Chapter 648 Photosensitivity
Acute Sunburn Reaction
Pathophysiology and Clinical Manifestations
Transmitted radiation <300 nm is largely absorbed in the epidermis, whereas that >300 nm is mostly transmitted to the dermis after variable epidermal melanin absorption. Children vary in susceptibility to UV radiation, depending on their skin type (amount of pigment) (Table 648-1). Immediate pigment darkening is due to UVA radiation–induced photo-oxidative darkening of existing melanin and its transfer from melanocytes to keratinocytes. This effect generally lasts for a few hours and is not photoprotective. UVB-induced effects appear 6-12 hr after initial exposure and reach a peak in 24 hr. Effects include redness, tenderness, edema, and blistering (Fig. 648-1). Reactive oxidation species generated by UVB induce keratinocyte membrane damage and are involved in the pathogenesis of sunburn. A portion of the vasodilatation seen in UVB-induced erythema is mediated by prostaglandins E2 and F2. Delayed melanogenesis as a result of UVB radiation begins in 2-3 days and lasts several days to a few weeks. Manufacture of new melanin in melanocytes, transfer of melanin from melanocytes to keratinocytes, increase in size and arborization of melanocytes, and activation of quiescent melanocytes produce delayed melanogenesis. This effect reduces skin sensitivity to development of UV-induced erythema. The amount of protection afforded depends on the skin type of the patient. Additional effects and possible complications of sun exposure include increased thickness of the stratum corneum, recurrence or exacerbation of herpes simplex labialis, lupus erythematosus, and many other conditions (Table 648-2).
| TYPE AND DEMOGRAPHICS | SUNBURN, TANNING HISTORY |
|---|---|
| I Red hair, freckles, Celtic origin | Always burns easily, no tanning |
| II Fair skin, fair-haired, blue-eyed, white | Usually burns, minimal tanning |
| III Darker-skinned white | Sometimes burns, gradual light brown tan |
| IV Mediterranean background | Minimal to no burning, always tans |
| V Middle Eastern white, Mexican | Rarely burns, tans profusely dark brown |
| VI Black | Never burns, pigmented black |
Table 648-2 CUTANEOUS REACTIONS TO SUNLIGHT
Prognosis and Prevention of Sequelae
The long-term sequelae of chronic and intense sun exposure are not often seen in children, but most individuals receive >50% of their lifetime UV dose by age 20 yr. Therefore, pediatricians have a pivotal role in educating patients and their parents about the harmful effects, potential malignancy risks, and irreversible skin damage that result from unduly prolonged exposure to the sun and tanning lights. Premature aging, senile elastosis, actinic keratoses, squamous and basal cell carcinomas, and melanomas all occur with greater frequency in sun-damaged skin. In particular, blistering sunburns in childhood and adolescence significantly increase the risk for development of malignant melanoma. Sun protection is best achieved by sun avoidance, which includes minimizing time in the midday sun (10 AM to 3 PM), staying in the shade, and wearing protective clothing including wide-brimmed hats. Protection is enhanced by a wide variety of sunscreen agents. Physical opaque sunscreens (zinc oxide, titanium dioxide) block UV light, whereas chemical sunscreens (para-aminobenzoic acid [PABA], PABA esters, salicylates, benzophenones, dibenzoylmethanes [avobenzone], cinnamates, terephthalylidene dicamphor sulfonic acid [ecamsule]) absorb damaging radiation. The benzophenones and dibenzoylmethanes provide protection in both the UVA and UVB ranges. Stabilizers such as octocrylene and diethyl 2,6-naphthalate increase the time of function of the dibenzoylmethanes. Ecamsule and drometrizole trisiloxane are UVA sunscreens. Vitamins C and E added to sunscreen may also be beneficial in reduction of the formation of reactive oxygen species. Children with skin types I to III (see Table 648-1) require sunscreens with a sun protection factor (SPF) of at least 15, although the higher SPF, the more protection. SPF is defined as the minimal dose of sunlight required to produce cutaneous erythema after application of a sunscreen, divided by the dose required with no use of sunscreen. SPF applies only to UVB protection. UVA rating of sunscreens should be available in the near future.
Photosensitive Reactions
Photoallergic reactions occur in only a small percentage of persons exposed to photosensitizers and light and require a time interval for sensitization to take place. Thereafter, dermatitis appears within ≈ 24 hr of re-exposure to the photosensitizer and light. Photoallergic dermatitis is a T cell–mediated delayed hypersensitivity reaction in which the drug, acting as a hapten, may combine with a skin protein to form the antigenic substance. Photoallergic reactions vary in morphology and may occur on partially covered and on light-exposed skin. Some of the important classes of drugs and chemicals responsible for photosensitivity reactions are listed in Table 648-2.
Phototoxic reactions occur in all individuals who accumulate adequate amounts of a photosensitizing drug or chemical within the skin. Prior sensitization is not required. Dermatitis develops within hours after exposure to radiation in the range of 285-450 nm. The eruption is confined to light-exposed areas and often resembles exaggerated sunburn, but it may be urticarial or bullous. It results in postinflammatory hyperpigmentation. All the drugs that cause photoallergic reactions may also cause a phototoxic dermatitis if given in sufficiently high doses. Several additional drugs and contactants cause phototoxic reactions, notably the plant-derived furocoumarins (see Table 648-2). Differentiation from contact dermatitis due to poison ivy or poison oak may be difficult, but itching is prominent in contact dermatitis. In phytophotodermatitis, burning is prominent and is confined to sun-exposed areas, sparing the upper eyelids, beneath the nose and chin, and the retroauricular areas. Postinflammatory hyperpigmentation develops rapidly and is usually the presenting sign.
Porphyrias (Chapter 85)
Congenital erythropoietic porphyria (Günther disease) is a rare autosomal recessive disorder. It manifests in the first few months of life as exquisite sensitivity to light, which may induce repeated severe bullous eruptions that result in mutilating scars (Fig. 648-2). Hyperpigmentation, hyperkeratosis, vesiculation, and fragility of skin develop in light-exposed areas. Hirsutism in areas of mild involvement, scarring alopecia in severely affected areas, pink to red urine, brown teeth, hemolytic anemia, splenomegaly, and increased amounts of uroporphyrin I in urine, plasma, and erythrocytes and of coproporphyrin I in feces are additional characteristic manifestations. Urine from affected patients fluoresces reddish pink under a Wood light. Total protection from sunlight is the treatment of choice.
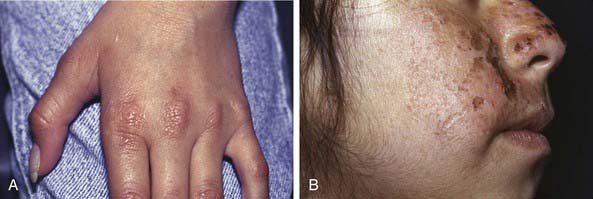
Erythropoietic protoporphyria, an autosomal dominant trait, becomes apparent in early childhood and manifests as pain, tingling, and a burning sensation within ≈ 30 min of sun exposure, followed by erythema, edema, urticaria, and, rarely, vesicles on light-exposed areas. Nail changes consist of opacification of the nail plate, onycholysis, pain, and tenderness. Mild systemic symptoms such as malaise, chills, and fever may accompany the acute skin reaction. Recurrent sun exposure produces a chronic eczematous dermatitis with thickened, lichenified skin, especially over the finger joints (Fig. 648-3A), and persistent violaceous erythema, ulcers, and pitted or linear, crusted atrophic scars on the face (Fig. 648-3B) and rims of the ears. Pigmentation, hypertrichosis, skin fragility, and mutilation are uncommon. Liver disease is uncommon and generally mild, with only 3% of patients demonstrating severe disease.
Actinic Prurigo
A chronic familial photodermatitis, actinic prurigo is inherited as an autosomal dominant trait among the Native Americans of North and South America. HLA DRB1*0407 (60-70%) and HLA DRB1*0401 (20%) are strongly associated with actinic prurigo. The first episode generally occurs in early childhood, several hours to 2 days after intense sun exposure. Most patients are female and are sensitive to UVA radiation. Lesions are intensely pruritic, erythematous papules on the face (Fig. 648-4), lower lip, distal extremities, and, in severe cases, buttocks. Facial lesions may heal with minute pitted or linear scarring. Lesions often become chronic, without periods of total clearing, merging into eczematous plaques that lichenify and may become secondarily infected. Associated features that distinguish this disorder from other photoeruptions and atopic dermatitis include cheilitis, conjunctivitis, and traumatic alopecia of the outer half of the eyebrows. Actinic prurigo is a chronic condition that generally persists into adult life, although it may improve spontaneously in the late teenage years. Sun avoidance, protective clothing, and broad-spectrum sunscreens may be helpful in preventing the eruption. Mid- to high-potency topical corticosteroids and antihistamines palliate the pruritus and inflammation. Thalidomide 50-100 mg/day is very effective, but its use is limited by toxicity.
Solar Urticaria
Solar urticaria is a rare disorder induced by UV or visible irradiation. The disorder is mediated by immunoglobulin (Ig) E antibodies to either an abnormal chromophore (type I) or a normal chromophore (type II), leading to mast cell degranulation and histamine release. This reaction occurs within 5-10 min of sun exposure, fades within 1-2 hr, and is characterized by widespread severe wheal formation (Fig. 648-5), which may lead to faintness, headache, nausea, syncope, or bronchospasm. H1-blocking antihistamines may be useful to prevent or abate the eruption.
Cockayne Syndrome
Onset of Cockayne syndrome, an autosomal recessive disorder, is characterized by the appearance, at ≈ 1 yr of age, of facial erythema in a butterfly distribution after sun exposure, followed by loss of adipose tissue and development of thin, atrophic, hyperpigmented skin, particularly over the face. Associated features include dwarfism; mental retardation; large, protuberant ears; long limbs; disproportionately large hands and feet, which are sometimes cool and cyanotic; pinched nose; carious teeth; unsteady gait with tremor; limitation of joint mobility; progressive deafness; cataracts; retinal degeneration; optic atrophy; decreased sweating and tearing; and premature graying of the hair. Diffuse extensive demyelination of the peripheral and central nervous systems ensues, and patients generally die of atheromatous vascular disease before the third decade. There are 2 types of Cockayne syndrome. Type I (CSA gene) is less severe than type II (CSB gene). Xeroderma pigmentosum–Cockayne syndrome (XP-CS) demonstrates complementation with xeroderma pigmentosa groups B, D, or G. Patients with XP-CS are phenotypically more like patients with Cockayne syndrome. Photosensitivity is due to deficient rates of repair of UV-induced damage, specifically within actively transcribing regions of DNA (transcription-coupled DNA repair). The syndrome is distinguished from progeria (Chapter 84) by the presence in Cockayne syndrome of photosensitivity and the ocular abnormalities.
Xeroderma Pigmentosum
Xeroderma pigmentosum is a rare autosomal recessive disorder that results from a defect in nucleotide excision repair. Seven complementation groups have been recognized, on the basis of each group’s separate defect in ability to repair damaged DNA. Xeroderma pigmentosum variant is caused by mutations in the DNA polymerase ETA gene (POLH), which lead to a defect in the conversion of newly synthesized DNA after UV radiation. The wavelength of light that induces the DNA damage ranges from 280 to 340 nm. Skin changes are first noted during infancy or early childhood in sun-exposed areas such as the face, neck, hands, and arms; lesions may occur, however, at other sites, including the scalp. The skin lesions consist of erythema, scaling, bullae, crusting, ephelides, telangiectasia, keratoses (Fig. 648-6), basal and squamous cell carcinomas, and malignant melanomas. Ocular manifestations include photophobia, lacrimation, blepharitis, symblepharon, keratitis, corneal opacities, tumors of the lids, and possible eventual blindness. Neurologic abnormalities such as mental deterioration and sensorineural deafness may develop in ≈ 20% of patients.
Rothmund-Thomson Syndrome
Rothmund-Thomson syndrome is also known as poikiloderma congenitale because of the striking skin changes (Fig. 648-7). It is inherited as an autosomal recessive trait. Mutations in the RECQL4 gene are found in approximately 65% of the patients. The other mutations causing Rothmund-Thomson syndrome are unknown. Skin changes are noted as early as 3 mo of age. Plaques of erythema and edema appear on the cheeks, forehead, ears, neck, dorsal portions of the hands, extensor surfaces of the arms, and buttocks and are replaced gradually by reticulated, atrophic, hyperpigmented, telangiectatic plaques. Light sensitivity is present in many cases, and exposure to the sun may provoke formation of bullae. Areas of involvement, however, are not strictly photodistributed. Short stature; small hands and feet; sparse eyebrows, eyelashes, and pubic and axillary hair, and sparse, fine, prematurely gray scalp hair or alopecia; bony defects; and hypogenitalism are common. Cataracts may also occur at an early age. Most patients have normal mental development. Keratoses and later squamous cell carcinomas may develop on exposed skin. The most worrisome association is that with osteosarcoma, which occurs only in those patients with Rothmund-Thomson syndrome and RECQL4 mutations.
Balk SJ, Geller AC. Teenagers and artificial tanning. Pediatrics. 2008;121:1040-1042.
Bissonnette R. Update on sunscreens. Skin Therapy Lett. 2008;13:5-7.
Botto NC, Warshaw EM. Solar urticaria. J Am Acad Dermatol. 2008;59:909-920.
Honigsmann H. Polymorphous light eruption. Photodermatol Photoimmunol Photomed. 2008;24:155-161.
Iwatsuki K, Satoh M, Yamamoto T, et al. Pathogenic link between hydroa vacciniforme and Epstein-Barr virus associated hematologic disorders. Arch Dermatol. 2006;142:587-595.
Lautenschlager S, Wulf HC, Pittelkow MR. Photoprotection. Lancet. 2007;370:528-537.
2007 A new sunscreen agent. Med Lett Drugs Ther. 2007;49:41-43.
Pourabbani S, Marra DE, Iwasaki J, et al. Colloid milium: a review and update. J Drugs Dermatol. 2007;6:293-296.
Ross G, Foley P, Baker C. Actinic prurigo. Photodermatol Photoimmunol Photomed. 2008;24:272-275.
Sassa S. Modern diagnosis and management of the porphyries. Br J Haematol. 2006;135:281-292.