27 Photorejuvenation with Lasers
Cumulative damage to the skin over time from ultraviolet light results in photoaging. Photoaging changes are clinically evident as benign pigmented lesions, such as solar lentigines, freckles (ephelides), hyperpigmentation, melasma, and as benign vascular lesions, such as telangiectasias, poikiloderma of Civatte, rosacea, and cherry angiomas.1 Photorejuvenation refers to the cosmetic treatment of photoaged skin with nonablative lasers and light-based technologies (collectively referred to as lasers*).2 Treatments are most commonly performed on the face, neck, chest, and hands, but may be performed on almost any photodamaged area of the body.3 Photorejuvenation treatments reliably achieve improvements, have short postprocedure recovery times and minimal risks of complications, and are associated with high patient satisfaction.4,5
Laser Principles
Laser treatments are based on the principle of selective photothermolysis. Light-absorbing pigments in the skin, called chromophores, selectively absorb light energy and convert it to heat in the targeted lesions. The lesions are heated, damaged, and eliminated, while the surrounding skin is left unaffected. Photorejuvenation treatment of benign pigmented and vascular lesions is achieved through selectively targeting two main chromophores in the skin, oxyhemoglobin, which is found in red blood, and melanin, which is found in pigmented lesions.6
When treating red vascular lesions, laser energy is absorbed by the oxyhemoglobin chromophore. The vessel is heated, causing injury to the vessel wall and perivascular collagen damage, which results in vessel closure and obliteration. Oxyhemoglobin absorbs light between 510 and 600 nm (Figure 27-1). Lasers used for the treatment of red vascular lesions produce light in this range and include argon (510 nm), potassium titanyl phosphate or KTP (532 nm), and pulsed dye (585 nm) lasers.
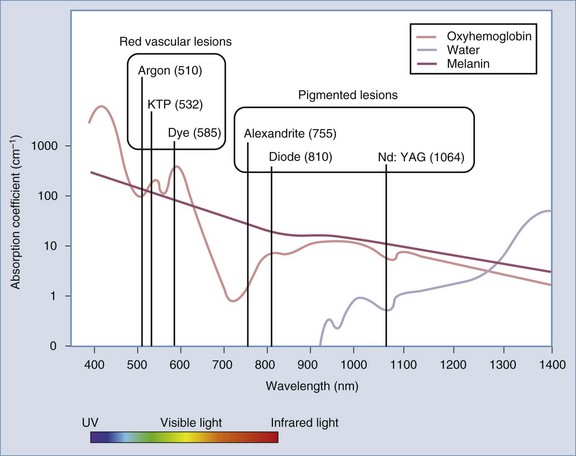
FIGURE 27-1 Absorption spectra of tissue chromophores and lasers commonly used for photorejuvenation.
When treating benign pigmented lesions, such as lentigines, light energy is absorbed by the target chromophore melanin that is contained within the melanosomes of epidermal melanocytes and keratinocytes. The melanosome is heated, ruptured, and the melanin eliminated. Melanin preferentially absorbs light between 650 and 1100 nm (see Figure 27-1). Lasers used for treatment of epidermal pigmented lesions produce light in this range and include ruby (694 nm), alexandrite (755 nm), diode (810 nm), and neodymium-doped yttrium aluminum garnet or Nd:YAG (1064 nm) lasers. The light from KTP (532 nm) and argon (510 nm) lasers has high absorption by both melanin and oxyhemoglobin and can be used to treat both pigmented and vascular lesions.
Several device parameters affect the safety and efficacy of photorejuvenation treatments. These parameters include wavelength, fluence, pulse duration, and spot size (see Laser Parameters in Chapter 19, Aesthetic Principles and Consultation).
Patient Selection
Patients with fair skin (Fitzpatrick skin types I through III) are the best candidates for photorejuvenation treatments because this population presents with the greatest contrast between background skin and target lesions. Both benign vascularities and hyperpigmentation are common complaints in patients with light skin types. Photodamaged skin characteristically shows midface erythema and peripheral lentigines (see Figure 19-1 in Chapter 19).
Indications
Patient Expectations
Photorejuvenation of benign pigmented and vascular lesions may be performed on virtually any body region where photodamage is present. The face, neck, chest, and hands are some of the most commonly treated areas. Noticeable results are evident with a single treatment in properly selected candidates, but typically a series of three to five IPL treatments is required for dramatic improvements.4 Treatment with lasers may require a fewer number of treatments than with IPL devices. Larger red facial vessels, which have more chromophore target, usually respond more dramatically than smaller lacy red vessels or diffuse erythema. Discreet lesions such as cherry angiomas typically resolve with no recurrence after one or two treatments.
Alternative Therapies
Nonlaser treatment options for benign pigmented lesions include liquid nitrogen, exfoliation treatments such as microdermabrasion and chemical peels, and topical skin-lightening products such as hydroquinone. Liquid nitrogen can achieve reduction in pigmentation, however, it is frequently associated with hyperpigmentation and hypopigmentation and it is advisable to restrict use to lighter skin types for this reason. Exfoliation and topical therapies are slower to achieve improvements and results are rarely comparable to those seen with lasers. More aggressive laser treatments with longer recovery times and greater risks of complications, such as ablative carbon dioxide and erbium lasers (fractionated and nonfractionated), are also indicated for pigmented lesions. Electrosurgery may be used for some vascular lesions, although this may scar (see Chapter 14, Electrosurgery). Photodynamic therapy (PDT), utilizing topical photosensitizing medication activated by light, has also been used for photorejuvenation (see the Current Developments section below).
Products Currently Available7–11
Lasers commonly used for treatment of red vascular lesions include the following:
Lasers commonly used for treatment of pigmented lesions include these:
See the Resources section at the end of this chapter for laser manufacturers.
Contraindications
See Chapter 26, Hair Reduction with Lasers, for general laser contraindications. Other contraindications include:
Anatomy
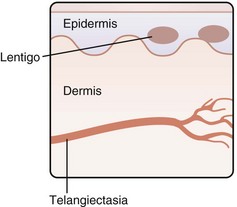
Benign pigmented lesions, such as lentigines, and benign vascular lesions, such as telangiectasias, are some of the most common lesions evident in photodamaged skin. Figure 27-2 shows the relative location of these lesions in the skin, with lentigines in the epidermis and telangiectasias in the dermis.
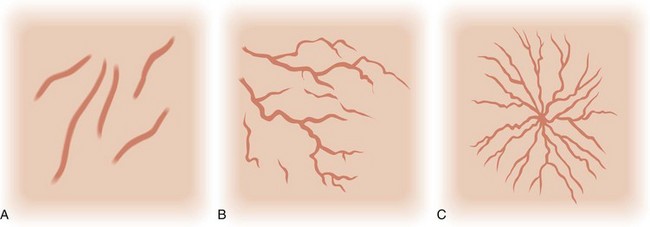
Telangiectasias are these cutaneous vessels that range in size from 0.1 to 1.0 mm. The three main types linear, arborizing and spider, are shown in Figure 27-3. Telangiectasias that arise from dilated arterioles are bright red with small diameters; those from venules are bluish in color with larger diameters; and those from capillaries are fine lacy red vessels or appear as background erythema to the naked eye.12 Red facial telangiectasias seen with photoaging are commonly located in the midface on the nasal ala and dorsum of the nose and cheeks. Telangiectasias may also be associated with clinical conditions such as rosacea, genetic syndromes, and collagen vascular diseases (Box 27-1).
BOX 27-1
Causes of Telangiectasias
Source: Adapted from Habif TP. Clinical Dermatology, 5th ed. St. Louis: Mosby; 2009.
Solar lentigines are small brown macules that increase in size and number with chronic sun exposure and are typically located around the periphery of the face (see Figure 27-8A later in the chapter). Postinflammatory hyperpigmentation can be seen in susceptible individuals, typically darker skin types (Fitzpatrick IV through VI), as brown macules arising at sites of previously inflamed acne lesions or sites of wound healing (see Figure 24-6A in Chapter 24, Skin Care Products). Melasma presents as hyperpigmented reticulated patches and brown macules, typically on the cheekbones, upper lip, forehead, and chin (see Figure 27-13A later in this chapter). It is frequently observed following a change in female hormonal status such as during pregnancy (chloasma) or after initiating use of oral contraceptives.
Cutaneous pigmented lesions may be located in the epidermis, dermis, or in both. Solar lentigines and ephelides (freckles) are located in the epidermis. Postinflammatory hyperpigmentation and melasma may be located in any of these levels. A Wood’s lamp can be used to determine the depth of melanin pigmentation in the skin.13 Epidermal pigmentation appears darker with more contrast against the background skin under Wood’s lamp illumination, whereas dermal pigmentation has less contrast.
Procedure Preparation
Laser Photorejuvenation: Steps and Principles
General Treatment Technique
Planning and Designing
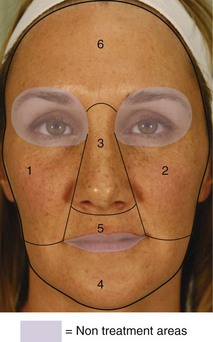
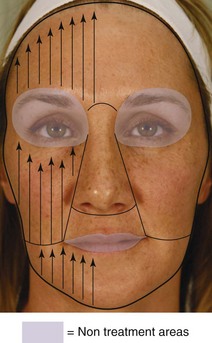
Figure 27-4 shows a recommended sequence for IPL treatment of the full face, starting with area 1 and progressing to area 6. The direction of IPL pulses is toward the provider as shown in Figure 27-5, with approximately 20% overlap of each pulse. The amount of pulse overlap may vary with different laser devices.
Safety Zone
The Laser Photorejuvenation Safety Zone for treatment of the face is shown in Figure 27-4. Laser treatments are performed outside of the ocular area: above the supraorbital ridge (above the eyebrows) and below the inferior orbital rim. When getting started with IPL treatments it is advisable to avoid the lips. As skill improves, providers may choose to treat the lip area for lesions such as lentigines.
Performing the Photorejuvenation Procedure
Results
Results of an initial photorejuvenation treatment with IPL for lentigines on the chest of a 36-year-old patient are shown in Figure 27-7. The patient’s chest is shown prior to treatment in (A) 1 week after treatment in (B), and 2 weeks after treatment in (C). Note in (B) the darkened and flaking appearance of the lentigines 1 week after treatment due to microcrust formation and the significant improvement in pigmentation at 2 weeks.
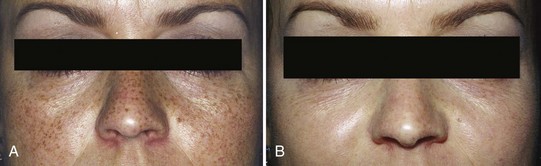
Figure 27-8 shows the results of photorejuvenation treatments for lentigines and mottled pigmentation on the face of a 75-year-old patient (A) before and (B) after a series of five IPL treatments (Starlux, Palomar).

FIGURE 27-8 Lentigines (A) before and (B) after photorejuvenation treatments with intense pulsed light.
(Copyright Rebecca Small, MD.)
Figure 27-9 shows the results of photorejuvenation treatments for lentigines and mottled pigmentation on the face (A) before and (B) after a Q-switched 532 nm treatment (Laser Peel™, Medlite HOYA ConBio).
Figure 27-10 shows the results of photorejuvenation treatments for solar lentigines and under-eye pigmentation for a 48-year-old patient (A) before and (B) after two Q-switched 532 nm treatments (RevLite, HOYA ConBio).
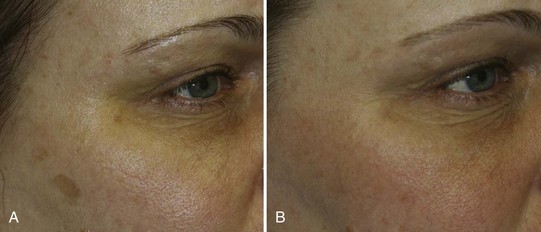
FIGURE 27-10 Hyperpigmentaion (A) before and (B) after photorejuvenation treatments with a Q-switched 532 nm laser.
(Copyright Rebecca Small, MD.)
Figure 27-11 shows the results of photorejuvenation treatments for solar lentigines on the hands of a 55-year-old patient (A) before and (B) after five IPL treatments (Starlux, Palomar).
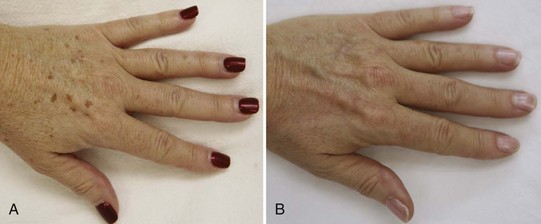
FIGURE 27-11 Hand lentigines (A) before and (B) after photorejuvenation treatments with intense pulsed light.
(Copyright Rebecca Small, MD.)
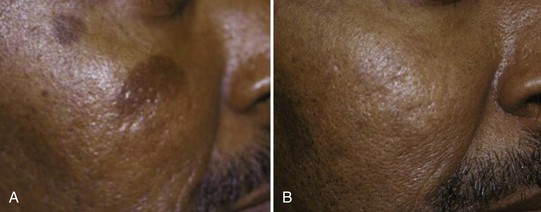
Figure 27-12 shows the results of photorejuvenation treatment for hyperpigmentation in a patient with Fitzpatrick VI skin type (A) before and (B) after Q-switched 1064 nm treatments (MedLite, HOYA ConBio).
Figure 27-13 shows the results of photorejuvenation treatment for melasma for a 41-year-old patient (A) before and (B) after Q-switched 1064 nm treatments (RevLite, HOYA ConBio).

FIGURE 27-13 Melasma (A) before and (B) after photorejuvenation treatments with a Q-switched 1064 nm laser
(Copyright Rebecca Small, MD.)
Figure 27-14 shows the results of photorejuvenation for nasal telangiectasias (A) before and (B) after 532 nm treatments (Gemini, Iridex).
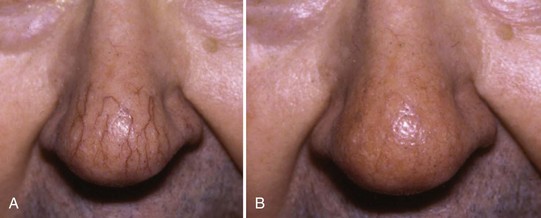
FIGURE 27-14 Nose telangiectasias (A) before and (B) after photorejuvenation treatments with a 532 nm laser.
(Courtesy of Iridex, Mount View, CA; B. Berger, MD, using laser.)
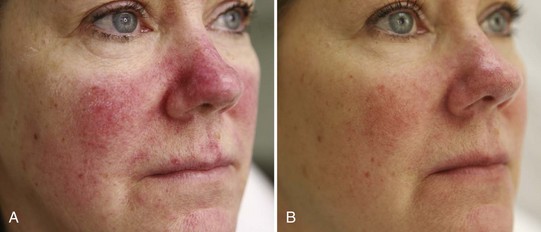
Figure 27-15 shows the results of photorejuvenation treatments for rosacea for a 57-year-old (A) before and (B) after a series of five IPL treatments (Starlux, Palomar).
Complications
Purpura is due to localized rupture of superficial blood vessels and can occur when aggressive treatment parameters are used with superficial vessels. Utilizing longer pulse widths and lower fluences will usually avoid this complication. There is no specific treatment for this and purpuric lesions usually resolve in 1 to 2 weeks. Figure 27-16 shows an example of purpura immediately after an IPL photorejuvenation treatment on the cheek.

FIGURE 27-16 Purpura of the cheek immediately after a photorejuvenation treatment with IPL for rosacea.
(Copyright Rebecca Small, MD.)
Pigmentary complications of hyperpigmentation and hypopigmentation are most commonly seen in darker Fitzpatrick skin types (IV)14 and in patients with a recent tan. These complications are more common with short pulse widths, high fluences, and poor epidermal cooling. Hyperpigmentation is usually transient (and rarely may be permanent), lasting in the order of months. The use of a lightening agent such as hydroquinone for 1 month prior to treatment and after treatment can reduce hyperpigmentation, particularly in darker skinned patients (see Chapter 24, Skin Care Products, for additional information). Hypopigmentation is a more significant complication. This may be temporary or permanent. Figure 27-17 shows stripes of hypopigmentation resulting from an overly aggressive IPL treatment for lentigines (not performed by the authors) on a patient with a darker skin type.
Postprocedure infections are rare with laser photorejuvenation treatments and require treatment specific to the infection. Infections such as herpes simplex and varicella zoster may be reactivated in the treatment area, and pretreatment prophylactic oral antiviral medication can reduce this risk (see the Procedure Preparation section above). Impetigo may occur, particularly with treatments around the mouth. Folliculitis may also occur, particularly after vigorous exercise, swimming or hot tub use immediately after treatments.
Current Developments
Some of the new fractional laser technologies used for nonablative skin resurfacing show promise as photorejuventation treatments15 (see Chapter 29, Skin Resurfacing with Ablative Lasers). The fractionated 1550 nm wavelength has been shown to reduce red vascularities16,17 and benign pigmented lesions18,19 as well as improve skin texture20 and scars (see Chapter 28, Wrinkle Reduction with Nonablative Lasers). Some newer devices combine chromophore-specific modalities with other modalities that are not chromophore specific to target pigmentation, vascularities, and skin texture, such as IPL with radio-frequency.21 Lasers with longer wavelengths, such as 940 nm, have been used for red vascular lesions and recently, a 980 nm wavelength laser22 has been used for targeting larger red facial vessels.
Photodynamic therapy (PDT) has also been used for photorejuvenation. PDT involves the use of a topical photosensitizing medication activated by light (usually LEDs or IPLs) . Commonly used photosensitizers include 5-aminolevulinic acid (ALA) and methyl ALA (mALA). ALA is selectively absorbed and concentrated in proliferating cells and pilosebaceous units where it is converted to protoporphyrin (PpIX). Upon activation with a light source, such as an IPL, laser (e.g., 585 nm), or LED, PpIX forms free radicals, which selectively destroy the target. PDT using ALA, activated by blue light, is currently FDA approved for treatment of nonhyperkeratotic actinic keratoses of the face and is also used off-label for photorejuvenation.23 PDT has a greater cost to the patient than laser alone, more downtime with erythema and crusting, and requires strict patient avoidance of ambient sunlight post-treatment for 48 hours, because sun exposure can lead to extended ALA activation and associated complications.
Financial Considerations
When covered by insurance, Box 27-2 lists the applicable ICD-9 codes for photorejuvenation procedures.
1. Small R. Aesthetic procedures introduction. In: Mayeaux E, editor. The Essential Guide to Primary Care Procedures. Philadelphia: Lippincott Williams & Wilkins; 2009:195-199.
2. Small R. Aesthetic procedures in office practice. Am Fam Physician. 2009;80(11):1231-1237.
3. Weiss RA, Weiss MA, Beasly KL. Rejuvenation of photoaged skin: 5 years results with intense pulsed light of the face, neck and chest. Dermatol Surg. 2002;28:1115-1119.
4. Bitter PH. Noninvasive rejuvenation of photodamaged skin using serial, full-face intense pulsed light treatments. Dermatol Surg. 2000;26:835-843.
5. Kligman DE, Zhen Y. Intense pulsed light treatment of photoaged facial skin. Dermatol Surg. 2004;30(8):1085-1090.
6. Small R. Laser photo rejuvenation. In: Mayeaux E, editor. The Essential Guide to Primary Care Procedures. Philadelphia: Lippincott Williams & Wilkins; 2009:249-264.
7. Uebelhoer NS, Bogle MA, Stewart B, et al. A split-face comparison study of pulsed 532-nm KTP laser and 595-nm pulsed dye laser in the treatment of facial telangiectasias and diffuse telangiectatic facial erythema. Dermatol Surg. 2007;33(4):441-448.
8. Kilmer SL. Diode laser treatment of pigmented lesions. Lasers Surg Med. 2000;12(Suppl):23.
9. Ross EV, Uebelhoer NS, Domankevitz Y. Use of a novel pulse dye laser for rapid single-pass purpura-free treatment of telangiectases. Dermatol Surg. 2007;33(12):1466-1469.
10. Ross EV, Smirnov M, Pankratov M. Intense pulsed light and laser treatment of facial telangiectasias and dyspigmentation: some theoretical and practical comparisons. Dermatol Surg. 2005;31(9 Pt 2):1188-1198.
11. Kilmer SL, Wheeland RG, Goldberg DJ, et al. Treatment of epidermal pigmented lesions with the frequency-doubled Q-switched Nd:YAG laser. A controlled, single-impact, dose-response, multicenter trial. Arch Dermatol. 1994;130(12):1515-1519.
12. Goldman MP, Bennett RG. Treatment of telangiectasia: a review. J Am Acad Dermatol. 1987;17(2 Pt 1):167-182.
13. Gilchrest BA, Fitzpatrick TB, Anderson RR, et al. Localization of melanin pigmentation in the skin with Wood’s lamp. Br J Dermatol. 1977;96(3):245-248.
14. Kono T, Manstein D, Chan HH, et al. Q-switched ruby versus long-pulsed dye laser delivered with compression for treatment of facial lentigines in Asians. Lasers Surg Med. 2006;38:94-97.
15. Tierney EP, Kouba DJ, Hanke CW. Review of fractional photothermolysis: treatment indications and efficacy. Dermatol Surg. 2009;35(10):1445-1461.
16. Glaich AS, Goldberg LH, Dai T, et al. Fractional photothermolysis for the treatment of telangiectatic matting: a case report. J Cutan Laser Ther. 2007;9:101-103.
17. Behroozan DS, Goldberg LH, Glaich AS, et al. Fractional photothermolysis for treatment of poikiloderma of Civatte. Dermatol Surg. 2006;32:298-301.
18. Wanner M, Tanzi EL, Alster TS. Fractional photothermolysis treatment of facial and non-facial cutaneous photodamage with the 1,550-nm erbium-doped fiber laser. Dermatol Surg. 2007;33:23-28.
19. Jih MH, Goldberg LH, Kimyai-Asadi A. Fractional photothermolysis for photoaging hands. Dermatol Surg. 2008;34:73-78.
20. Manstein D, Herron GS, Sink RK. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34:426-438.
21. Bitter P. Report of a new technique for enhanced non-invasive skin rejuvenation using a dual mode, pulsed light and radiofrequency energy source: selective radio-thermolysis. J Cosm Dermatol. 2002;1:142-145.
22. Dudelzak J, Hussain M, Goldberg DJ. Vascular-specific laser wavelength for the treatment of facial telangiectasias. J Drugs Dermatol. 2009;8(3):227-229.
23. Dover JS, Bhatia AC, Stewart B, et al. Topical 5-aminolevulinic acid combined with intense pulsed light in the treatment of photoaging. Arch Dermatol. 2005;141(10):1247-1252.
Small R. Photo rejuvenation. In: Small R, editor. A Practical Guide to Cosmetic Lasers. Philadelphia: Lippincott Williams & Wilkins, 2012.
Van Aardt R. Lasers and pulsed-light devices: photofacial rejuvenation. In Pfenninger JL, Fowler GC, editors: Pfenninger and Fowler’s Procedures for Primary Care, 3rd ed, Philadelphia: Mosby/Elsevier, 2011.



 % hydrocortisone cream two times per day for 3 to 4 days or until redness resolves are recommended. Pigmented lesions typically continue to darken 1 to 2 days after treatment, forming microcrusts that flake off over 1 to 2 weeks, exposing lightened or resolved lesions. Vascular lesions that have turned grayish or darkened at the time of treatment usually fade over 1 to 2 weeks. Patients are instructed to contact their provider if erythema persists for more than 5 days because postinflammatory hyperpigmentation (PIH) can occur with prolonged erythema. Patients are also instructed to avoid intense, direct sun exposure and use a full-spectrum sunscreen (SPF 30 with zinc or titanium) daily for 4 weeks after treatment to help minimize the risk of undesired pigmentary changes.
% hydrocortisone cream two times per day for 3 to 4 days or until redness resolves are recommended. Pigmented lesions typically continue to darken 1 to 2 days after treatment, forming microcrusts that flake off over 1 to 2 weeks, exposing lightened or resolved lesions. Vascular lesions that have turned grayish or darkened at the time of treatment usually fade over 1 to 2 weeks. Patients are instructed to contact their provider if erythema persists for more than 5 days because postinflammatory hyperpigmentation (PIH) can occur with prolonged erythema. Patients are also instructed to avoid intense, direct sun exposure and use a full-spectrum sunscreen (SPF 30 with zinc or titanium) daily for 4 weeks after treatment to help minimize the risk of undesired pigmentary changes.





