Pigmentation
Skin colour is due to a mixture of the pigments melanin (p. 8), oxyhaemoglobin (in blood) and carotene (in the stratum corneum and subcutaneous fat). Pigmentary diseases are common and particularly distressing to those with darker skin. Disorders of pigmentation mainly involve melanocytes, but other causes are mentioned where relevant.
Hypopigmentation
Pigment loss may be generalized or patchy. Generalized hypopigmentation occurs with albinism, phenylketonuria and hypopituitarism; patchy loss is seen in vitiligo, after inflammation, following exposure to some chemicals and with certain infections (Table 1).
| Cause | Example |
|---|---|
| Chemical | Substituted phenols, hydroquinone |
| Endocrine | Hypopituitarism |
| Genetic | Albinism, phenylketonuria, tuberous sclerosis, piebaldism |
| Infection | Leprosy, yaws, pityriasis versicolor |
| Postinflammatory | Cryotherapy, eczema, psoriasis, morphoea, pityriasis alba |
| Other | Vitiligo, lichen sclerosus, halo naevus, scarring |
Vitiligo
Clinical presentation
Vitiligo affects 0.5% of the population, is seen in all races and is most troublesome in those with a dark skin. The sex incidence is equal, and the onset, usually between 10 and 30 years of age, may be precipitated by injury or sunburn. The sharply defined white macules are often symmetrical (Fig. 1). The hands, wrists, knees, neck and areas around orifices (e.g. the mouth) are frequently affected. Occasionally, vitiligo is segmental (e.g. down an arm), generalized or universal. The course is unpredictable; areas may remain static, spread or (infrequently) repigment. In light-skinned individuals, vitiligo may be discernible only in summer, when the non-vitiliginous areas become sun-tanned.
Differential diagnosis
Postinflammatory hypopigmentation is often accompanied by other skin changes (Table 1). In chemical leucoderma, a history of exposure to phenolic chemicals should be sought. The hypopigmented macules of leprosy are normally anaesthetic.
Albinism
There are several syndromes of albinism. All are autosomal recessive and show a lack of pigment in the skin, hair, iris and retina. Melanocyte numbers are normal, but melanosome production fails due to defective gene control of tyrosinase (p. 8).
Albinism is uncommon (the prevalence is 1/20 000), although the diagnosis is straightforward. The skin is white or pink, the hair white and pigmentation is lacking in the eye (Fig. 2). Albinos have poor sight, photophobia and nystagmus. ‘Tyrosinase-positive’ albinos may pigment slightly with age, so that black African skin becomes yellow and freckled. In the tropics, albinos risk premature skin photoageing and the early onset of skin tumours, especially squamous cell carcinomas.
Hyperpigmentation
Hyperpigmentation is mostly hypermelanosis (Table 2), but sometimes other pigments colour the skin, e.g. iron deposition (with melanin) in haemochromatosis, and carotene (causing an orange discoloration) in carotenaemia, usually due to eating too many carrots.
| Cause | Example |
|---|---|
| Drugs | Photosensitizers, psoralens, oestrogens, phenothiazines, minocycline, amiodarone |
| Endocrine | Addison’s disease, Cushing syndrome, Graves’ disease |
| Genetic | Racial, freckles, neurofibromatosis, Peutz–Jeghers syndrome |
| Metabolic | Biliary cirrhosis, haemochromatosis, porphyria |
| Nutritional | Carotenaemia, malabsorption, malnutrition, pellagra |
| Postinflammatory | Eczema, lichen planus, systemic sclerosis, lichen amyloidosis |
| Other | Acanthosis nigricans, naevi, malignant melanoma, argyria, chronic renal failure |
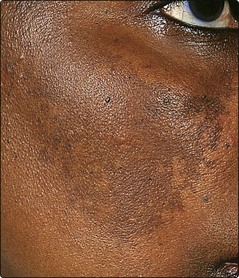
Melasma (chloasma)
Melasma is a patterned macular facial pigmentation occurring with pregnancy and in women on oral contraceptives. The pigmentation is symmetrical and often involves the forehead (Fig. 3). Pregnancy stimulates melanocytes generally, and also increases pigmentation of the nipples and lower abdomen and in existing melanocytic naevi. Melasma may improve spontaneously. Topical tretinoin, azelaic acid or hydroquinone can reduce pigmentation. Sunscreens and camouflage cosmetics can help.
Peutz–Jeghers syndrome
Peutz–Jeghers syndrome is a rare autosomal dominant condition. Lentigines around the lips (Fig. 4), buccal mucosa and fingers are associated with small bowel polyps. The polyps may cause intussusception and rarely undergo malignant change.
Addison’s disease
Addison’s disease is characterized by hypoadrenalism with pituitary overproduction of adrenocorticotrophic hormone (ACTH). The skin signs are due to excess ACTH, which stimulates melanogenesis. Pigmentation may be generalized or limited to the buccal mucosa (Fig. 5), palmar creases, scars, flexures or areas subjected to friction. Addisonian-like pigmentation is also seen in Cushing syndrome, hyperthyroidism and acromegaly.
Drug-induced pigmentation
Drug-induced pigmentation may be due to stimulation of melanogenesis or deposition of the drug in the skin, but the mechanism is often not well understood (Table 3, p. 86). Of the commonly used drugs, amiodarone, phenothiazines and minocycline not infrequently induce pigmentation.
| Drug | Effect |
|---|---|
| Amiodarone | Blue-grey pigmentation of exposed areas (p. 87) |
| Bleomycin | Diffuse pigmentation, often flexural; flagellate pattern |
| Busulfan | Diffuse brown pigment |
| Chloroquine | Blue-grey pigmentation of face and arms |
| Chlorpromazine | Slatey-grey pigment in sun-exposed sites |
| Clofazimine | Red and black pigment |
| Mepacrine | Yellow (drug deposited) |
| Minocycline | Blue-black pigment in scars and sun-exposed sites |
| Psoralens | Topical or systemic photosensitizers (cosmetics) |
Disorders of pigmentation
 Vitiligo: common, autoimmune; well-defined depigmented macules.
Vitiligo: common, autoimmune; well-defined depigmented macules.
 Albinism: rare, autosomal recessive; lack of skin and eye pigment; need strict sun avoidance; risk of skin cancer.
Albinism: rare, autosomal recessive; lack of skin and eye pigment; need strict sun avoidance; risk of skin cancer.
 Phenylketonuria: autosomal recessive enzyme defect; fair skin and hair.
Phenylketonuria: autosomal recessive enzyme defect; fair skin and hair.
 Freckles: brown macules darken with sun; normal number of melanocytes.
Freckles: brown macules darken with sun; normal number of melanocytes.
 Lentigines: brown macules; melanocyte numbers are increased.
Lentigines: brown macules; melanocyte numbers are increased.
 Peutz–Jeghers syndrome: autosomal dominant disorder of perioral lentigines and intestinal polyps.
Peutz–Jeghers syndrome: autosomal dominant disorder of perioral lentigines and intestinal polyps.
 Melasma: facial pigmentation; related to pregnancy and ‘the pill’.
Melasma: facial pigmentation; related to pregnancy and ‘the pill’.
 Addison’s disease: ACTH-stimulated melanogenesis of mucosae and flexures.
Addison’s disease: ACTH-stimulated melanogenesis of mucosae and flexures.
 Drug-induced pigmentation: due to deposition of pigment or stimulation of melanogenesis.
Drug-induced pigmentation: due to deposition of pigment or stimulation of melanogenesis.