Chapter 3 Physiology of the Reproductive Tract
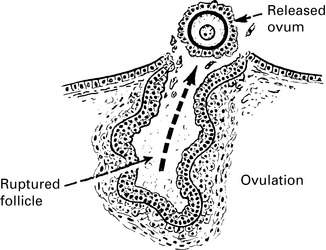
Ovulation
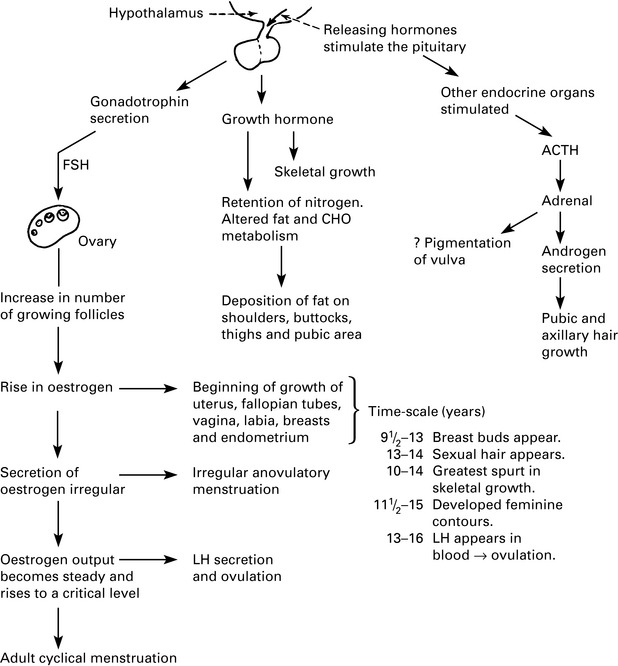
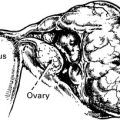
Female reproductive physiology
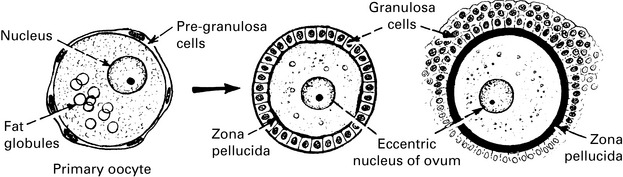
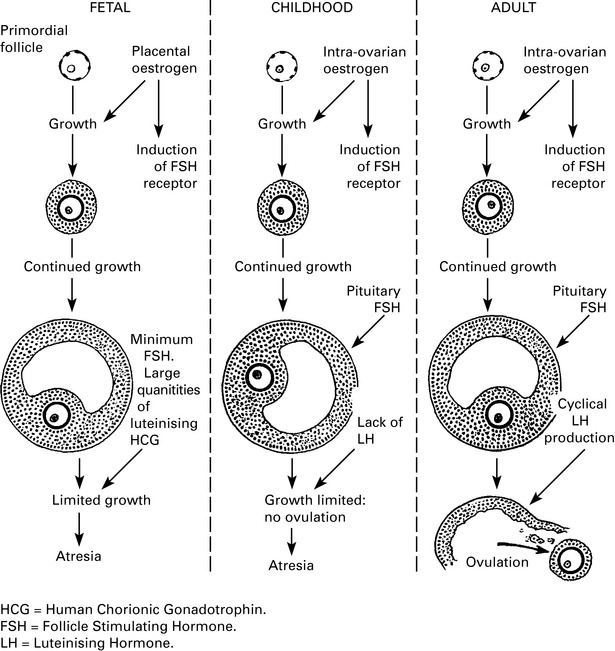
In men, gamete production continues throughout life, whereas women develop their life supply of gametes during intrauterine life. See Chapter 1. The numbers decline even before birth, and there will be around 300,000 remaining at puberty.
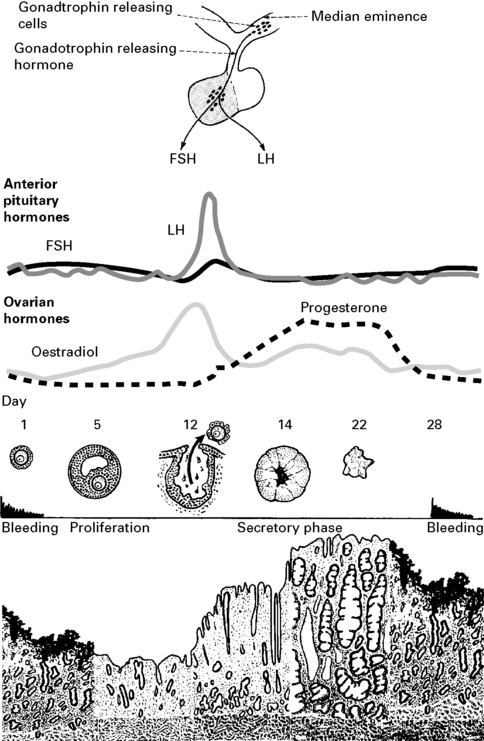
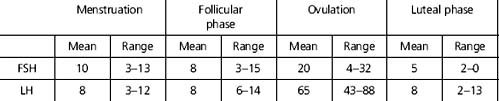
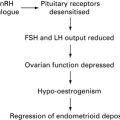
Cyclical ovarian hormonal changes
Action of ovarian hormones
Target tissues
 |
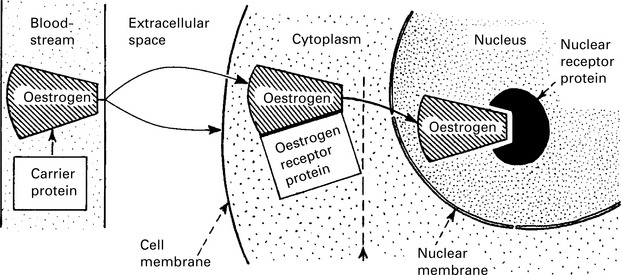
Tissues of these structures are particularly sensitive to oestrogen stimulation. The cytoplasm of their cells contains a specific oestrogen receptor molecule that has an affinity for oestrogen 100,000 times greater than the carrier protein, which retains the hormone in the bloodstream. Oestrogen also acts at the cell membrane, regulating ligand-gated ion channels. |
| Progesterone receptors appear in the cytoplasm only after the cell has been primed by oestrogen. |