-contacting areas. Blood vessels had grown in both from the endosteal cavity and the periosteal side. Lamellar bone is deposited at the partially devitalized marginal fracture ends (C) with empty lacunae. B, Primary lamellar bone is deposited on the partially devitalized fracture ends around the blood vessels (cross-sectioned), which had grown in from the endosteal cavity and the periosteal side. This is a microscopic slide from 4 weeks after the compression osteosynthesis of an experimental mandible fracture in a dog. From Luhr HG: Callus symposion. Nova Acta Leopold 44:85–93, 1976.
After confirming its success in experimental animals, Luhr was the first to apply maxillofacial compression osteosynthesis in a human. He did this on an edentulous woman who had sustained bilateral body fractures in an atrophic mandible (Fig. 2-49).127 Within 6 months of this initial success, Luhr used similar compression osteosynthesis techniques on mandibular fractures in 16 additional patients, all with good results. He immediately saw the value of “self-tapping screws” in maxillofacial surgery. However, this went against the grain of general orthopedic surgeons, who at the time were beginning to use compression osteosynthesis for long bone injuries. They preferred to “pretap” the bone before the placement of fixation screws. Dr. Luhr chose Vitallium as a material, because it was a corrosive-resistant cobalt/chromium/molybdenum alloy with good strength. The small plates that he designed for use in the mandible were first modeled in wax, and they were then cast at a private dental lab. He would grind eccentric holes into each Vitallium fixation plate with the use of a diamond bur to complete the required design (Fig. 2-50). When drilling holes in the bone for the placement of self-tapping screws, Dr. Luhr initially used a hand-drill technique, because low-speed drills were not available in the operating room at that time. In 1968, Luhr reported on his initial consecutive series of mandibular fractures that involved the use of compression plating.127 The Luhr Maxillofacial Fixation System was then manufactured by Howmedica in 1969.133 Remarkably, all of the commercially available plate configurations in this system were designed by Luhr himself. He first completed pencil drawings to scale, and these served as design patterns for the manufacturer. This was true for all of the plating systems that Luhr introduced over the following two decades.
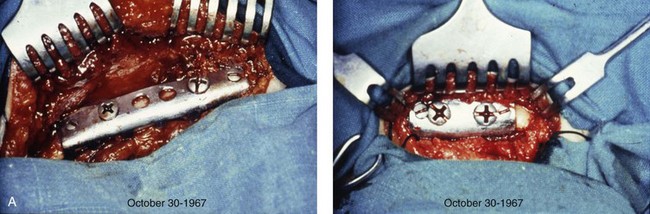
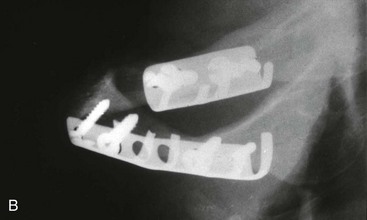
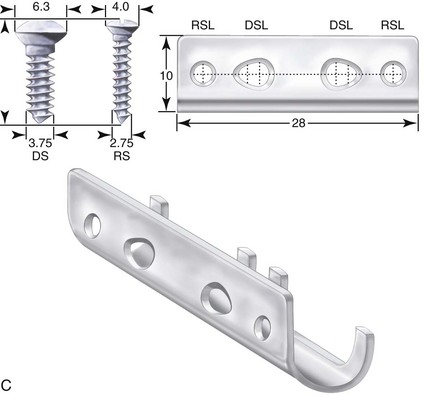
Figure 2-49 The first-ever compression osteosynthesis in maxillofacial surgery, which was performed by Luhr in 1967. A, An intraoperative view of the compression bone plates after the stabilization of bilateral body fractures of an edentulous mandible. B, A postoperative radiograph showing the fixation plates and screws that secured the reduced fracture. C, An illustration of the plate and screws (in millimeters) as designed by Luhr. Courtesy Hans Luhr.
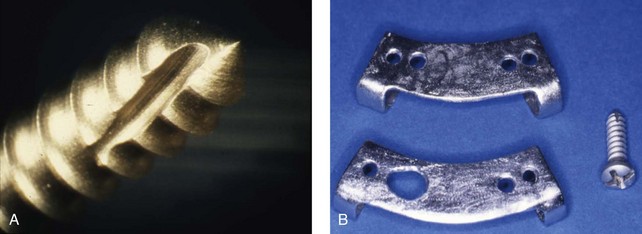
Figure 2-50 Self-tapping screw with a cutting flute is shown (A), along with an example of the raw plates that were cast for Dr. Luhr in Vitallium by a private dental lab (B). These plates were then refinished, and eccentric gliding holes were placed by Dr. Luhr with the use of a drill with a diamond bur. Courtesy Hans Luhr.
In January 1970, Dr. Luhr was presented with a patient who had been operated on elsewhere to correct a developmental jaw deformity that was characterized by mandibular prognathism. A Dingman osteotomy technique with interosseous wire fixation had been used, and this was followed by 12 weeks of IMF. The result was osteomyelitis with extraoral fistulas and nonunion on both sides (Fig. 2-51). Dr. Luhr initially removed the involved tooth at each osteotomy site and achieved drainage to manage the infection. He was able to stabilize each osteotomy site with the use of a compression plate with screws. A lower jaw arch bar was also left in place for 8 weeks to provide additional stability. With the stable direct fixation described, the intermaxillary fixation was immediately released, and healing was uneventful. This was likely the first case of plate and screw fixation used in orthognathic surgery. Although this case was not officially published by Dr. Luhr at the time, word quickly spread regarding this new technique of bone fixation for elective maxillofacial osteotomies.
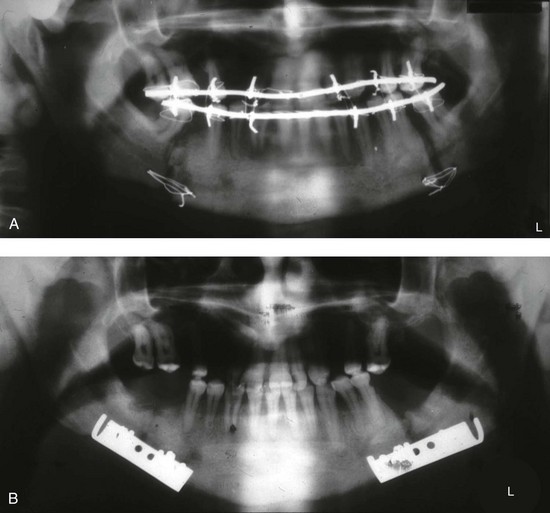
Figure 2-51 Osteomyelitis and nonunion resulted from a Dingman-technique osteotomy for the correction of mandibular prognathism, which included 12 weeks of intermaxillary fixation. A, A panorex radiograph is shown. B, The involved teeth were removed and drainage was achieved to manage the infection. Each of the osteotomy sites were stabilized with the use of a compression screw plate that was designed and placed by Dr. Luhr. Intermaxillary fixation was immediately released, and the final result after healing was uneventful. Courtesy Hans Luhr.
The advantages of plate and screw fixation for orthognathic surgery soon caught on. Francois Michelet and colleagues from Bordeaux, France, published their results involving mini-plate fixation of the Obwegeser sagittal split osteotomy in 1971.139 Two years later, mini-plate stabilization of elective maxillary osteotomies was also reported, with clear illustrations demonstrating how it should be done. Maxime Champy also described the use of mini-plates and monocortical screws for the treatment of mandibular fractures as well as the use of mini-plates and screws for elective Le Fort I osteotomies.52,53 Bernd Spiessl preferred the use of lag screw techniques to stabilize sagittal split osteotomies.176–178 He and others soon realized that, unless this technique was meticulously executed, the use of lag screws at the sagittal split osteotomy site could easily result in condyle dislocation with malocclusion as a result of the torquing effects. For the majority of surgeons, the philosophy of osteotomy fixation for sagittal splits soon shifted to the concept of “bicortical” (non–lag screw) technique in an attempt to avoid these complications. The so-called “positional screw” technique described by Lindorf124,125 and Niederdellmann146–148 gradually took hold. The potential risk of condyle dislocation with the application of mandibular osteotomy fixation during orthognathic surgery was recognized by Luhr.132 To help prevent this occurrence, he designed a temporomandibular joint positioning device, which remains a viable alternative to the freehand positioning approach that is most frequently used today (see Chapter 15).
Publications describing the value of mini-plate and screw fixation after Le Fort I osteotomy were initially described by Michelet139 and then by Champy,52,53 Hörster,97 Steinhäuser,179 and Drommer and Luhr (1981).73,74 Dr. Luhr reported on 17 cases of Le Fort I osteotomies using mini-plate and screw fixation specifically to correct the maxillary deformity in patients with cleft palates. During the late 1970s, the advantage of Dr. Luhr’s L-shaped mini-plates (specifically designed for the fixation of Le Fort I osteotomy sites) became known. The L-shaped plates overcame the difficulties of establishing fixation along the dense bicortical vertical pillars (i.e., the piriform rim region and the maxillary buttress) of the maxilla while also gaining maximum horizontal fixation directly above the roots of the teeth on the dentoalveolar side.
By the mid to late 1980s, the advantages of plate and screw fixation for use in a spectrum of elective craniofacial osteotomies, for fractures, and for tumor management was becoming known throughout the world. It was clear to Dr. Luhr that plates and screws of smaller dimension were required to accomplish clinical objectives, especially in the upper face. He designed the Luhr Micro-Fixation System, which is the smallest bone fixation system in the world; it includes screw diameters of as small as 0.8 mm and micro-plates of various design to match (Fig. 2-52).133 The system’s applicability to upper face clinical problems (e.g., cranial vault, orbit, zygomas, nose) was immediately clear and quickly adapted by craniofacial surgeons and neurosurgeons throughout the world.
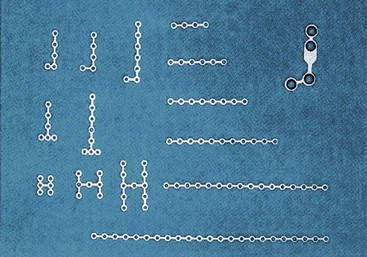
Figure 2-52 The first microplates designed by Dr. Luhr. A typical mini-plate from the time is shown in the upper right corner to demonstrate the difference in size. From Luhr HG: Indication for use of a microsystem for internal fixation in craniofacial surgery. J Craniofac Surg 1:36, 1990, Figure 2.
Until the 1980s, chin osteotomy via Obwegeser technique fixation was accomplished with interosseous wires or circumsymphyseal wires. Some clinicians also used threaded Steinmann pins. During the late 1980s, Dr. Luhr published articles about a series of genioplasties in which he used plate and screw fixation on a routine basis.134 There were few complications, and the clinical success was remarkable (Fig. 2-53). Dr. Luhr found the plate and screw fixation techniques for chin osteotomy stabilization to be especially useful when vertical lengthening and interpositional grafting were required. In 1988, Dr. Rosen also published a successful series of osseous genioplasties involving vertical lengthening with the use of Luhr (rigid) fixation.168
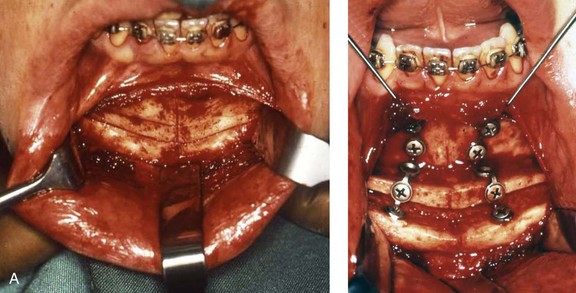
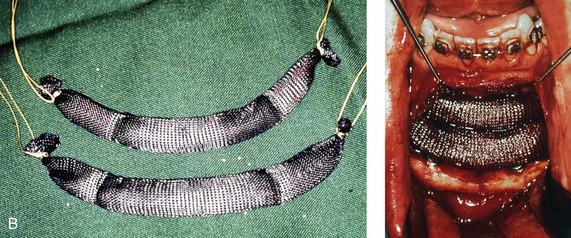

Figure 2-53 The advantage of plate and screw fixation is demonstrated via a double-step genioplasty that resulted in a 20-mm advancement. A, The two bony segments were stabilized with the use of two segmented mini-plates and screws. B, The steps were filled with hydroxyapatite granules that were packed into Vicryl sacks. C, Profile views of the patient before and after surgery. Courtesy Hans Luhr.
Throughout the 1960s and into the 1990s, Dr. Luhr stimulated a generation of craniomaxillofacial surgeons to embrace plate and screw fixation for trauma, elective osteotomies, and tumor management.127–134 Luhr’s initial ideas and commercially available fixation system served as a springboard for many of today’s craniomaxillofacial innovations. Stable plate and screw fixation is one of the most significant advances in craniomaxillofacial surgery to have occurred during the 20th century. On the basis of his laboratory research, technical innovations, and clinical contributions, it is right to consider Dr. Luhr “the father of rigid fixation.”
Paul Louis Tessier: Development of Craniofacial Surgery101,215,216
Paul Tessier (1917-2008) was born into a family of wine merchants in Héric on France’s Atlantic Coast (see Fig. 2-30). He was an only child, and he had no family background in medicine. It has been stated that his initial ambition was to join the Navy, but he was excluded from this by early ill health. Because of his love for the outdoors, he also considered a career in forestry. In 1936, at age 19, he entered medical school. However, just halfway through his studies, he became a prisoner of war in 1940. While he was interred, he became critically ill with a typhoid infection, but he eventually recovered. When he was released, he finally receiving his Doctor of Medicine degree from the Faculté de Médecine de Paris in 1943. When he came to Paris in 1944 (because the U.S. 8th Air Force had destroyed the hospital that he worked at in Nantes), Tessier worked with Maurice Virenque, a maxillofacial surgeon, at Hôpital Puteauz. After the war, the service moved to Foch, where there were, in essence, two maxillofacial services: one with Virenque and Tessier and one with Gustave Ginestet, an officious martinet who held the rank of General in the French Army. After Virenque died, Ginestet wrote Tessier several letters forbidding him to perform any maxillofacial surgery; his only function was to be running the burn service. Tessier ignored Ginestet, but many of his methods of interlocking bone fixation were the result of the fact that Ginestet controlled the dental lab and forbade the technicians to provide any help to Tessier. Jacques Dautrey, who was Tessier’s friend but who was also on Ginestet’s service, used to sneak in to help Tessier.
Between 1946 and 1950, Dr. Tessier made yearly visits to England to observe Harold Gillies, Archibald McIndoe, and others whose advances in plastic surgery in response to severe military injuries were ongoing. Through his observations and his passion to find solutions to complex reconstructive problems, Dr. Tessier began to find innovative ways to perform osteotomies for the correction of congenital midface retrusion but without the problems that had plagued the performance by his mentor Harold Gillies. By the mid 1950s, Tessier had become the head of his department in Paris. He was consulted in 1957 by a young man with a facial deformity of “monstrous aspect” who was found to have Crouzon syndrome.186 The patient’s facial deformities included severe orbital dystopia/eye proptosis, midface deficiency/malocclusion, and obstructed breathing. Dr. Tessier was aware that Gillies had completed an elective Le Fort III osteotomy on a young adult with Crouzon syndrome who had a moderate degree of proptosis and midface deficiency (Fig. 2-54). Dr. Gillies was reported to be discouraged with the eventual outcome and had recommended to others “never to do it.”82
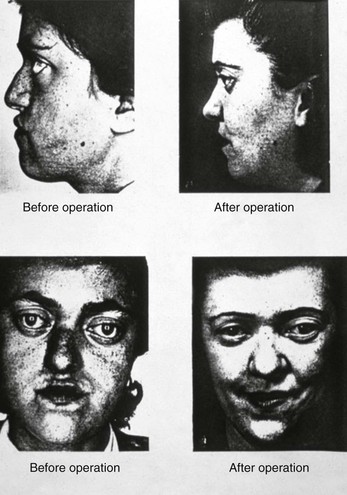
Figure 2-54 Gillies published the results of a Le Fort III osteotomy that was completed in 1942 for an adult with Crouzon syndrome. From Gillies H, Harrison SH: Operative correction by osteotomy of recessed malar maxillary compound in case of oxycephaly. Br J Plast Surg 3:102, 1950.
Tessier was undeterred, and he set out to solve the problem initially by performing an anatomic study of dry skulls. For access to the anatomy laboratory, he traveled by train in the evenings to his medical school in Nantes. After his late-night cadaver dissections, he returned during the early hours for the next Parisian working day. His painstaking preparatory work paid off when he successfully advanced his patient’s face by 25 mm and achieved stability with the novel use of bone grafts (which Gillies had not used), improved osteotomy design, incision placement, and immobilization techniques, including use of an external fixation apparatus (Fig. 2-55).
The surgical procedures developed by Tessier were shown to the world at a presentation that he made in Rome at the International Plastic Surgery Meeting in 1967.187 The techniques were so revolutionary that Tessier sought to establish their validity before continuing further. In the most humble and unique way, Tessier invited prominent surgeons from around the world to observe him operating live so that he could demonstrate these techniques before a distinguished international group of his peers. He asked for their vote on whether his demonstrated surgical techniques had a place in the practice of surgery. The resounding positive responses of his peers were clear evidence of their support and approval. During the late 1960s and throughout the 1970s, Dr. Tessier developed all of the basic procedures and essential techniques that are currently used to perform what has come to be known as craniofacial surgery, including the transcranial and subcranial correction of orbital dystopia such as orbital hypertelorism; the correction of midface deficiency or deformity among patients with conditions such as Crouzon syndrome and Apert syndrome; the correction of facial deformities associated with such conditions as Treacher Collins–Franceschetti syndrome; and the description and correction of the spectrum of oro-ocular clefts. The impact of Dr. Tessier’s work has affected every surgical specialty that seeks solutions to head and neck problems, including plastic surgery, otolaryngology/head and neck surgery, ophthalmology, neurosurgery, trauma surgery, and oral and maxillofacial surgery.
By the late 1960s, Paris become the birthplace of the new specialty of craniofacial surgery, where visitors would flock to observe Tessier’s techniques and approach to problem solving. Dr. Tessier began traveling to the United States and England to demonstrate his procedures in cities such as Philadelphia, Chicago, Kansas City, Houston, Boston, Norfolk, and London.185 Dr. Tessier’s work became so far reaching that, by the 1990s, virtually everyone performing craniofacial procedures was either trained by Dr. Tessier himself or by surgeons whom he had trained.
Dr. Tessier’s contributions cannot be overestimated.184–196 His basic innovations to safely separate the orbits and the midface from the base of the skull with the use of an intracranial approach satisfy the needs for exposure during complex surgery and craniofacial reconstruction. His techniques have revolutionized the treatment of birth defects of the head and neck; tumors of the midface, orbit, and skull base; severe facial deformities and asymmetries; craniofacial trauma; and complex infections. In response to questions about what inspired his unique approach to problem solving, Tessier would quote Guiot’s response: “Pourquoi pas?” This phrase—which is translated into English as “Why not?”—became the motto of the International Society of Craniofacial Surgery, founded in 1983, of which Tessier was invited to be Honorary President.
References
1. Adams, WM. Internal wiring fixation of facial fractures. Surgery. 1942; 12:4.
2. Andrews, LF. The six keys to normal occlusion. Am J Orthod. 1972; 63:296–309.
3. Andrews, WA. Andrews. Journal of Orthodontics and Orofacial Harmony. 2000; 1(1):1–56.
4. Andrews, WA. Andrews. Journal of Orthodontics and Orofacial Harmony. 2001; 1(2):1–60.
5. Angle, EH. Double resection of the lower maxilla. Dent Cosmos. 40(July-Dec), 1898.
6. Angle, EH. Treatment of malocclusion of the teeth and fractures of the mandible: Angle’s system. Philadelphia: White Dental Manufacturing; 1900.
7. Angle, EH. Double resection for the treatment of mandibular protrusion. Dent Cosmos. 1903; 45:268.
8. Angle, JL. Greek teeth: ancient and modern. Hum Biol. 1944; 16:283–297.
9. Asbell, MB. Bicentenary of a dental classic: John Hunter’s natural history of the human teeth. J Am Dent Assoc. 1972; 84:1311–1334.
10. Asbell, MB. A brief history of orthodontics. Am J Orthod Dentofacial Orthop. 1990; 98:176–183.
11. Asbell, MB. Simeon Hayden Guilford (1841-1919). Am J Orthod Dentofacial Orthop. 113(367), 1998.
12. Asbell, MB. John Nutting Farrar 1839-1913. Am J Orthod Dentofacial Orthop. 114(602), 1998.
13. Aufricht, G. Combined nasal plastic and chin plastic: correction of microgenia by osteocartilaginous transplant from large hump of nose. Am J Surg. 1934; 25:292.
14. Aufricht, G. Combined plastic surgery of the nose and chin. Am J Oral Surg. 1958; 95:231.
15. Axhausen, G. Zur Behandlung veralteter disloziert geheilter oberkieferbruche. Dtsch Zahn Mund Kieferheilkd. 1934; 1:334.
16. Axhausen, G. Ueber die korrigierende osteotomie am oberkiefer. Dtsch Z Chir. 1936; 248:515–522.
17. Axhausen, G. Die operative orthopädie bei den fehlbildungen der kiefer. Dtsch Zahn Mund Kieferhlkd. 1939; 6:582–600.
18. Aziz, SR, Simon, P. Hullihen and the origin of orthognathic surgery. Oral Maxillofac Surg. 2004; 62:1303–1307.
19. Babcock, WW. Surgical treatment of certain deformities of the jaw associated with malocclusion of the teeth. JAMA. 1909; 53:833.
20. Baker, CR. Orthodontic profiles. Am J Orthod. 1957; 43:210–218.
21. Barton, JR. Systemic bandage for fracture of the lower jaw. Am Med Rec. 1819; 2:153.
22. Barrow, GV, Dingman, RO. Orthodontic considerations in the surgical management of developmental deformities of the mandible. Am J Orthod. 1950; 36:121–124.
23. Begg, PR. Stone age man’s dentition. Am J Orthod. 1954; 40:298–312.
24. Bell, WH. Revascularization and bone healing after anterior maxillary osteotomy: a study using adult rhesus monkeys. J Oral Surg. 1969; 27:249–255.
25. Bell, WH, Levy, BM. Revascularization and bone healing after anterior mandibular osteotomy. J Oral Surg. 1970; 28:196–203.
26. Bell, WH, Levy, BM. Revascularization and bone healing after posterior maxillary osteotomy. J Oral Surg. 1971; 29:313–320.
27. Bell, WH. Correction of skeletal type of anterior open bite. J Oral Surg. 1971; 29:706.
28. Bell, WH, Levy, BM. Revascularization and bone healing after maxillary corticotomies. J Oral Surg. 1972; 30:640–648.
29. Bell, WH, Fonseca, RJ, Kenneky, JW, Levy, BM. Bone healing and revascularization after total maxillary osteotomy. J Oral Surg. 1975; 33:253–260.
30. Bell, WH. Le Fort I osteotomy for correction of maxillary deformities. Oral Surg. 1975; 33:412–426.
31. Bell, WH, Kennedy, JW. Biologic basis for vertical ramus osteotomies—a study of bone healing and revascularization in adult rhesus monkeys. J Oral Surg. 1976; 34:215–225.
32. Bell, WH, Schendel, SA. Biologic basis for modification of the sagittal ramus split operation. J Oral Surg. 1977; 35:362–369.
33. Bell, WH, Schendel, SA, Finn, RA. Revascularization after surgical repositioning of one-tooth dento-osseous segments. J Oral Surg. 1978; 36:757–765.
34. Bell, WH, Mannai, C, Luhr, HG. Art and science of the Le Fort I downfracture. Int J Adult Orthod Orthognath Surg. 1988; 3:23.
35. Bell, WH, You, ZH, Finn, RA, Fields, RT. Wound healing after multisegmental Le Fort I osteotomy and transection of the descending palatine vessels. J Oral Maxillofac Surg. 1995; 53:1425–1433.
36. Biederman, W. The strange story of the Angle operation. Ann Dent. 1956; 15:115.
37. Bier, A, Braun, A, Kummel, H. Chirurgische operationslehre. Band I. Leipzig, Germany: Barth; 1914.
38. Blair, VP. Report of a case of double resection for the correction of protrusion of the mandible. Dent Cosmos. 1906; 48:817–820.
39. Blair, VP. Operations on the jaw-bone and face. Surg Gynecol Obstet. 1907; 4:67–78.
40. Blair, VP. Surgery of the mouth and jaws. St. Louis: Mosby; 1914.
41. Blair, VP. Instances of operative correction of malrelation of the jaws. Int J Orthod. 1915; 1:395.
42. Brodie, AG. Orthodontic history and what it teaches. Angle Orthod. 1934; 4:85–97.
43. Brodie, AG. Orthodontic concepts prior to the death of Edward H Angle. Angle Orthod. 1956; 26:144–154.
44. Cadenat, H, Aussenac, R, Barthélémy, I, Combelles, R. Le maxillaire supérieur, facteur de prognathie inférieur. Rev Stomatol Chir Maxillofac. 1971; 72:527–530.
45. Caldwell, JB, Letterman, GS. Vertical osteotomy in the mandibular rami for correction of prognathism. J Oral Surg. 1954; 12:185.
46. Caldwell, JB, Hayward, J, Lister, R. Correction of mandibular retrognathia by vertical L-osteotomy: a new technique. J Oral Surg. 1968; 26:259.
47. Case, CS. Principles of occlusion and dentofacial relations. Dent Items Int. 1905; 27:489.
48. Case, CS, A practical treatise on the techniques and principles of dental orthopedia and prosthetic correction of cleft palate. ed 2, 1922.
49. Casto, FM. A historical sketch of orthodontia. Dent Cosmos. 1934; 76:111–135.
50. Cernea, Grignon, Crépy, Benoist. Les osteotomies totales de maxillaire superieurs. Rev Stomatol. 1955; 56:700–716.
51. Chadwick, J, Mann, W. The medical works of Hippocrates. London: Blackwell Scientific; 1950.
52. Champy, M, Lodde, JP, Wilk, A, Grasset, D. Plattenosteosynthesen bei mittelgesichtsfrakturen und osteotomien. Dtsch Z Mund-Kiefer-u Gesichts-Chir. 1978; 2:26–36.
53. Champy, M. Surgical treatment of midface deformities. Head Neck Surg. 1980; 2:451–465.
54. Chapman, H. Orthodontics: Fifty years in retrospect. Am J Orthod. 1955; 41:421–442.
55. Cheever, DW. Displacement of the upper jaw. Med Surg Rep Boston City Hosp. 1870; 1:156.
56. Conn-Stock, G. Die chirurgische immediate—gulierung der kiefer, speziell die chirurgische behandlung der prognathie. Vjscher Zahnhkd. 1921; 37:320.
57. Converse, JM, Shapiro, H. Treatment of developmental deformations of the jaws. Plast Reconstr Surg. 1952; 10:473–510.
58. Converse, JM, Wood-Smith, D. Horizontal osteotomy of the mandible. Plast Reconstr Surg. 1964; 34:464.
59. Converse, JM, Horwitz, SL. The surgical orthodontic approach to the treatment of dentofacial deformities. Am J Orthod. 1969; 55:217–243.
60. Cryer, M. Typical and atypical occlusion of teeth. Dent Cosmos. 1904; 46:713.
61. Cupar, I. Die chirurgische behandlung der form und stellungs veranderungen des oberkiefers. Ost Z Stomatol. 1954; 51:565.
62. Dal Pont, G. L’osteotomia retromolare per la correzione della progenia. Minerva Chir. 1958; 1:369–371.
63. Dal Pont, G. L’osteotomia retromolare per la correzione della progenia. Minerva Chir. 1959; 14:1138–1141.
64. Dal Pont, G. Retromolar osteotomy for the correction of prognathism. J Oral Surg Anaesth Hosp D Serv. 1961; 19:42–47.
65. Delaire, J. De l’interet des osteotomies sagittales dans la correction des infragnathies mandibulaires. Ann Chir Plast. 1970; 15:104.
66. Delaire, J, Verdon, P, Lumineau, J, et al. Quelques resultats des tractions extra-orales B appui fronto-mentonnier dans le traitement orthopedique des malformations maxillomandibulaires de classe III et des sequelles osseuses des fentes labio-maxillaires. Rev Stomatol (Paris). 1972; 73:633.
67. Delaire, J. Sagittal splitting of the body of the mandible (Mehnert’s technique) for correction of open bite and deep over bite. J Maxillofac Surg. 1977; 5:93.
68. Deranian, HM. The miracle man of the Western Front; the story of Dr. Varaztad Kazanjian. Bull Hist Dent. 1984; 32:85–95.
69. Dewel, BF. The Case-Dewey-Cryer extraction debate. Am J Orthod. 1964; 50:862–865.
70. Dewel, BF. The ribbon arch: its influence in the development of orthodontic appliances. Angle Orthod. 1981; 51:263–268.
71. Dingman, RO. Surgical correction of mandibular prognathism: an improved method. Am J Orthod Dentofacial Orthop. 1944; 30:683.
72. Dingman, RO, Harding, RL. The treatment of malunited fractures of the facial bones. Plast Reconstr Surg. 1951; 7:505–519.
73. Drommer, R, Luhr, HG. The stabilization of osteotomized maxillary segments with Luhr miniplates in secondary cleft surgery. J Maxillofac Surg. 1981; 9:166–169.
74. Drommer, R. The history of the “Le Fort I osteotomy,”. J Maxillofac Surg. 1986; 14:119–122.
75. Dufourmentel, L. Le traitement chirurgical du prognathisme. Presse Med. 1921; 29:235.
76. Egyedi, P, Obwegeser, H. Zur operativen zungenwerk-leinerung. Dtsch Zahn Mund Kieferheilkd. 1964; 41:16.
77. Epker, BN. A modified anterior maxillary osteotomy. J Maxillofac Surg. 1977; 5:35.
78. Epker, B. Modifications in the sagittal osteotomy of the mandible. J Oral Surg. 1977; 35:157–159.
79. Ernst, F. Uber die chirurgische beseitigung der prognathie des unterkiefers (progenie). Zentralbl Chir. 1938; 65:179.
80. Gadd, P. Cited in Limber. J Am Dental Assoc. 1928; 15:851.
81. Gillies, HD. Plastic surgery of the face. London: Oxford University Press; 1920.
82. Gillies, HD, Harrison, SH. Operative correction by osteotomy of recessed malar maxillary compound in case of oxycephaly. Br J Plast Surg. 1950; 3:123.
83. Gillies, HD, Kristensen, HK. Ox cartilage in plastic surgery. Br J Plast Surg. 1951; 4:63.
84. Gillies, HD, Rowe, NL. L’ostéotomie du maxillaire supérieur enoisagée essentiellement dans le cas de bec-de-lièvre total. Rev Stomatol. 1954; 55:545–552.
85. Gillies, HD, Millard, DR, Jr. The principles and art of plastic surgery. Boston: Little, Brown; 1957.
86. Gilmer, TL. Fractures of the inferior maxilla. Ohio St J Dent Sci. 1882; 2:14.
87. Gunning, TB. The treatment of lower jaw by interdental splints. NY Med J. 1866; 3:433.
88. Halvorson, EG, Mulliken, JB. Cheever’s double operation: the first Le Fort I osteotomy. Plast Reconst Surg. 2008; 121:1375–1381.
89. Harsha, WM. Bilateral resection of the jaw for prognathism. Surg Gynecol Obstet. 1912; 15:51.
90. Hausamen, JE. The scientific development of maxillofacial surgery in the 20th century and an outlook into the future. J Craniomaxillofac Surg. 2001; 29:2.
91. Herbert, JM, Kent, JN, Hinds, EC. Correction of prognathism by an intraoral vertical subcondylar osteotomy. J Oral Surg. 1970; 28:651.
92. Hinds, EC. Correction of prognathism by subcondylar osteotomy. J Oral Surg. 1958; 16:209.
93. Hinds, EC, Girotti, WJ. Vertical subcondylar osteotomy: a reappraisal. Oral Surg. 1967; 24:164.
94. Hofer, O. Die operative behandlung der alveolare retraktion des unterkiefers und ihre anwendungsmoglichkeit fur prognathie und mikrogenie. Dtsch Zahn Mund Kieferheilkd. 1942; 9:121–132.
95. Hofer, O. Die osteoplastiche verlagerung des unterkiefers nach von eiselberg bei mikrogenie. Dtsch Zahn Mund Kieferheilkd. 1957; 27:81.
96. Hogemann, KE. Surgical orthopaedic correction of mandibular protrusion. Acta Chir Scand Suppl. 1951; 159:26–28.
97. Hörster, W. Experience with functionally stable plate osteosynthesis after forward displacement of the upper jaw. J Maxillofac Surg. 1980; 8:176–181.
98. Hullihen, S. Case of elongation of the under jaw and distortion of the face and neck, caused by a burn, successfully treated. Am J Dent Sci. 1849; 9:157.
99. Hunsuck, EE. A modified intraoral sagittal splitting technique for correction of mandibular prognathism. J Oral Surg. 1968; 26:250–253.
100. Jaboulay, M, Berard, L. Traitemente chirurgical du prognathisme inferieur. Presse Med. 1898.
101. Jones, BM. Paul Louis Tessier. J Plast Reconstr Surg. 2008; 122:1297–1299.
102. Joseph, J. Verbesserung meiner hangewangenplastik (melomioplastik). Dtsch Med Wochenschr. 1928; 54:567.
103. Kazanjian, VH. Surgical correction of deformities of the jaws and its relation to orthodontia. Am J Orthod Oral Surg. 1936; 22:259.
104. Kazanjian, VH. Jaw reconstruction. Am J Surg. 1939; 3:249.
105. Kazanjian, VH. The interrelation of dentistry and surgery in the treatment of deformities of the face and jaws. Am J Orthod Oral Surg. 1941; 27:11.
106. Kazanjian, VH, Converse, EJ. The surgical treatment of facial injuries. Baltimore: The Williams and Wilkins Company; 1949.
107. Kazanjian, VH. The treatment of mandibular prognathism with special reference to edentulous patients. J Oral Surg Oral Med Oral Pathol. 1951; 4:680–688.
108. Kazanjian, VH. Remembrance of things past. Plast Reconst Surg. 1965; 35(1):5–13.
109. Kingsley, NW. A treatise on oral deformities (as a branch of mechanical surgery). New York: Appleton & Co; 1880.
110. Kirchner, L. Die bedeutung der gesichtsproportionen für die wiederherstellungschirurgie. Fortschr Kiefer Gesichtschir. 1961; 7:5–14.
111. Köle, H. Corticalisschwachung zur unterstutzung bei der kieferorthopadischen behandlung. Fortschr Kiefer Gesichtschir. 1958; 4:208.
112. Köle, H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol. 1959; 12:515–529.
113. Köle, H. Results, experience and problems in the operative treatment of anomalies with reserve overbite. Oral Surg. 1965; 18:427.
114. Köle, H. Zur behandlung der luxationsfracturen des unterkiefers. Zahnärztl Rundsch. 1995; 64:419–425.
115. Kostecka, F. Die chirurgische therapie der progenie. Zahnärztl Rundsch. 1931; 16:670–688.
116. Kufner, J. Four-year experience with major maxillary osteotomy for retrusion. J Oral Surg. 1971; 29:549–553.
117. Lane, WA. Cleft palate and hare lip. London: London Medical Publishing Co Ltd; 1905.
118. Langenbeck, BV. Beitrage zur osteoplastik—die osteoplastische resektion de oberkiefers. In: Goschen A, ed. Deutsche klinik. Berlin: Reimer, 1859.
119. Le Fort, R. Etude experimentale sur les fractures de la machoire superieure. Rev Chir Paris. 1901; 23:214.
120. Le Fort, R. Experimental study of fracture of the upper jaw [reprint]. Plast Reconstr Surg. 1972; 50:497.
121. Levignac, J. Traitment d’un enforcement consolide du tiers moyen de la face par osteotomies et greffes. Rev Stomatol. 1958; 50:551–556.
122. Limberg, AA. Treatment of open bite by means of plastic oblique osteotomy of the ascending rami of the mandible. Dent Cosmos. 1925; 67:1191.
123. Limberg, AA. New method of plastic lengthening of the mandible in unilateral micrognathism and asymmetry of the face. J Am Dent Assoc. 1928; 15:851.
124. Lindorf, HH. Functionally stable tandem screw fixation in sagittal ramus osteotomy: surgical technique. Dtsch Z Mund Kiefer Gesichtschir. 1984; 8:367–373.
125. Lindorf, HH. Sagittal ramus osteotomy with tandem screw fixation: technique and results. J Maxillofac Surg. 1986; 14:311.
126. Loh, FC. Surgical refinement of the anterior maxillary subapical osteotomy. J Oral Maxillofac Surg. 1993; 51:332–334.
127. Luhr, HG. Zur stabilen osteosynthese bei unterkiefer-frakturen. Dtsch Zahnarztl Z. 1968; 23:754.
128. Luhr, HG. Die operative behandlung von unterkieferfrakturen besonderer berucksichtigung der kompressionosteosynthese. Zentralbl Chir. 1969; 94:819.
129. Luhr, HG. The compression osteosynthesis of mandibular fracture in dogs. A histologic contribution to “primary bone healing. ”. Eur Surg Res. 1969; 1:3.
130. Luhr, HG. Die kompressionsosteosynthese bei unterkieferfrakturen. Munich: Hanser; 1972.
131. Luhr, HG, Busch, W, Maerker, R. Histologische untersuchungen zur frage de primaren knochenheilung nach kompressionosteosynthese. Fortschr Kiefer Gesichtschir. 1975; 19:13.
132. Luhr, HG. Skelettverlagernde operationen zur harmonisierung des gesichtsprofils—probleme der stabilen fixation von osteotomiesegmenten. In: von Pfeifer G, ed. Die esthetik von form und funktion in der plastischen und wiederherstellungs—chirurgie. Berlin: Springer-Verlag, 1985.
133. Luhr, HG. A micro-system for craniomaxillofacial surgery. J Cranio Maxillofac Surg. 1988; 16:312.
134. Luhr, HG. Fortschritte der kiefer und gesichts-chirurgie. Stuttgart: Thieme Verlag, 1994; 1–13.
135. Matasa, CG, Graber, TM. Angle, the innovator, mechanical genius, and clinician. Am J Orthod Dentofacial Orthop. 2000; 117:444–452.
136. Max, D, Rotskoff, K. A modified technique for the sagittal split osteotomy. J Oral Maxillofac Surg. 1993; 51:1050.
137. McKinstry, RE. Cleft palate dental care: a historical perspective. Arlington, Va: ABI Publications; 2000.
138. Mehnert, H. Progenieoperation durch sagittalstufenformige osteotomie in horizontalen ast bei bezahntem unterkiefer. Dtsch Zahn Mund Kieferheilkd. 1967; 4:88.
139. Michelet, FX, Deymes, J, Dessus, B. Osteosynthesis with miniaturized screws and plates in maxillofacial surgery. J Maxillofac Surg. 1973; 1:79.
140. Millard, DR. Chin implants. Plast Reconstr Surg. 1954; 13:70.
141. Mohnac, AM. Maxillary osteotomy in the management of occlusal deformities. J Oral Surg. 1966; 24:305.
142. Moos, KF. Origins of orthognathic surgery. Dent Hist. 2000; 37:5–18.
143. Moose, SM. Correction of abnormal mandibular protrusion by intraoral operation. J Oral Surg. 1945; 3:304–310.
144. Muchnic, HV. Spencer Roane Atkinson (1886-1970). Am J Orthod. 1980; 77:580–582.
145. Nance, HN. The limitations of orthodontic treatment. Am J Orthod. 1947; 33:177–223.
146. Niederdellmann, H, Schilli, W. Zur platen osteosynthese bei unterkieferfrakturen. Dtsch Zahnarztl Z. 1973; 28:638.
147. Niederdellmann, H, Schilli, W, Ewers, R, et al. Photoelastic behavior of osteosynthesis plates with different arrangements of screw holes for mandibular fractures. Int J Oral Surg. 1975; 4:27.
148. Niederdellmann, H, Shetty, V. Solitary lag screw osteosynthesis in the treatment of fractures of the angle of the mandible: a retrospective study. Plast Reconstr Surg. 1987; 80:68.
149. Obwegeser, HL, Trauner, R, Obwegeser, H, eds. Dtsch Zahn- Mund- u Kieferheilk; 23. 1955:1–26.
150. Obwegeser, HL. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. Part 1. Oral Surg. 1957; 10:677.
151. Obwegeser, HL. The indications for surgical correction of mandibular deformity by the sagittal splitting technique. Br J Oral Surg. 1964; 1:157–171.
152. Obwegeser, HL. Der offene biss in chirurgischer sicht. Schweiz Monatschr Zahnhlkd. 1964; 74:668–687.
153. Obwegeser, HL. Surgical correction of small or retrodisplaced maxillae. Plast Reconstr Surg. 1969; 53:351.
154. Obwegeser, HL. Zur korrektur der dysostosis otomandibularis. Schweiz Monatsschr Zahnheilkd. 1970; 80:331.
155. Obwegeser, HL. Kieferchirurgische aufgaben im bereich des mittelgesichtes. Arch Otorhinolaryngol. 1974; 207:229.
156. Obwegeser, HL. Orthognathic surgery and a tale of how three procedures came to be: a letter to the next generations of surgeons. Clin Plast Surg. 2007; 34:331–355.
157. Paladin P, ed. Orthodontic history: braced for a century. St. Louis: American Association of Orthodontics, 2005.
158. Perko, M. Maxillary sinus and surgical movement of maxilla. Int J Oral Surg. 1972; 1:177.
159. Perko, M. The history of treatment of cleft lip and palate. Prog Pediatr Surg. 1986; 20:239–248.
160. Perthes, G. Ueber frakturen und luxationsfrakturen des kieferkopfchens und ihre operative behandlung. Verh Dtsch Gesell Chir. Berlin: Springer; 1924.
161. Peterson, HW. Some observations on the progress of orthodontics during the past fifty years. Am J Orthod. 1953; 39:289–290.
162. Proffit, WR, White, RP, Sarver, DM. Contemporary treatment of dentofacial deformity. St. Louis: Mosby; 2003.
163. Proffit WR, Fields HW, Sarver DM, eds. Contemporary orthodontics, ed 4, St. Louis: Mosby/Elsevier, 2007.
164. Proffit, WR, White, RP, Jr. Development of surgeon-orthodontist interaction in orthognathic surgery. Semin Orthod. 2011; 17:183–185.
165. Ricketts, RM. Keystone triad: part 2. Am J Orthod. 1964; 50:728–750.
166. Ring, ME. A thousand years of dental implants: a definitive history, part 1. Compend Contin Educ Dent. 1995; 16:1060–1069.
167. Robinson, M. Prognathism corrected by vertical subcondylotomy. J Oral Surg. 1958; 16:215.
168. Rosen, HM. Surgical correction of the vertically deficient chin. Plast Reconstr Surg. 1988; 82:247.
169. Rowe, NL, Killey, HC. Fractures of the facial skeleton, ed 2. Edinburgh and London: Livingstone Ltd; 1968.
170. Schmid, E. Zue wiederherstellung des mittelgeisichtes nach entwicklungsstorungen und defekten der knochernen unterbaues. Fortschr Kiefer Gesichtschir. 1956; II:240–243.
171. Schuchardt, K. Ein beitrag zur chirurgischen kieferorthopadie unter berucksichtigung ihrer bedentung fur die behandlung angeborener und erworbener kieferdeformitaten bei soldaten. Dtsch Zahn Mund Kieferhlkd. 1942; 9:73.
172. Schuchardt, K. Die chirurgie als helferin der kieferorthopadie. Fortschr Kieferorthop. 1954; 15:9.
173. Schuchardt, K. Formen des offenen bisses und ihre operativen behandlungsmoglechkeiten. In: Schuchardt K, ed. Fortschritt in kiefer und gesichtschirurgie. Stuttgart, Germany: Thieme, 1955.
174. Shankland, WM. The American Association of Orthodontists: the biography of a specialty organization. St. Louis: The American Association of Orthodontists; 1971.
175. Simon, P. Fundamental principles of systematic diagnosis of dental anomalies. Boston: Stratford Co; 1926.
176. Spanier, F. Prognathie-operationen. Z Zahnarztl Orthop Munchen. 1932; 24:76.
177. Spiessl, B. Osteosynthese bei sagittaler osteotomie nach Obwegeser/Dal Pont. Fortschr Kiefer Gesichts Chir. 1974; 18:145.
178. Spiessl, B. The sagittal splitting osteotomy for correction of mandibular prognathism. Clin Plast Surg. 1982; 9:496.
179. Steinhauser, EW. Bone screws and plates in orthognathic surgery. Int J Oral Surg. 1982; 11:209.
180. Stoker, NG, Epker, BN. The posterior maxillary osteotomy: a retrospective study of treatment results. Int J Oral Surg. 1974; 3:153.
181. Strang, RH. Highlights of sixty-four years in orthodontics. Angle Orthod. 1974; 44:101–112.
182. Storum, KA, Bell, WH, Nagura, H. Microangiographic and histologic evaluation of revascularization and healing after genioplasty by osteotomy of the inferior border of the mandible. J Oral Maxillofac Surg. 1988; 48:210–216.
183. Stubtelny, JD, Sakuda, M. Open bite: diagnosis and treatment. Am J Orthod Dentofacial Orthop. 1964; 50:337.
184. Tessier, P, Guiot, G, Rougerie, J, et al. [Cranio-naso-orbito-facial osteotomies. Hypertelorism]. Ann Chir Plast. 1967; 12:103–118.
185. Tessier, P. Demonstration operations at Hopital Foch. Paris (Suresnes). 1967.
186. Tessier, P. Osteotomies totales de la face: syndrome de Crouzon, syndrome d’Apert: oxycephalies, scaphocephalies, turricephalies. Ann Chir Plast. 1967; 12:273–286.
187. Tessier, P. Dysostosis cranio-faciales (syndromes de Crouzon et d’Apert) osteotomies totales de la face. Transactions of the Fourth International Congress of Plastic and Reconstructive Surgery. Rome, 1967/Amsterdam: Excerpta Medica Foundation; 1969.
188. Tessier, P. Autogenous bone grafts taken from the calvarium for facial and cranial applications. Plast Reconstr Surg. 1971; 48:224.
189. Tessier, P. The definitive plastic surgical treatment of the severe facial deformities of craniofacial synostosis: Crouzon and Apert diseases. Plast Reconstr Surg. 1971; 48:419.
190. Tessier, P. Total osteotomy of the middle third of the face for faciostenosis or for sequelae of the Le Fort III fractures. Plast Reconstr Surg. 1971; 48:533.
191. Tessier, P. Traitement des dysmorphies faciales propres aux dysostoses craniofaciales (DGF), maladies de Crouzon et d’Apert. Neurochirurgie. 1971; 17:295.
192. Tessier P: Recent improvement in the treatment of facial and cranial deformities in Crouzon disease and Apert syndrome. In Symposium of plastic surgery of the orbital region, St. Louis, 1976, CV Mosby Co, pp 271.
193. Tessier, P. Relationship of craniosynostosis to craniofacial dysostosis and to faciosynostosis: a study with therapeutic implications. Clin Plast Surg. 1982; 9:531.
194. Tessier, P. Apert syndrome: acrocephalosyndactyly, type I. In: Caronni P, ed. Craniofacial surgery. Boston: Little, Brown, 1985.
195. Tessier, P. Craniofacial surgery in syndromic craniosynostosis: craniosynostosis, diagnosis, evaluation and management. New York: Raven Press; 1986.
196. Tessier, P. The monobloc and frontofacial advancement: do the pluses outweigh the minuses? [discussion]. Plast Reconstr Surg. 1993; 91:988.
197. The Division of Plastic and Reconstructive Surgery, Department of Surgery, Washington University School of Medicine: The legacy of Vilray Blair. http://surgerydept. wustl. edu/Surgery_M. aspx?id=2990&menu_id=284.
198. Trauner, R, Obwegeser, H. Zur operationstechnik bei der progenie und anderen unterkieferanomalien. Deutsche Zahn-, Mund- und Kieferheilkunde. 1955; 23:1–26.
199. Trauner, R, Obwegeser, H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg Oral Med Oral Pathol. 1957; 10:677–689.
200. Trauner, R, Obwegeser, H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. II. Operating methods for microgenia and distoocclusion. Oral Surg Oral Med Oral Pathol. 1957; 10:787–792.
201. Von Eiselberg, E. Cited in Limberg. J Am Dental Assoc. 1928; 15:851.
202. Wahl, N. Orthodontics in 3 millennia. Chapter 1: Antiquity to the mid-19th century. Am J Orthod Dentofacial Orthop. 2005; 127:255–259.
203. Wahl, N. Orthodontics in 3 millennia. Chapter 2: Entering the modern era. Am J Orthod Dentofacial Orthop. 2005; 127:510–515.
204. Wahl, N. Orthodontics in 3 millennia. Chapter 6: More early 20th-century appliances and the extraction controversy. Am J Orthod Dentofacial Orthop. 2005; 128:795–800.
205. Wassmund, M, Frakturen und luxationen des gesichtsschadels. 1927.
206. Wassmund, M. Die totale mobilisation des oberkiefers. Lehrbuch der praktischen chirurgie des mundes und der kiefer. Leipzig: Meusser; 1935.
207. Wassmund, M. Die korrektur der mikrognathie. Lehrbuch der praktischen chirurgie des mundes und der kiefer. Leipzig: Barth; 1939.
208. Weinberger, BW. Orthodontics: a historical review of its origin and evolution, including an extensive bibliography of orthodontic literature up to the time of specialization. St. Louis: The CV Mosby Company; 1926.
209. Weinberger, BW. Historical resume of the evolution and growth of orthodontia. J Am Dent Assoc. 1934; 21:2001–2021.
210. Weinberger, BW. Dr Edward Hartley Angle: his influence on orthodontics. Am J Orthod. 1950; 36:596–607.
211. Weinstein, I. C-osteotomy for correction of mandibular retrognathia: report of cases. J Oral Surg. 1971; 29:358.
212. Whipple, JW. Double resection of the inferior maxilla for protruding lower jaw. Dent Cosmos. 1898; 40:552–557.
213. Wikkeling, OME, Tacoma, J. Osteotomy of the pterygomaxillary junction. Int J Oral Surg. 1975; 4:99.
214. Wolfe, SA. Gunther Cohn-Stock, M. S., D. D. S., father of maxillary orthognathic surgery. J Cranio Maxillofac Surg. 1989; 17:331–334.
215. Wolfe, SA. Paul Tessier, creator of a new surgical specialty, is recipient of Jacobson innovations award. J Craniofacial Surg. 2001; 12(1):98–99.
216. Wolfe, SA. Paul Louis Tessier, MD, 1917 to 2008. J Plast Reconstr Surg. 2008; 122:1294–1296.
217. Worms, FW, Meskin, CH, Isaacson, RJ. Open bite. Am J Orthod Dentofacial Orthop. 1971; 59:589.
218. Wright, CF. Status of orthodontic education prior to 1930. Angle Orthod. 1947; 17:92–96.
219. Wunderer, S. Die prognathie-operation mittels frontal gestieltem maxillofragment. Oesterr Z Stomatol. 1962; 59:98–102.
220. Wunderer, S. Erfahrungen mit der operativen behandlung hochgradiger prognathien. Dtsch Zahn Mund Kieferheilkd. 1963; 39:451.
*Please note that the author of this text has paraphrased Dr. Proffit’s original work.
*Please note that this section was reviewed for accuracy by Dr. Obwegeser.
*Please note that this section was reviewed for accuracy by Dr. Bell.
*Please note that this section was reviewed for accuracy by Dr. Luhr.