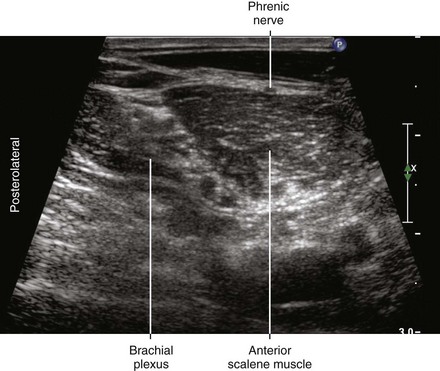
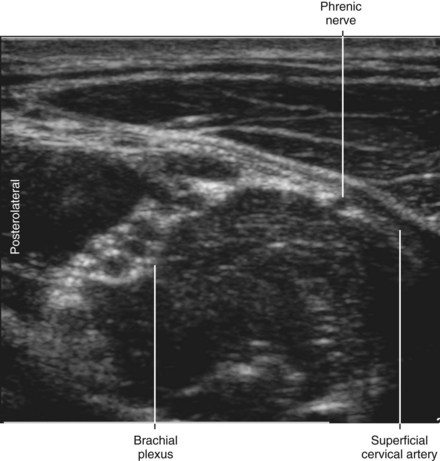
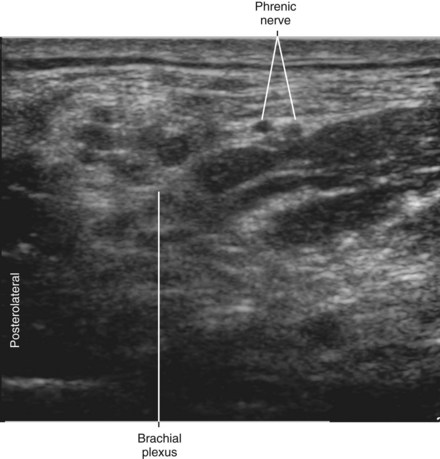
28 Phrenic Nerve Imaging
The phrenic nerve is a small (<1 mm in diameter), monofascicular nerve that arises from the third, fourth, and fifth cervical ventral rami. The most consistent and largest contribution is from the fourth cervical ventral ramus. At the level of the cricoid cartilage, the phrenic nerve is essentially coincident with the C5 ventral ramus.1 As the nerve descends the neck, it travels from lateral to medial over the surface of the anterior scalene muscle. The nerve usually enters the chest between the subclavian artery and vein. Accessory phrenic nerves are observed in 60% of specimens and often derive from the fifth cervical ventral ramus.2
Phrenic nerve imaging is important for two reasons. First, it may be possible to reduce the incidence of transient pulmonary complications related to phrenic nerve block using ultrasound. Low volumes of local anesthetic (5 mL) administered for interscalene block using ultrasound guidance appear to reduce the incidence of concomitant phrenic nerve block.3 Ultrasound guidance allows more caudal approaches to brachial plexus block with an even lower chance of phrenic nerve block. Second, direct trauma to the nerve can potentially be avoided during regional anesthetic procedures in the cervical region.
1 Kessler J, Schafhalter-Zoppoth I, Gray AT. An ultrasound study of the phrenic nerve in the posterior cervical triangle: implications for the interscalene brachial plexus block. Reg Anesth Pain Med. 2008;33:545–550.
2 Loukas M, Kinsella CR, Jr., Louis RG, Jr., et al. Surgical anatomy of the accessory phrenic nerve. Ann Thorac Surg. 2006;82:1870–1875.
3 Riazi S, Carmichael N, Awad I, et al. Effect of local anaesthetic volume (20 vs 5 mL) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth. 2008;101:549–556.